Rheumatoid arthritis flare up – Rheumatoid arthritis flare-up is a painful and disruptive experience for those living with the condition. It’s a temporary worsening of symptoms, often triggered by various factors, and understanding these triggers is key to managing them effectively. This guide explores the complexities of rheumatoid arthritis flare-ups, from defining the symptoms to strategies for early detection and management.
We’ll delve into the various factors contributing to flare-ups, including genetic predisposition, environmental influences, and lifestyle choices. Understanding these aspects allows for a more personalized approach to managing flare-ups. Additionally, we’ll explore medical interventions, lifestyle adjustments, and crucial monitoring techniques to provide a comprehensive overview of the condition.
Defining a Flare-Up
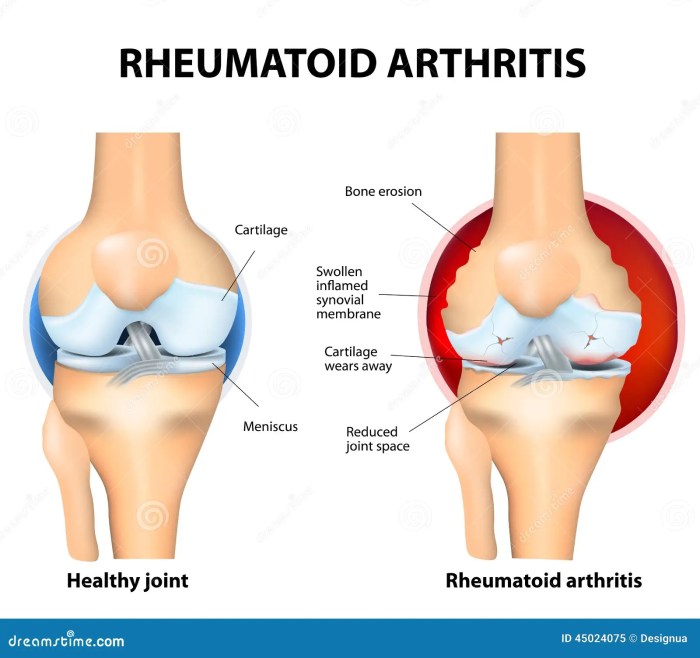
A rheumatoid arthritis flare-up is a period of increased inflammation and pain, characterized by a worsening of symptoms compared to a stable period. These episodes can range in severity and duration, impacting daily life and requiring adjustments to treatment plans. Understanding what constitutes a flare-up is crucial for effective self-management and communication with healthcare professionals.Flare-ups are distinct from the overall progression of rheumatoid arthritis.
While rheumatoid arthritis is a chronic condition with periods of remission and activity, a flare-up represents a temporary intensification of symptoms. The underlying disease process continues, but the symptoms become more pronounced during a flare. This distinction is important for distinguishing the temporary exacerbation from the long-term progression of the disease.
Symptoms of a Flare-Up
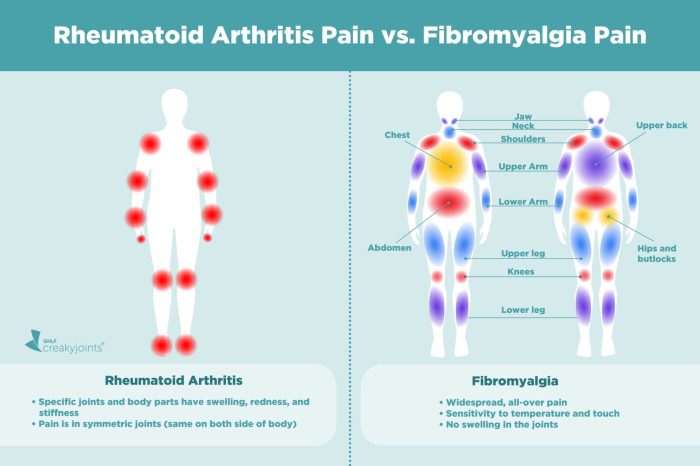
Flare-ups are typically characterized by a noticeable increase in the severity of pre-existing rheumatoid arthritis symptoms. These symptoms can vary from person to person, but some commonalities exist. Differentiating between a flare-up and other conditions, like a simple infection, requires careful attention to the pattern of symptoms and their duration.
