What causes death in people with alzheimers disease – What causes death in people with Alzheimer’s disease? This complex question delves into the multifaceted ways this progressive neurodegenerative disorder impacts the body. From the initial neurological damage to the systemic consequences and secondary complications, Alzheimer’s can lead to a variety of factors contributing to the eventual demise of a patient.
This exploration will delve into the intricate interplay of neuropathological changes, systemic effects, nutritional deficiencies, infections, fluid imbalances, medication interactions, and physical complications. Understanding these interconnected factors is crucial for improving care and potentially altering the course of the disease.
Underlying Pathophysiology
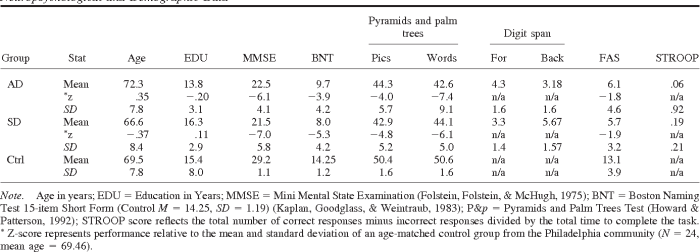
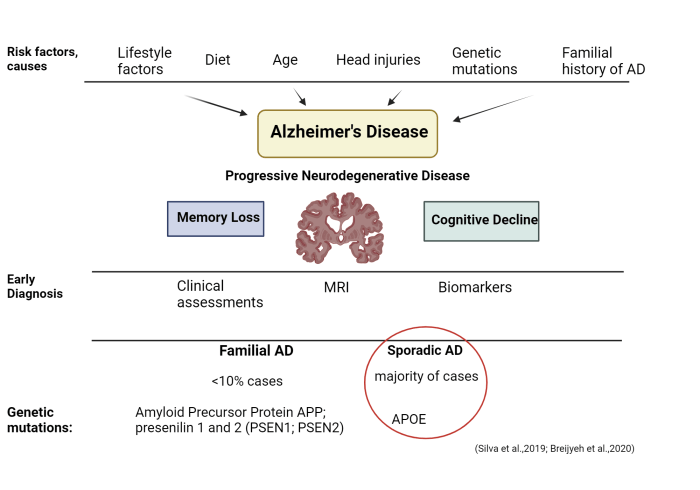
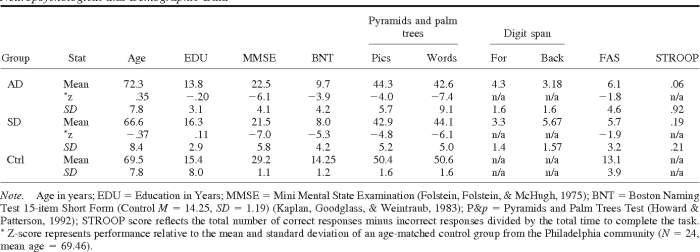
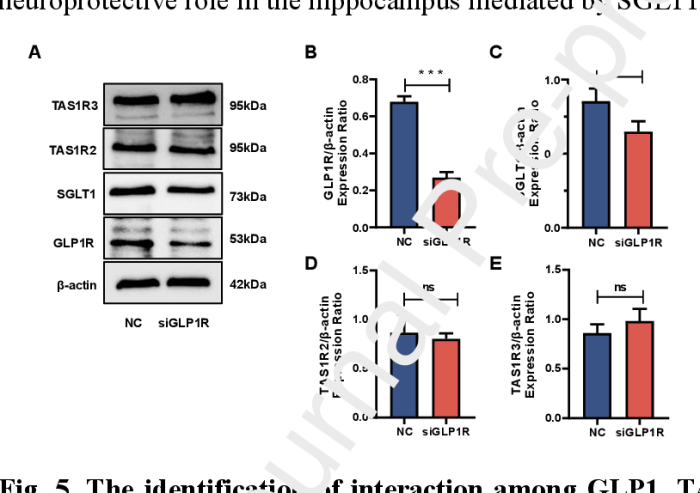
Alzheimer’s disease, a progressive neurodegenerative disorder, is characterized by a complex interplay of pathological changes in the brain. These changes disrupt normal neuronal function and communication, leading to the cognitive decline and behavioral symptoms that define the disease. Understanding these underlying mechanisms is crucial for developing effective treatments and interventions.The hallmark neuropathological features of Alzheimer’s disease are amyloid plaques and neurofibrillary tangles.
