Ace inhibitors vs beta blockers: Understanding these two classes of antihypertensive medications is crucial for managing high blood pressure effectively. Each works through distinct mechanisms impacting the cardiovascular system, leading to different effects and potential side effects. This exploration delves into the intricacies of how they function, comparing their efficacy, and considering patient-specific factors that influence treatment decisions.
This in-depth comparison will explore the mechanisms of action for each, their effects on blood pressure and other physiological parameters, potential side effects, and how these factors influence patient selection. We’ll examine the role of the renin-angiotensin-aldosterone system, and the sympathetic nervous system, to understand the underlying biology. Ultimately, we’ll help you understand which medication might be better suited for your needs or the needs of a loved one.
Introduction to Antihypertensive Medications
High blood pressure, or hypertension, is a significant risk factor for cardiovascular diseases like heart attacks and strokes. Managing blood pressure effectively is crucial for maintaining overall health and well-being. Antihypertensive medications play a vital role in this process, working to lower blood pressure and reduce the risk of associated complications. These medications target various mechanisms in the body responsible for blood pressure regulation.Blood pressure regulation is a complex process involving multiple interacting factors.
Maintaining a healthy balance of these factors is essential for cardiovascular health. Antihypertensive drugs aim to restore this balance by interfering with the processes that elevate blood pressure, ultimately reducing the strain on the heart and blood vessels. Selecting the appropriate antihypertensive medication requires careful consideration of individual patient characteristics, including medical history, lifestyle factors, and potential side effects.
This personalized approach is critical to ensuring optimal treatment outcomes and minimizing adverse reactions.
General Mechanisms of Action of Antihypertensive Drugs, Ace inhibitors vs beta blockers
Antihypertensive medications work through diverse mechanisms, targeting different aspects of blood pressure regulation. Some drugs inhibit the production of hormones that constrict blood vessels, while others promote the excretion of excess sodium and water, reducing blood volume. Others influence the contraction of blood vessels themselves. This multifaceted approach ensures a range of options to address individual patient needs.
Role of Blood Pressure Regulation in Cardiovascular Health
Blood pressure is the force exerted by blood against the walls of the blood vessels. Sustained high blood pressure damages blood vessel walls, increasing the risk of atherosclerosis, a condition characterized by plaque buildup in the arteries. This buildup can lead to reduced blood flow, potentially causing heart attacks, strokes, and kidney damage. Maintaining healthy blood pressure is crucial for preventing these serious cardiovascular complications.
Significance of Choosing the Right Antihypertensive for Individual Patients
The choice of antihypertensive medication is not a one-size-fits-all approach. Factors such as the patient’s overall health, other medical conditions, and potential drug interactions need careful consideration. For example, a patient with diabetes might require a different medication regimen than someone with a history of kidney disease. Individualized treatment plans, considering all relevant factors, are essential for optimal management of hypertension.
Comparison of Antihypertensive Medication Classes
The following table provides a general overview of common antihypertensive drug classes, highlighting their mechanisms of action and potential side effects. Choosing the appropriate class depends on individual patient characteristics and factors such as age, comorbidities, and lifestyle.
| Drug Class | Mechanism of Action | Examples | Potential Side Effects |
|---|---|---|---|
| ACE Inhibitors | Block the production of angiotensin II, a hormone that constricts blood vessels. | Lisinopril, Enalapril | Dry cough, dizziness, kidney problems |
| Beta-Blockers | Reduce heart rate and the force of heart contractions, thus lowering blood pressure. | Metoprolol, Atenolol | Fatigue, dizziness, cold hands and feet |
| Diuretics | Increase the excretion of sodium and water, reducing blood volume. | Hydrochlorothiazide, Furosemide | Dehydration, electrolyte imbalances |
| Calcium Channel Blockers | Relax blood vessel walls by reducing calcium influx. | Amlodipine, Diltiazem | Headache, swelling in ankles and feet |
Ace Inhibitors
Ace inhibitors, a crucial class of antihypertensive medications, work by targeting a key player in the renin-angiotensin-aldosterone system (RAAS). Understanding their mechanism of action is essential for comprehending their effectiveness and potential side effects.
Mechanism of Action
ACE inhibitors, or angiotensin-converting enzyme inhibitors, function by inhibiting the enzyme angiotensin-converting enzyme (ACE). This enzyme plays a vital role in converting angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor, meaning it narrows blood vessels, increasing blood pressure. By blocking ACE, ace inhibitors prevent this conversion, thus reducing the amount of angiotensin II in the body.