Comparison to Other Conditions
Differentiating a rheumatoid arthritis flare-up from other conditions is vital for accurate diagnosis and appropriate treatment. Similar symptoms can occur in conditions such as infections, injuries, or even other autoimmune diseases. The presence of other symptoms, such as fever, specific joint pain locations, or recent infections, can help in differentiating. A thorough medical evaluation by a healthcare professional is essential for accurate diagnosis.
Symptom Table
| Symptom | Description | Severity Level |
|---|---|---|
| Joint Pain | Aching, throbbing, or stabbing pain in one or more affected joints. | Mild: Slight discomfort; Moderate: Significant pain interfering with daily tasks; Severe: Excruciating pain, inability to move joints. |
| Joint Swelling | Inflammation of the affected joints, causing them to feel warm, tender, and swollen. | Mild: Slight swelling; Moderate: Noticeable swelling; Severe: Significant swelling, potentially causing deformity. |
| Stiffness | Limited range of motion in affected joints, particularly noticeable in the morning or after periods of inactivity. | Mild: Slight stiffness; Moderate: Significant stiffness, limiting mobility; Severe: Extreme stiffness, making it difficult to perform basic tasks. |
| Fatigue | Extreme tiredness, often more pronounced during flare-ups. | Mild: Slight tiredness; Moderate: Significant fatigue impacting daily activities; Severe: Extreme exhaustion, inability to perform any tasks. |
| Fever | Elevated body temperature, often accompanied by chills and sweats. | Mild: Slightly elevated temperature; Moderate: Elevated temperature, noticeable discomfort; Severe: High fever, potentially accompanied by other systemic symptoms. |
| Loss of Function | Inability to perform daily activities due to pain and stiffness. | Mild: Slight limitations in daily tasks; Moderate: Significant limitations; Severe: Complete loss of function in affected joints. |
Triggers and Risk Factors
Rheumatoid arthritis (RA) flare-ups can be unpredictable and debilitating. Understanding the factors that contribute to these episodes is crucial for effective management. This knowledge empowers individuals to proactively address potential triggers and reduce the frequency and severity of flare-ups. Identifying these triggers allows for personalized strategies to minimize the impact of RA on daily life.Identifying the specific triggers that initiate or exacerbate RA flare-ups is often a personalized process.
While a precise cause isn’t always evident, various factors can play a role. This exploration of potential triggers delves into genetics, environmental influences, and lifestyle choices, ultimately aiming to equip readers with insights into proactive management.
Potential Triggers for RA Flare-Ups
Several factors can trigger or worsen rheumatoid arthritis flare-ups. Recognizing these triggers is essential for developing personalized strategies to manage symptoms effectively. Identifying specific triggers allows individuals to proactively address potential risk factors and minimize the impact of RA.
Genetic Predisposition
Genetic factors play a significant role in RA susceptibility. Individuals with a family history of RA are more likely to develop the condition. This genetic predisposition doesn’t guarantee a flare-up, but it increases the risk. The specific genes involved in RA development are complex and not fully understood, but ongoing research continues to shed light on these connections.
Environmental Factors
Environmental factors can also contribute to RA flare-ups. Exposure to certain infections, such as Epstein-Barr virus, has been linked to RA onset and flare-ups. Environmental pollutants, like certain chemicals, may also contribute to inflammation. While not fully understood, these environmental interactions contribute to the overall RA experience.
Lifestyle Choices
Lifestyle choices are vital in managing RA. Poor sleep quality can increase inflammation and trigger flare-ups. Stress, lack of exercise, and an unhealthy diet can also negatively influence the disease course. Making healthy lifestyle choices is important to reduce the risk of flare-ups.
Examples of Common Triggers and their Impact
Infections, such as a cold or the flu, can sometimes trigger or exacerbate RA symptoms. Stressful life events, such as job loss or relationship problems, may also contribute to flare-ups. These factors can increase inflammation in the body, leading to increased joint pain and stiffness.
Comparison of Trigger Types and Symptom Severity
| Trigger Type | Description | Symptom Severity (1-5, 1 being mild, 5 being severe) |
|---|---|---|
| Infections (e.g., colds, flu) | Viral or bacterial infections can trigger inflammatory responses. | 3-4 |
| Stressful life events | Major life changes or emotional distress can worsen RA symptoms. | 2-4 |
| Poor sleep quality | Insufficient or poor quality sleep can increase inflammation. | 2-3 |
| Lack of exercise | Sedentary lifestyle can exacerbate joint stiffness and pain. | 2-3 |
| Unhealthy diet | Poor dietary choices can contribute to inflammation. | 2-3 |
Early Detection and Management
Early detection of rheumatoid arthritis (RA) flare-ups is crucial for minimizing their impact on daily life and preventing long-term complications. Prompt intervention can help reduce inflammation, pain, and joint damage. A proactive approach allows individuals to maintain a better quality of life and adhere to their treatment plan effectively.Understanding the subtle warning signs and knowing the diagnostic methods can empower individuals to take control of their RA management.