These abnormal protein deposits accumulate in the brain, interfering with neuronal function and ultimately contributing to cell death. The precise sequence and interaction of these events remain a subject of ongoing research.
Amyloid Plaques
Amyloid plaques are extracellular deposits primarily composed of beta-amyloid protein. This protein, derived from the amyloid precursor protein (APP), is normally broken down and cleared from the brain. In Alzheimer’s disease, however, an abnormal processing pathway leads to the accumulation of misfolded beta-amyloid peptides, which aggregate to form insoluble plaques. These plaques disrupt neuronal communication by interfering with synaptic function and promoting inflammation.
The presence of amyloid plaques is often considered an early event in the disease process.
Neurofibrillary Tangles
Neurofibrillary tangles are intracellular aggregates of hyperphosphorylated tau protein. Tau normally stabilizes microtubules, which are essential components of the neuronal cytoskeleton. In Alzheimer’s disease, tau protein becomes hyperphosphorylated, causing it to detach from microtubules and aggregate into tangles. These tangles disrupt the transport of essential nutrients and molecules within the neuron, leading to neuronal dysfunction and death.
The formation of neurofibrillary tangles is closely associated with the later stages of the disease.
Impact on Neuronal Function and Communication
The accumulation of amyloid plaques and neurofibrillary tangles significantly impacts neuronal function and communication. These abnormal protein deposits disrupt synaptic transmission, interfere with signal transduction pathways, and promote neuroinflammation. This cascade of events ultimately leads to neuronal loss, synaptic dysfunction, and the cognitive impairments characteristic of Alzheimer’s disease. These impairments can vary greatly, depending on the specific brain regions affected.
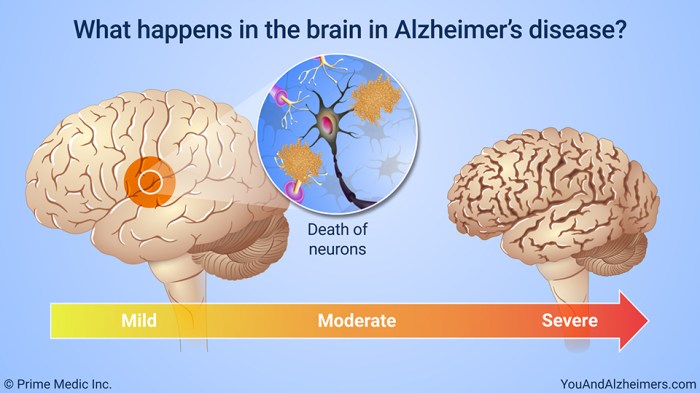
Brain Regions Affected and Symptoms
Different brain regions are affected at varying stages of the disease, leading to a specific pattern of cognitive decline. The hippocampus, crucial for memory formation, is typically one of the first regions affected, explaining the early memory loss often observed in Alzheimer’s disease. The cortex, involved in higher-order cognitive functions like language and executive function, is also progressively affected, contributing to the later stages of the disease.
The frontal lobes are affected, impacting personality and behavior. The temporal lobe is also involved, affecting language and comprehension.
Types of Alzheimer’s Disease
| Type | Description | Key Features |
|---|---|---|
| Sporadic Alzheimer’s Disease | The most common form, accounting for the vast majority of cases. | No clear genetic predisposition, typically diagnosed in later life. |
| Familial Alzheimer’s Disease | Characterized by early-onset of symptoms, often before age 65. | Associated with specific genetic mutations in genes like APP, PSEN1, and PSEN2. |
| Late-onset Alzheimer’s Disease | This form typically manifests in individuals over the age of 65. | While a genetic component may be present, it is often not as strongly linked to specific genes as in familial cases. |
Systemic Effects and Complications
Alzheimer’s disease, while primarily affecting the brain, exerts profound systemic effects that significantly impact the overall health and well-being of individuals. These systemic complications often contribute significantly to the progressive decline and ultimately, the mortality associated with the disease. Understanding these effects is crucial for comprehensive patient care and management.