This reduction in angiotensin II leads to a decrease in peripheral resistance, which ultimately lowers blood pressure. Furthermore, ACE inhibitors can also impact the level of bradykinin, a vasodilator.
Effects on Blood Pressure Regulation
The primary effect of ace inhibitors is a reduction in blood pressure. This occurs through several interconnected mechanisms. Reduced angiotensin II levels lead to a decrease in vasoconstriction, allowing blood vessels to relax and widen. This, in turn, lowers peripheral resistance, facilitating easier blood flow and decreasing blood pressure. Additionally, ace inhibitors can influence the levels of bradykinin, a substance that has vasodilatory properties.
While typically considered a side effect, an increase in bradykinin can contribute to the lowering of blood pressure. The balance between these opposing forces (vasoconstriction and vasodilation) is critical in blood pressure regulation.
Potential Side Effects
ACE inhibitors, while effective, can sometimes cause adverse effects. One notable side effect is a persistent cough, often described as dry and hacking. This is believed to be related to increased bradykinin levels. Other potential side effects include dizziness, fatigue, headache, and, in rare cases, more serious reactions like angioedema (swelling of the face, lips, tongue, or throat).
It’s important to note that individual responses to ace inhibitors can vary.
Pharmacokinetics of ACE Inhibitors
The pharmacokinetics of ACE inhibitors, which describe how the body absorbs, distributes, metabolizes, and excretes the drug, significantly influence their effectiveness and safety. Understanding these factors is critical for appropriate dosing and patient management.
| Pharmacokinetic Parameter | Description |
|---|---|
| Absorption | ACE inhibitors are typically administered orally. Absorption rates vary depending on the specific medication, but generally, they are well absorbed from the gastrointestinal tract. Food can sometimes slightly delay absorption. |
| Distribution | ACE inhibitors are distributed throughout the body, affecting various tissues and organs. Their distribution depends on factors like protein binding and tissue permeability. |
| Metabolism | Most ACE inhibitors are metabolized in the liver, often by the cytochrome P450 enzyme system. This process can influence drug interactions and the potential for side effects. |
| Excretion | The primary route of excretion for ACE inhibitors is through the kidneys. The kidneys filter and eliminate the drug from the body. Impaired kidney function can impact the excretion rate and require dose adjustments. |
Beta-Blockers
Beta-blockers are a class of medications commonly prescribed to manage high blood pressure and other cardiovascular conditions. They work by interfering with the effects of adrenaline and noradrenaline, hormones released by the sympathetic nervous system, which typically increase heart rate and blood pressure. Understanding their mechanism of action is crucial for comprehending their impact on various physiological parameters and recognizing potential side effects.
Mechanism of Action
Beta-blockers primarily exert their effects by blocking beta-adrenergic receptors, specifically beta-1 and beta-2 receptors, in the heart and other tissues. These receptors are part of the sympathetic nervous system, which plays a key role in the body’s fight-or-flight response. By blocking these receptors, beta-blockers reduce the stimulatory effects of adrenaline and noradrenaline. This, in turn, lowers heart rate, reduces the force of heart contractions, and decreases the demand for oxygen by the heart.
Effects on Physiological Parameters
Beta-blockers have a significant impact on several physiological parameters. They typically reduce heart rate, which is a key factor in controlling blood pressure. The reduced force of heart contractions lowers blood pressure by decreasing the output of blood from the heart. Additionally, beta-blockers can influence other systems in the body. For example, they can affect lung function, potentially causing bronchospasm in individuals with asthma or other respiratory conditions.
Furthermore, they may impact glucose metabolism and blood sugar levels, which needs careful consideration for patients with diabetes.
Potential Side Effects
The side effects of beta-blockers can vary depending on the specific subtype of beta-blocker. Some common side effects include fatigue, dizziness, and cold extremities. Cardio-selective beta-blockers, designed to primarily affect beta-1 receptors in the heart, are generally associated with fewer side effects on the lungs than non-selective beta-blockers. However, even cardio-selective beta-blockers can induce bronchospasm in susceptible individuals.
Careful monitoring is essential to identify and manage any potential adverse reactions.
So, I’ve been researching ace inhibitors vs beta blockers lately, and it’s fascinating how different drugs can impact your health. While I’m not a doctor, I’ve been curious about how a healthy diet can potentially help manage blood pressure, which is a key consideration when weighing the pros and cons of these medications. For instance, can eating watermelon daily help you lose weight?