This section will detail how to recognize early signs of a flare-up, explore common diagnostic tools, and provide a step-by-step approach to managing a flare-up effectively.
Importance of Early Detection
Early detection of RA flare-ups allows for timely intervention, mitigating the severity of symptoms and preventing lasting joint damage. By addressing the flare-up promptly, individuals can avoid the progressive deterioration of joint function and maintain a better quality of life. This proactive approach helps in preventing long-term complications and promotes adherence to the treatment plan.
Common Diagnostic Methods
Several methods are used to identify and diagnose RA flare-ups. These include physical examination, blood tests, and imaging studies. A physical examination by a rheumatologist assesses joint swelling, tenderness, and range of motion. Blood tests, such as measuring inflammatory markers (e.g., ESR, CRP), can indicate the presence of inflammation, even before noticeable physical changes. Imaging techniques, such as X-rays and MRI scans, are used to visualize joint damage and evaluate the extent of inflammation.
Ugh, another rheumatoid arthritis flare-up. The pain is relentless, making even the simplest tasks feel impossible. It’s frustrating to deal with these unpredictable episodes, especially when you’re trying to maintain a healthy lifestyle. While researching alternative approaches, I stumbled upon an interesting overview of familial dysautonomia, an overview of familial dysautonomia , which highlights the complex interplay of genetic and environmental factors.
Hopefully, understanding similar neurological conditions can lead to insights that might help manage my own flare-ups. It’s definitely a long road ahead, but I’m determined to find some relief.
Recognizing Early Warning Signs
Recognizing early warning signs of an impending flare-up is vital for effective management. These signs can vary from person to person, but common indicators include increased fatigue, stiffness, and pain in affected joints. Changes in the affected joints, like swelling, warmth, or redness, should be noted. A sudden increase in morning stiffness or a change in the usual pain patterns can be significant indicators.
Monitoring these changes, in combination with other factors like stress levels and sleep patterns, can aid in anticipating flare-ups.
Managing a Flare-Up: A Step-by-Step Procedure
Managing a flare-up involves a structured approach. The first step involves contacting a healthcare professional for guidance and support. Next, take prescribed medications as directed. This might include nonsteroidal anti-inflammatory drugs (NSAIDs) or disease-modifying antirheumatic drugs (DMARDs). If pain or stiffness increases significantly, consider over-the-counter pain relievers, but always consult a physician first.
Ugh, another rheumatoid arthritis flare-up. The pain is relentless, and I’m feeling utterly drained. Navigating these flare-ups is tough, but I’ve found that managing digestive issues like IBS and diverticulosis simultaneously can be even trickier. Fortunately, there’s helpful information out there on how to best handle this combination of conditions, which can really impact your overall well-being.
Check out this article for tips on managing both IBS and diverticulosis , which can be really beneficial for anyone facing similar challenges. Hopefully, these strategies will help me get through this flare-up more comfortably.
Prioritizing rest and gentle exercises is essential to reduce stress on the affected joints. Applying heat or cold packs to the affected areas can also help manage pain and inflammation. Maintaining a healthy lifestyle, including a balanced diet and regular exercise (when possible), can support overall well-being and aid in managing symptoms.
Table of Common Early Detection Methods
| Detection Method | Effectiveness | Limitations |
|---|---|---|
| Physical Examination | Useful for identifying initial signs like swelling and tenderness. | May not detect subtle inflammation. Subjectivity in assessment can vary between healthcare professionals. |
| Blood Tests (ESR, CRP) | Reliable indicators of inflammation. Can detect subtle changes before physical signs appear. | Results can be influenced by other factors like infections or other medical conditions. Results may not always correlate directly with the severity of the flare-up. |
| Imaging Studies (X-rays, MRI) | Visualizes joint damage and inflammation. | Can be expensive and may not be necessary for every flare-up. May not detect early-stage inflammation as effectively as blood tests. |
Medical Interventions and Therapies
Managing a rheumatoid arthritis (RA) flare-up requires a multifaceted approach combining various medical interventions and therapies. A key aspect is understanding that RA treatment is not a one-size-fits-all solution. Individualized plans tailored to the specific needs and characteristics of each patient are essential for effective management.Effective treatment strategies aim to reduce inflammation, alleviate pain, and maintain joint function.