Impact on Organ Systems
The progressive nature of Alzheimer’s disease leads to disruptions in the communication and coordination between the brain and various organ systems. This disrupts the body’s natural homeostasis, increasing vulnerability to infections and other complications. For instance, the brain’s reduced ability to regulate essential bodily functions can impact the cardiovascular, respiratory, and gastrointestinal systems.
Common Complications
Several complications frequently arise as Alzheimer’s disease progresses. These complications can range from infections to malnutrition and even pressure sores. Their impact on the patient’s overall health and well-being is often substantial.
- Infections: Weakened immune responses are common in Alzheimer’s patients, making them more susceptible to infections like pneumonia, urinary tract infections, and other systemic illnesses. The impaired cognitive function often hinders proper hygiene practices, increasing the risk of infection. This can be particularly challenging in individuals requiring assistance with daily care, as they may not be able to communicate their needs effectively.
- Malnutrition and Dehydration: Cognitive decline often leads to difficulties with eating and drinking. Individuals with Alzheimer’s may forget to eat or drink, leading to malnutrition and dehydration. This can further compromise the body’s ability to fight off infections and can lead to a significant decline in overall health.
- Pressure Sores: Immobility and reduced awareness of body positioning can lead to pressure sores (decubitus ulcers). These sores are a significant concern as they can become infected and significantly impair the patient’s health, requiring extensive treatment and potentially leading to serious complications, like sepsis.
- Urinary Incontinence: Neurological changes associated with Alzheimer’s disease can affect bladder control, leading to urinary incontinence. This can contribute to urinary tract infections (UTIs), further weakening the immune system and causing discomfort and distress for the patient and caregivers. The frequency and severity of UTIs increase with disease progression.
- Cardiovascular Issues: There’s a correlation between Alzheimer’s and cardiovascular problems, including an increased risk of heart failure. This can be attributed to the brain’s reduced ability to regulate the cardiovascular system, leading to irregularities in blood pressure and heart rate.
Mechanisms of Mortality
The complications of Alzheimer’s disease often contribute to mortality in multiple ways. Infections, for instance, overwhelm the body’s defenses, leading to sepsis and organ failure. Malnutrition and dehydration compromise the body’s ability to maintain essential functions, increasing the risk of numerous health problems. Pressure sores, when infected, can also lead to serious complications, including sepsis and even death.
Stages of Disease Progression and Related Complications
| Stage of Disease Progression | Common Complications | Mechanism of Contribution to Mortality |
|---|---|---|
| Early Stage | Mild cognitive impairment, subtle memory loss, difficulty with complex tasks | Increased risk of falls and injuries, reduced ability to manage daily needs, potentially leading to malnutrition and dehydration. |
| Middle Stage | Increased confusion, significant memory loss, difficulty with communication, behavioral changes | Increased risk of infections (pneumonia, UTIs), difficulties with nutrition, increased vulnerability to pressure sores, and complications from immobility. |
| Late Stage | Loss of motor skills, inability to communicate, complete dependence on caregivers, severe cognitive decline | Severe malnutrition, dehydration, severe pressure sores, infections (pneumonia, sepsis), and failure of multiple organ systems. |
Nutritional Deficiencies and Malnutrition
A significant, often overlooked, aspect of Alzheimer’s disease progression is the role of nutritional deficiencies and malnutrition. These conditions, frequently present in individuals with Alzheimer’s, can exacerbate existing symptoms, hinder treatment effectiveness, and contribute to a decline in overall health. The impact on the immune system and bodily functions is substantial, making nutritional support a crucial element in managing the disease.Nutritional deficiencies can stem from various factors, including reduced appetite, difficulty chewing or swallowing (dysphagia), decreased social interaction, and the inability to prepare or access adequate meals.
These challenges, compounded by the cognitive decline associated with Alzheimer’s, can lead to a vicious cycle of worsening nutritional status and declining health. Addressing these deficiencies is essential for improving quality of life and potentially slowing disease progression.
Sadly, Alzheimer’s disease often leads to death from complications like infections, malnutrition, and ultimately, the gradual failure of vital organs. While researching different health issues, I stumbled across interesting information about the potential interplay between hidradenitis suppurative and COVID-19, hidradenitis suppurative and covid 19 , which highlighted the importance of understanding how various health conditions can interact.