This article suggests that it might contribute to overall health, potentially improving blood pressure and weight management. Ultimately, consulting with a healthcare professional remains crucial when considering the best approach for managing blood pressure and choosing between ace inhibitors and beta blockers.
Beta-Blocker Subtypes
Understanding the differences between beta-blocker subtypes is critical for tailoring treatment to individual needs and minimizing potential risks. The distinctions primarily lie in their selectivity for beta-1 and beta-2 receptors.
| Subtype | Selectivity | Primary Effects | Potential Side Effects |
|---|---|---|---|
| Cardio-selective (e.g., Metoprolol, Atenolol) | Primarily affect beta-1 receptors in the heart | Reduced heart rate, decreased blood pressure, reduced heart contractility | Less likely to cause bronchospasm, but can still affect blood sugar and lung function in some cases |
| Non-selective (e.g., Propranolol, Nadolol) | Affect both beta-1 and beta-2 receptors | Reduced heart rate, decreased blood pressure, reduced heart contractility, potential bronchospasm | Increased risk of bronchospasm in patients with respiratory conditions, can mask symptoms of hypoglycemia |
Comparing Ace Inhibitors and Beta-Blockers
Choosing between ACE inhibitors and beta-blockers for managing hypertension often depends on individual patient characteristics and the presence of co-morbidities. Both classes are crucial in blood pressure management, but their mechanisms of action and side effects differ, influencing their suitability for specific patient groups. Understanding these nuances is vital for clinicians to make informed treatment decisions.
Mechanisms of Action
ACE inhibitors and beta-blockers work through distinct physiological pathways to lower blood pressure. ACE inhibitors, such as lisinopril and ramipril, primarily inhibit the angiotensin-converting enzyme (ACE). This enzyme plays a role in the production of angiotensin II, a potent vasoconstrictor. By blocking ACE, these drugs reduce angiotensin II levels, leading to vasodilation (widening of blood vessels) and a decrease in blood pressure.
Beta-blockers, such as metoprolol and atenolol, reduce blood pressure by blocking beta-adrenergic receptors in the heart and blood vessels. This action decreases heart rate and contractility, reducing the workload on the heart and thereby lowering blood pressure. This differing mechanism of action explains some of the variations in their effects on patients.
Potential Benefits and Drawbacks in Different Patient Populations
ACE inhibitors are often preferred in patients with diabetes or kidney disease, as they can have beneficial effects on kidney function. Their vasodilatory effect can also be advantageous in patients with conditions like heart failure. However, ACE inhibitors can cause a dry cough in some individuals, and are contraindicated in patients with bilateral renal artery stenosis. Beta-blockers are valuable in patients with angina, or those experiencing rapid heart rate or anxiety.
They are also frequently used in patients with a history of myocardial infarction. However, beta-blockers can mask the symptoms of hypoglycemia in diabetics and may have adverse effects on asthma patients.
Situations Where One Class Might Be Preferred Over the Other
In patients with chronic kidney disease (CKD), ACE inhibitors are often the first-line therapy. Their renoprotective effects can slow the progression of the disease. Conversely, beta-blockers are more appropriate for patients with hypertension and co-morbidities such as angina or atrial fibrillation. The presence of a history of stroke might also lean towards beta-blocker therapy. The decision depends on careful consideration of individual patient needs.
Summary Table
| Characteristic | ACE Inhibitors | Beta-Blockers |
|---|---|---|
| Mechanism of Action | Inhibit angiotensin-converting enzyme (ACE) | Block beta-adrenergic receptors |
| Efficacy | Generally effective in lowering blood pressure, especially in patients with diabetes or kidney disease. | Effective in lowering blood pressure, particularly in patients with angina or rapid heart rate. |
| Side Effects | Dry cough, dizziness, angioedema (rare but serious). | Fatigue, dizziness, bradycardia (slow heart rate), potential masking of hypoglycemia in diabetics. |
| Contraindications | Pregnancy, bilateral renal artery stenosis, history of angioedema. | Severe bradycardia, asthma, severe heart block. |
| Patient Populations | Often preferred in patients with diabetes, kidney disease, and heart failure. | Often preferred in patients with angina, rapid heart rate, or anxiety. |
Patient Considerations and Selection

Choosing the right antihypertensive medication requires a nuanced approach, considering the individual patient’s unique characteristics. A one-size-fits-all approach is rarely effective. Factors such as medical history, concurrent health conditions, lifestyle, and potential drug interactions play critical roles in determining the optimal treatment plan.