This often involves a combination of medications, physical therapy, and patient self-management techniques. The goal is not just to suppress symptoms during a flare, but also to prevent future flare-ups and preserve long-term joint health.
Different Medical Interventions
Various medical interventions are employed to address the inflammatory processes and pain associated with RA flare-ups. These interventions encompass a range of approaches, from medications to lifestyle modifications. A comprehensive strategy often involves a collaborative effort between the patient and their healthcare team.
Types of Medications for Flare-Up Management
A variety of medications are used to manage RA flare-ups. These are typically categorized based on their mechanism of action. Early intervention with appropriate medications is crucial for controlling inflammation and preventing long-term joint damage.
- Disease-modifying antirheumatic drugs (DMARDs): These medications are designed to slow or stop the progression of the disease and are often the cornerstone of RA treatment. They work by suppressing the immune system’s inflammatory response. Examples include methotrexate, sulfasalazine, and leflunomide. DMARDs may take several weeks or months to show full effect.
- Corticosteroids: These powerful anti-inflammatory medications are often used to quickly reduce inflammation and pain during a flare-up. They can be administered orally, intravenously, or topically. However, long-term use of corticosteroids is not recommended due to potential side effects.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications are frequently used to alleviate pain and reduce inflammation. They are often the first line of treatment for mild to moderate RA symptoms. Examples include ibuprofen and naproxen.
- Biologics and targeted synthetic DMARDs (tsDMARDs): These newer medications are specifically designed to target certain components of the immune system involved in RA. They are often used when other treatments have not been effective. Examples include TNF inhibitors (e.g., etanercept, adalimumab) and JAK inhibitors (e.g., tofacitinib, baricitinib).
Role of Physical Therapy and Exercise
Physical therapy plays a vital role in managing RA flare-ups. Therapeutic exercises are crucial for maintaining joint mobility, strength, and function. Regular exercise, tailored to the patient’s capabilities and limitations, can help reduce pain, improve overall fitness, and enhance the effectiveness of medication. It is crucial to consult a physical therapist for an individualized exercise program.
Importance of Patient Self-Management
Effective self-management is critical in controlling RA flare-ups. Patients can actively participate in their care by closely monitoring their symptoms, adhering to their treatment plan, and adopting healthy lifestyle habits. This includes managing stress, maintaining a balanced diet, and engaging in regular physical activity. This proactive approach empowers patients to take control of their health and improve their overall well-being.
Treatment Options Summary
| Treatment Option | Potential Side Effects |
|---|---|
| Disease-modifying antirheumatic drugs (DMARDs) | Gastrointestinal upset, liver problems, mouth sores, and potential for allergic reactions. |
| Corticosteroids | Weight gain, osteoporosis, increased risk of infections, and mood changes. |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Gastrointestinal issues, kidney problems, and potential for allergic reactions. |
| Biologics and targeted synthetic DMARDs (tsDMARDs) | Increased risk of infections, allergic reactions, and other serious side effects. |
Lifestyle Adjustments and Support
Managing rheumatoid arthritis (RA) flare-ups effectively goes beyond medication. Lifestyle choices play a crucial role in controlling symptoms and preventing exacerbations. By making conscious adjustments in diet, stress management, sleep, and self-care, individuals with RA can significantly improve their quality of life and reduce the frequency and severity of flare-ups.
Balanced Diet for Mitigation
A well-balanced diet is essential for managing RA. Nutrients impact inflammation levels in the body, and certain foods can exacerbate symptoms. A diet rich in anti-inflammatory foods can help reduce pain and swelling associated with RA flares.
- Fruits and vegetables are excellent sources of vitamins, minerals, and antioxidants that combat inflammation. Aim for a variety of colors, ensuring a diverse intake of nutrients.
- Lean proteins, such as fish, poultry, and beans, provide essential amino acids for tissue repair and maintenance. Limit red meat and processed meats due to their potential inflammatory effects.