This further emphasizes the complex interplay of factors contributing to death in those with Alzheimer’s.
Common Nutritional Deficiencies
A range of nutritional deficiencies are frequently observed in Alzheimer’s patients. These include deficiencies in essential vitamins like B vitamins (particularly B12), vitamin D, and vitamin E, as well as minerals such as iron, zinc, and calcium. Protein deficiency is also a concern, given the increased metabolic demands of the body. These deficiencies can arise from various factors, including dietary restrictions, decreased food intake, and difficulties with food preparation and consumption.
Impact on Overall Health
Nutritional deficiencies significantly impact overall health and contribute to disease progression. Vitamin B12 deficiency, for example, can lead to neurological symptoms, including fatigue, weakness, and cognitive impairment. Vitamin D deficiency can increase the risk of falls and fractures, while iron deficiency can result in anemia, leading to further fatigue and weakness. These deficiencies can also weaken the immune system, making individuals more susceptible to infections and slowing the healing process.
The impact of malnutrition on overall health can be substantial and potentially accelerate the progression of Alzheimer’s.
Impact on Body Weakening
Malnutrition, characterized by a lack of essential nutrients, can lead to a gradual weakening of the body. Reduced protein intake, for instance, can impair muscle function, increasing the risk of falls and injuries. Deficiencies in vitamins and minerals contribute to weakened bones, making fractures more likely. The cumulative effect of these deficiencies can lead to a general decline in physical strength and stamina, making daily tasks increasingly difficult for individuals with Alzheimer’s.
Impact on the Immune System
The immune system is significantly affected by malnutrition, impacting its ability to fight off infections. A lack of essential nutrients compromises the production and function of immune cells, reducing the body’s defenses against pathogens. This can result in increased susceptibility to infections, prolonged recovery times, and a higher risk of complications. The table below illustrates the relationship between malnutrition and immune function.
| Nutritional Deficiency | Impact on Immune System | Impact on Overall Function |
|---|---|---|
| Vitamin C deficiency | Reduced production of antibodies, decreased immune cell function | Increased susceptibility to infections, delayed wound healing |
| Protein deficiency | Impaired immune cell development and function | Reduced muscle mass, increased risk of infections |
| Zinc deficiency | Reduced immune cell activity, impaired wound healing | Impaired immune response, increased susceptibility to infections |
| Iron deficiency | Reduced red blood cell production, reduced oxygen delivery to tissues | Anemia, fatigue, impaired cognitive function |
Importance of Proper Nutrition
Proper nutrition plays a crucial role in maintaining overall health and preventing complications in individuals with Alzheimer’s. A balanced diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats is essential. Ensuring adequate intake of essential vitamins and minerals is critical. For example, individuals might benefit from fortified foods or supplements, under the guidance of a healthcare professional.
Maintaining a consistent eating schedule and addressing any swallowing difficulties are also important strategies for promoting nutritional intake. These efforts can significantly improve the overall health and well-being of individuals with Alzheimer’s, mitigating the negative impact of nutritional deficiencies.
Secondary Infections and Immunosuppression
Alzheimer’s disease isn’t just about memory loss; it significantly impacts the body’s ability to fight off infections. Weakened immune responses and a compromised ability to heal create a vicious cycle where infections can easily take hold and worsen the overall condition of the patient. This vulnerability to secondary infections is a crucial aspect of the disease’s progression and a significant contributor to mortality.The immune system, a complex network of cells and proteins, plays a vital role in defending the body against harmful pathogens.
In Alzheimer’s disease, this intricate system is disrupted, leading to impaired immune function. This compromised immune response leaves individuals more susceptible to infections that would otherwise be easily managed by a healthy immune system. This vulnerability, combined with the physiological changes associated with Alzheimer’s, can lead to more serious health complications and, ultimately, a shortened lifespan.
The Role of the Immune System in Alzheimer’s Disease
The immune system’s response to Alzheimer’s disease is complex and multifaceted. The accumulation of amyloid plaques and tau tangles, hallmarks of the disease, triggers an inflammatory response. This response, while initially intended to clear these abnormal proteins, can become chronic and damaging. Over time, this chronic inflammation further weakens the immune system’s ability to fight off opportunistic infections.
Common Secondary Infections in Alzheimer’s Patients
Several types of infections commonly affect Alzheimer’s patients. Pneumonia, often caused by bacteria or viruses, is a frequent and serious concern. Urinary tract infections (UTIs) are also prevalent, stemming from the compromised immune system and often the increased need for catheterization. Skin infections, such as pressure ulcers or cellulitis, are more common due to reduced mobility and decreased tissue regeneration capabilities.
Fungal infections, like candidiasis, can also arise from impaired immune responses and compromised skin integrity.
Mechanisms of Infection Contribution to Disease Progression
Infections can significantly exacerbate Alzheimer’s disease in several ways. The inflammatory response triggered by the infection adds to the existing chronic inflammation, further damaging brain tissues and potentially accelerating the progression of neurodegeneration. Infections can also consume vital resources, diverting the body’s energy and immune cells away from the fight against the Alzheimer’s-related pathology. The resulting systemic inflammation can lead to further complications, including organ dysfunction and even death.
For example, a simple pneumonia can quickly lead to respiratory failure in an Alzheimer’s patient due to a weakened immune response and the overall physiological deterioration of the body.
Immunosuppression in Alzheimer’s Disease, What causes death in people with alzheimers disease
Alzheimer’s disease weakens the immune system through various mechanisms. The chronic inflammation associated with the disease reduces the production of immune cells and antibodies. Additionally, the disruption of neuro-immune communication can lead to impaired immune responses. This overall immunosuppression leaves the individual vulnerable to a wide range of infections, which can, in turn, accelerate the progression of Alzheimer’s disease and contribute to its severity.
Relationship Between Infections and Mortality in Alzheimer’s Patients
Studies have shown a strong correlation between infections and mortality in Alzheimer’s patients. A higher frequency of infections and their severity are often linked to a decreased lifespan. For example, a study published in the Journal of Alzheimer’s Disease demonstrated a significant increase in mortality rates among Alzheimer’s patients experiencing pneumonia compared to those without infections. This data highlights the critical role that secondary infections play in the overall prognosis and outcome of Alzheimer’s disease.
Dehydration and Fluid Imbalance
Dehydration is a significant concern for Alzheimer’s patients, often exacerbating existing health issues and contributing to a decline in overall well-being. The challenges in communication and self-care common in Alzheimer’s can lead to inadequate fluid intake, making dehydration a serious and frequently overlooked complication. This poses a substantial risk to their health, as the body struggles to maintain essential functions.The complex interplay between cognitive decline and the ability to recognize thirst cues can result in inadequate fluid intake, a crucial factor in maintaining bodily functions.
Moreover, behavioral changes, such as wandering or disorientation, can prevent patients from accessing water or understanding the importance of hydration.
Common Causes of Dehydration
Alzheimer’s patients may experience difficulty with daily tasks, including recognizing the need to drink fluids. This can stem from several factors, including: memory loss regarding hydration, impaired swallowing, reduced oral intake due to dental problems, and altered perception of thirst. Changes in appetite or medication side effects can also contribute.
How Dehydration Contributes to Decline
Dehydration in Alzheimer’s patients compromises numerous bodily systems, ultimately contributing to a decline in health. Reduced blood volume leads to decreased blood pressure, impacting organ perfusion. This can manifest as fatigue, confusion, and dizziness, further hindering their ability to participate in daily activities. Dehydration also affects kidney function, potentially leading to acute kidney injury.
Importance of Maintaining Hydration
Adequate hydration is crucial for maintaining optimal cognitive function, and it directly impacts the effectiveness of other treatments. Hydration supports metabolic processes, transports nutrients, and regulates body temperature, all essential aspects of well-being. A hydrated body is better equipped to handle the effects of the disease, potentially delaying the progression of certain symptoms.
Mechanisms of Organ Failure
Dehydration’s impact on organ function is multifaceted. Reduced blood volume can trigger the release of stress hormones, placing undue strain on the cardiovascular system. The kidneys, tasked with filtering waste, become compromised by the reduced fluid intake, leading to a buildup of toxins. The brain, particularly vulnerable to changes in hydration, experiences reduced oxygen supply and altered metabolic function.
This can cause confusion, disorientation, and further cognitive decline.