- Healthy fats, found in avocados, nuts, and olive oil, contribute to overall well-being and can reduce inflammation. Minimize intake of saturated and trans fats.
- Whole grains, like brown rice and quinoa, offer complex carbohydrates and fiber for sustained energy levels and digestive health. Limit refined grains, which may increase inflammation.
Stress Management Techniques
Chronic stress can significantly worsen RA symptoms. Implementing stress-reducing techniques can help manage flare-ups and improve overall well-being.
- Mindfulness and meditation practices help calm the mind and body, reducing the physiological response to stress. Regular mindfulness exercises can lessen stress-induced inflammation.
- Yoga and tai chi combine physical postures and breathing techniques, promoting relaxation and flexibility. These practices can enhance physical function and mental well-being, reducing the risk of flare-ups.
- Physical activity, such as walking, swimming, or cycling, can help reduce stress hormones and improve mood. Moderate exercise can improve overall health and potentially decrease the frequency of flare-ups.
- Spending time in nature, listening to calming music, or engaging in hobbies can also contribute to stress reduction. Engaging in enjoyable activities can provide a welcome distraction from stressful situations.
Regular Sleep Patterns
Adequate sleep is crucial for the body’s restorative processes, which are vital in managing RA. Consistent sleep patterns can significantly impact the severity and frequency of RA flare-ups.
- Establishing a regular sleep schedule, going to bed and waking up at the same time each day, even on weekends, helps regulate the body’s natural sleep-wake cycle.
- Creating a relaxing bedtime routine, such as taking a warm bath or reading, can signal to the body that it’s time to wind down and prepare for sleep.
- Ensuring a comfortable sleep environment, including a dark, quiet, and cool room, can promote better sleep quality.
- Limiting caffeine and alcohol intake before bed can reduce disruptions to sleep patterns. Avoiding these stimulants can help regulate sleep quality.
Personalized Self-Care Plan
Developing a personalized self-care plan is essential for managing RA flare-ups effectively. This plan should consider individual needs and preferences.
- Identify triggers: Recognizing specific factors that tend to trigger flare-ups allows for proactive management and avoidance.
- Prioritize activities: Balancing rest and activity is crucial. Scheduling rest periods throughout the day can help prevent fatigue and allow the body to recover.
- Track symptoms: Keeping a journal of symptoms, triggers, and responses to different treatments can help identify patterns and tailor management strategies.
- Seek support: Connecting with support groups or other individuals with RA can provide valuable insights, encouragement, and practical advice.
Monitoring and Tracking Progress
Staying on top of your rheumatoid arthritis (RA) journey involves meticulous monitoring of flare-ups and your response to treatment. This proactive approach allows you and your healthcare team to adjust strategies as needed, ensuring optimal management of your condition. Understanding how to track your symptoms and progress is crucial for successful RA management.Effective monitoring is a collaborative effort between you and your doctor.
By carefully documenting your experiences, you provide valuable insights that help tailor your treatment plan for maximum effectiveness. Accurate record-keeping allows for quicker identification of trends, potential triggers, and the efficacy of different interventions.
Methods for Monitoring Flare-Up Severity
Several methods can be used to track the severity of a flare-up. These include subjective assessments like pain levels, fatigue, and stiffness, alongside objective measurements such as joint swelling and range of motion. Combining these methods provides a more comprehensive picture of your condition.
Tools and Technologies for Symptom Tracking
Numerous tools and technologies can facilitate symptom tracking. Dedicated apps designed for chronic conditions offer structured symptom logging, reminders for medication, and the ability to graph trends over time. Many of these apps also allow for sharing data with healthcare providers. Furthermore, wearable devices capable of measuring activity levels, sleep patterns, and heart rate variability can provide additional data points.
Importance of Regular Check-ups with Healthcare Professionals
Regular check-ups with your rheumatologist or other healthcare provider are essential for monitoring your RA. These appointments allow for physical assessments, blood tests, and discussions about your progress, enabling adjustments to your treatment plan as needed. They also offer an opportunity to address any concerns or questions you might have.
Ugh, another rheumatoid arthritis flare-up. The pain is relentless, making even the simplest tasks feel impossible. Sometimes, doctors need to see exactly what’s going on inside my joints, and that’s where an MRI comes in handy. Learning more about what an MRI is and what it does can be really helpful, which you can find out more about here.
Hopefully, this diagnostic tool will help pinpoint the cause of the flare-up and get me back on track to feeling better.