Alzheimer’s disease often leads to death from complications like infections or malnutrition. It’s a gradual decline affecting various bodily functions. While researching the causes, it’s important to note that similar oral issues can arise in other conditions, such as hiv mouth sores pictures , highlighting the importance of comprehensive medical care. Ultimately, the multifaceted nature of Alzheimer’s disease contributes to the eventual demise of those affected.
Symptoms of Dehydration and Correlation to Alzheimer’s
| Symptom | Correlation to Alzheimer’s | Description |
|---|---|---|
| Dry mouth | Common; reduced awareness of thirst | A noticeable dryness of the mouth, often accompanied by difficulty swallowing or speaking. |
| Decreased urine output | Reduced awareness of need to urinate | Little or no urine production, indicating fluid loss. |
| Confusion and disorientation | Exacerbates existing cognitive issues | Increased confusion and difficulty with spatial awareness; may be mistaken for worsening dementia. |
| Fatigue and lethargy | Can be misinterpreted as normal disease progression | Extreme tiredness, lack of energy, and general sluggishness. |
| Headache | Can be a sign of underlying dehydration | Pain in the head, potentially aggravated by exertion or movement. |
| Dark urine | Concentrated urine; reduced fluid intake | Urine that is darker than usual, suggesting the body is conserving fluids. |
| Sunken eyes | Severe dehydration; immediate medical attention | Noticeable depression or hollowing of the eyes, indicating significant fluid loss. |
Medication Interactions and Side Effects
Medication interactions are a significant concern for Alzheimer’s patients, as the disease often necessitates multiple medications for various symptoms and potential complications. These medications can interact in unpredictable ways, leading to adverse effects that could worsen the patient’s condition and potentially contribute to their decline. Understanding these interactions is crucial for managing Alzheimer’s patients effectively and minimizing harm.
Potential Interactions Between Alzheimer’s Medications and Other Drugs
Alzheimer’s disease often requires a combination of medications, each with its own set of potential side effects. These drugs can interact with each other and with other medications the patient may be taking for other conditions. These interactions can significantly alter the effectiveness of the prescribed drugs, leading to reduced therapeutic benefits or increased risks.
Adverse Effects and Deterioration
Medication side effects can exacerbate existing symptoms of Alzheimer’s, potentially leading to a faster decline in cognitive function and overall well-being. For instance, some medications can cause confusion, disorientation, or agitation, making it difficult for the patient to manage daily tasks. These side effects can also impact the patient’s quality of life and increase the burden on caregivers.
Furthermore, some interactions can cause serious, potentially life-threatening, complications.
Importance of Monitoring Medication Use in Alzheimer’s Patients
Careful monitoring of medication use is essential to mitigate the risks of adverse interactions. This involves regular review of all medications, including prescription drugs, over-the-counter medications, and supplements. Healthcare providers need to be aware of all the medications a patient is taking to prevent potentially harmful interactions. Regular communication between the patient, their caregivers, and healthcare professionals is critical to identify and address any emerging issues promptly.
Sadly, various factors contribute to the demise of Alzheimer’s patients. While cognitive decline is a prominent aspect, it’s often complications like infections or, surprisingly, issues like cardiac sarcoidosis, which can significantly impact overall health. Learning more about this condition can help you understand the multifaceted nature of Alzheimer’s progression and potential contributing factors. For a deeper dive into cardiac sarcoidosis, check out this informative resource: cardiac sarcoidosis what you should know.
Ultimately, understanding these complexities is crucial in comprehending the multifaceted causes of death in Alzheimer’s patients.
Table of Potential Drug Interactions
| Medication Category | Potential Interaction | Possible Side Effects | Impact on Alzheimer’s Progression |
|---|---|---|---|
| Cholinesterase Inhibitors (e.g., Donepezil, Rivastigmine) | Anticholinergics (e.g., some antidepressants, antihistamines) | Increased risk of bradycardia, gastrointestinal issues, confusion | Potentially accelerated cognitive decline due to increased confusion and decreased quality of life. |
| Antipsychotics (e.g., for agitation) | Many other medications | Increased risk of falls, stroke, and cardiovascular events | Can worsen cognitive impairment and contribute to faster decline. Examples of such medications can be antihypertensives. |
| Benzodiazepines (e.g., for anxiety) | Many medications, including alcohol | Drowsiness, confusion, impaired coordination | Can worsen cognitive impairment and contribute to faster decline. |
| Statins (e.g., for cholesterol) | Some medications | Muscle pain, liver damage | Can potentially worsen existing muscle weakness or pain in patients with Alzheimer’s. |
Pressure Ulcers and Immobility
Pressure ulcers, also known as bedsores, are a serious complication arising from prolonged pressure on the skin. They’re particularly prevalent in individuals with reduced mobility, such as those with Alzheimer’s disease, and significantly impact their overall health and well-being. Understanding the link between immobility and pressure ulcers is crucial for effective prevention and management in this population.Prolonged immobility in Alzheimer’s patients leads to decreased blood flow to the affected areas.
This diminished circulation, combined with the pressure exerted on the skin by bony prominences like the heels, hips, and elbows, creates an environment conducive to tissue damage. This can be exacerbated by the cognitive decline often associated with Alzheimer’s, which may lead to decreased awareness of discomfort and reduced ability to communicate needs.
Relationship Between Immobility and Pressure Ulcer Development
Immobility directly contributes to the development of pressure ulcers by reducing the movement of blood and other essential nutrients to the affected skin areas. When a person remains in one position for extended periods, the pressure on bony prominences compresses the blood vessels, hindering the flow of oxygen and nutrients to the skin cells. This lack of blood supply causes cell death and tissue breakdown.
Pressure Ulcer Contribution to Deterioration of Health
Pressure ulcers significantly impact the health of Alzheimer’s patients. They can cause significant pain and discomfort, making it difficult for the individual to move, sleep, and participate in daily activities. The open wounds can become infected, leading to sepsis, a life-threatening condition. The added burden of managing a pressure ulcer further stresses the patient’s already compromised immune system.
Moreover, the treatment of pressure ulcers often requires extensive care and resources, putting a strain on caregivers and healthcare systems.
Link Between Immobility and Increased Susceptibility to Infections
Immobility weakens the immune system, increasing susceptibility to infections. The decreased blood flow associated with immobility can impair the body’s ability to fight off infections, and pressure ulcers provide a direct entry point for bacteria to invade the body. This heightened risk of infection further complicates the management of pressure ulcers, potentially leading to serious systemic complications.
Stages of Pressure Ulcers
Pressure ulcers progress through distinct stages, each characterized by increasing tissue damage. Understanding these stages is critical for timely intervention and prevention.
- Stage 1: Non-blanchable erythema (redness) of the skin. This is the earliest stage and often reversible if pressure is relieved. The skin might appear reddened but is intact. This stage often presents as redness over bony prominences and may be overlooked, particularly in individuals with darker skin tones.
- Stage 2: Partial-thickness skin loss involving epidermis and/or dermis. The wound may appear as a blister, abrasion, or shallow ulcer. The wound bed is pink or red and may be moist.
- Stage 3: Full-thickness skin loss. Subcutaneous fat may be visible, but bone, tendon, or muscle are not exposed. The wound may have a deep crater-like appearance.
- Stage 4: Full-thickness tissue loss with exposed bone, tendon, or muscle. The wound is often deep and extensive.
- Unstageable Pressure Ulcer: Full-thickness tissue loss in which the base of the ulcer is covered by eschar (dead tissue). The eschar obscures the depth of the ulcer, making it impossible to determine the stage.
Prevention Strategies for Pressure Ulcers in Alzheimer’s Patients
Early detection and proactive measures are crucial for preventing pressure ulcers in Alzheimer’s patients. Regular turning, repositioning, and appropriate pressure relief are vital components of a preventative strategy.