Examples of Ways to Document and Track Flare-Up Information
Maintain a detailed journal that includes the date, time, and nature of symptoms. Note the severity of pain, stiffness, and swelling on a scale (e.g., 0-10). Include any triggers you suspect might have contributed to the flare-up. Also, record any changes in your medications, lifestyle, or environmental factors. Photographs of affected joints can be helpful for documenting changes in swelling and inflammation.
Symptom Tracking Methods: A Comparative Table
| Method | Description | Pros | Cons |
|---|---|---|---|
| Symptom Diary | A daily log of symptoms, including pain, stiffness, fatigue, and other relevant details. | Simple, cost-effective, and allows for detailed personal observations. | Subjective data; requires discipline to maintain consistently. |
| Symptom Tracking Apps | Mobile applications designed to track symptoms, medication, and other relevant data. | Convenient, provides graphs and trends, often integrates with healthcare providers. | Requires a smartphone or tablet; may have data privacy concerns. |
| Wearable Devices | Devices that monitor activity levels, sleep, and other physiological indicators. | Objective data, potential for early detection of changes. | Limited insight into specific symptoms, potential for data inaccuracies. |
| Physical Examinations | Assessments by healthcare providers to evaluate joint swelling, range of motion, and overall condition. | Provides objective measurements and professional insights. | Requires appointments and time commitment. |
Illustrative Cases and Examples
Understanding rheumatoid arthritis (RA) flare-ups requires more than just statistics. Real-life experiences offer crucial insights into the challenges and triumphs of managing this chronic condition. Each individual’s journey is unique, shaped by diverse factors like genetics, environmental triggers, and treatment responses. This section delves into illustrative case studies, highlighting the variability in RA flare-up experiences and successful management strategies.Navigating a RA flare-up is a multifaceted experience.
Symptoms can range from mild discomfort to debilitating pain, impacting daily activities and emotional well-being. The severity and duration of flare-ups can vary significantly, making a standardized approach challenging.
Different Experiences and Management Strategies, Rheumatoid arthritis flare up
Diverse individual experiences underscore the importance of personalized care in managing RA flare-ups. The following case studies showcase the range of experiences and successful strategies for managing flare-ups.
“I noticed my usual stiffness was much worse, and I developed a fever and intense joint pain in my hands and feet. My doctor prescribed a higher dose of methotrexate, and I also started using heat packs and gentle exercises. After a week, the pain subsided significantly. The key for me is proactive management and open communication with my rheumatologist.”
Maria, 48, diagnosed with RA for 10 years.
“My flare-ups are often triggered by stress. I’ve learned to identify my stressors and implement relaxation techniques like meditation and deep breathing. This, combined with my prescribed biologics, helps me keep the flare-ups under control. It’s about finding a balance between managing the condition and maintaining a fulfilling life.”
David, 32, diagnosed with RA for 2 years.
“I’m a single mother of two young children. A flare-up significantly impacts my ability to care for them. I’ve learned to prioritize tasks and ask for support from my family and friends. My rheumatologist has been instrumental in finding a treatment plan that minimizes disruption to my daily life.”
Sarah, 35, diagnosed with RA for 5 years.
Impact on Daily Life
Flare-ups in rheumatoid arthritis can profoundly impact daily life. The varying degrees of pain, fatigue, and stiffness can make even basic tasks challenging. Successful management requires a multifaceted approach, encompassing medical interventions, lifestyle adjustments, and emotional support.
- Physical limitations: Difficulties with mobility, performing household chores, and engaging in hobbies are common during flare-ups.
- Emotional toll: Flare-ups can cause anxiety, frustration, and feelings of isolation, requiring emotional coping mechanisms and support systems.
- Social implications: Reduced participation in social activities and maintaining relationships can be consequences of flare-ups.
- Occupational challenges: Flare-ups may lead to missed work or reduced productivity, impacting employment and financial stability.
Conclusive Thoughts: Rheumatoid Arthritis Flare Up
In conclusion, managing rheumatoid arthritis flare-ups requires a multifaceted approach. Early detection and prompt medical intervention are crucial, along with understanding personal triggers and implementing effective lifestyle adjustments. This comprehensive guide provides a framework for understanding, managing, and living with rheumatoid arthritis flare-ups. Remember, consistent monitoring, open communication with healthcare professionals, and personalized strategies are key to effectively navigating these challenges.