| Prevention Strategy | Detailed Description |
|---|---|
| Regular repositioning | Frequent turning and repositioning of the patient, ideally every two hours, helps distribute pressure and prevents prolonged pressure on bony prominences. |
| Specialized equipment | Using pressure-reducing mattresses, cushions, or other specialized equipment helps redistribute pressure and prevent tissue damage. These aids provide a layer of support, reducing the direct contact between the patient and the surface they are lying on. |
| Skin care | Regularly moisturizing the skin and maintaining good skin hygiene are crucial for preventing dryness and cracking, which can make the skin more susceptible to pressure injuries. |
| Nutrition and hydration | Maintaining adequate nutrition and hydration is vital for overall health and skin integrity. |
| Regular assessment | Regularly assessing the skin for any signs of redness or pressure sores is critical for early detection. Caregivers and healthcare professionals should be vigilant in monitoring the skin for any changes. |
| Patient and caregiver education | Educating patients and caregivers about the importance of pressure ulcer prevention and the signs to watch for is crucial for effective management. |
Swallowing Difficulties and Aspiration: What Causes Death In People With Alzheimers Disease
Swallowing difficulties, a common symptom in Alzheimer’s disease, can significantly impact a patient’s quality of life and, unfortunately, contribute to serious health complications. These difficulties often arise from progressive neurological damage, making the act of swallowing increasingly challenging. The implications extend beyond discomfort; impaired swallowing can lead to a potentially life-threatening condition called aspiration pneumonia.Progressive brain changes associated with Alzheimer’s disease affect the complex motor functions needed for coordinated swallowing.
The muscles responsible for moving food from the mouth to the stomach become weaker and less efficient, resulting in difficulties with different stages of the swallowing process. This includes problems with initiating the swallow, moving food through the pharynx (throat), and transporting it safely to the esophagus.
Causes of Swallowing Difficulties
Neurological damage inherent to Alzheimer’s disease disrupts the intricate pathways and signals that control the muscles involved in swallowing. The progressive loss of neurons and the accumulation of amyloid plaques and neurofibrillary tangles in the brain directly impact the coordination of these crucial movements. As the disease progresses, these difficulties become more pronounced, increasing the risk of aspiration.
Certain medications used to manage Alzheimer’s symptoms can also have side effects that worsen swallowing difficulties.
Aspiration Pneumonia: A Serious Complication
Aspiration pneumonia occurs when food, liquids, or saliva enter the lungs instead of the esophagus. This foreign material triggers an inflammatory response in the lungs, leading to infection and inflammation. The compromised immune system often seen in Alzheimer’s patients makes them more susceptible to this infection. The impaired swallowing mechanism allows for easier entry of food particles into the airways.
This process can be accelerated by factors such as decreased awareness of the swallowing process and reduced saliva production, further hindering the natural protective mechanisms of the throat.
Aspiration Pneumonia and Mortality in Alzheimer’s Patients
Aspiration pneumonia is a significant cause of death in Alzheimer’s patients. The infection can rapidly worsen the patient’s condition, leading to respiratory distress, organ failure, and ultimately, death. The compromised immune system and the inability to clear the infection effectively contribute to the severity of the pneumonia. Patients with Alzheimer’s disease are already vulnerable to infections due to their weakened immune response, and aspiration pneumonia can quickly overwhelm their systems.
Monitoring for Swallowing Difficulties
Early detection of swallowing difficulties is crucial for preventing aspiration pneumonia. Regular assessment by healthcare professionals, including speech-language pathologists, is essential to identify potential issues and implement appropriate interventions. This includes observation of the patient’s eating habits, evaluation of the consistency of food and liquids, and analysis of the patient’s overall response during meals. A comprehensive assessment, focusing on the patient’s swallowing ability, is paramount in managing the risk of aspiration pneumonia.
Table Demonstrating the Link Between Aspiration Pneumonia and Mortality
| Aspiration Pneumonia | Mortality Rate (Estimated Percentage) | Explanation |
|---|---|---|
| Mild Aspiration Episodes | Low | The body’s immune response is usually able to clear the infection, with supportive care. |
| Moderate Aspiration Episodes | Moderate | Frequent aspiration episodes lead to inflammation and infections, necessitating interventions and treatment. |
| Severe Aspiration Episodes | High | Severe episodes often lead to respiratory distress, organ failure, and death, particularly in patients with weakened immune systems. |
Final Summary
In conclusion, Alzheimer’s disease is not a single cause of death, but rather a confluence of factors. The progressive damage to the brain, coupled with systemic issues, nutritional problems, infections, and complications from medications and immobility, all contribute to the ultimate decline and death of those afflicted. While a definitive cure remains elusive, a comprehensive understanding of these factors allows for more effective management of symptoms and potential interventions to improve quality of life and potentially delay the disease progression.