Patient History and Comorbidities
Patient history provides invaluable insights into potential drug sensitivities and interactions. A thorough medical history, including past cardiovascular events, kidney disease, diabetes, and other chronic conditions, significantly influences treatment decisions. For example, a patient with a history of kidney disease might be more susceptible to adverse effects from ACE inhibitors and may require careful monitoring. Similarly, patients with asthma or other respiratory issues may require alternative medications due to potential bronchospasm risks.
The presence of other comorbidities like heart failure or peripheral artery disease may dictate the need for specific antihypertensive agents.
Lifestyle Factors
Lifestyle factors significantly impact blood pressure management and medication adherence. Dietary habits, exercise routines, stress levels, and alcohol consumption all contribute to overall cardiovascular health. Patients with a history of poor adherence to lifestyle modifications may require medications that are easier to incorporate into their daily routines. Consideration of factors like cost, ease of administration, and potential side effects are crucial for patient buy-in and adherence.
Patient Education and Adherence
Patient education is paramount to successful antihypertensive therapy. Clear communication about the medication’s purpose, potential side effects, and importance of adherence is crucial. Patients must understand the rationale behind their treatment plan and how it contributes to their overall health. Educational materials should be tailored to the patient’s comprehension level and cultural background. This includes explaining the importance of regular follow-up appointments, monitoring blood pressure at home, and recognizing early signs of adverse reactions.
So, I’ve been doing some research on ace inhibitors vs beta blockers, and it’s fascinating how they affect your body. Ultimately, maintaining a healthy lifestyle, including regular exercise, is key to managing blood pressure. Figuring out what exercise burns the most calories what exercise burns the most calories can help you achieve your goals, but understanding how these medications work is equally important.
In the end, it’s a balancing act between medication and exercise for optimal health.
Strong patient-physician communication is vital for maintaining treatment adherence and ensuring optimal outcomes.
Potential Drug Interactions
Careful consideration of potential drug interactions is essential to avoid adverse effects and optimize treatment efficacy.
| ACE Inhibitor | Beta-blocker | Other Medications | Potential Interaction |
|---|---|---|---|
| ACE Inhibitors | Beta-blockers | Potassium-sparing diuretics (e.g., spironolactone) | Increased risk of hyperkalemia (high potassium levels). |
| ACE Inhibitors | Beta-blockers | Nonsteroidal anti-inflammatory drugs (NSAIDs) | Potential reduction in antihypertensive effect and increased risk of kidney injury. |
| ACE Inhibitors | Beta-blockers | Lithium | Increased risk of lithium toxicity. |
| ACE Inhibitors | Beta-blockers | Angiotensin II receptor blockers (ARBs) | Possible additive blood pressure lowering effect, but potential for increased risk of kidney injury. |
The table above provides a simplified overview of potential interactions. Always consult with a physician or pharmacist for personalized guidance and to ensure safe and effective medication combinations.
Clinical Applications and Case Studies
ACE inhibitors and beta-blockers are cornerstone medications in managing hypertension and other cardiovascular conditions. Understanding their specific applications and the importance of meticulous patient monitoring are crucial for optimal therapeutic outcomes. This section delves into clinical scenarios where each class of drug is frequently the preferred choice, highlighting the importance of tailored treatment strategies.Applying these medications appropriately and observing the patients’ responses with careful monitoring are essential aspects of successful treatment.
Monitoring parameters, as detailed later, help clinicians assess efficacy and identify potential side effects promptly.
Clinical Scenarios Favoring ACE Inhibitors
ACE inhibitors often take center stage in certain cardiovascular conditions. Their specific benefits and mechanisms of action make them the preferred choice in specific situations.
- Diabetic Nephropathy: ACE inhibitors are frequently prescribed in patients with diabetes who exhibit signs of kidney damage. Their ability to reduce glomerular filtration pressure helps slow the progression of kidney disease, a significant concern in diabetic populations. For instance, a patient with type 2 diabetes and microalbuminuria might benefit from an ACE inhibitor like lisinopril to preserve kidney function.
- Heart Failure with Reduced Ejection Fraction (HFrEF): In cases of heart failure where the heart’s pumping ability is compromised, ACE inhibitors are frequently a cornerstone of treatment. Their ability to reduce afterload (the pressure the heart must work against) helps the heart pump more efficiently, improving symptoms and potentially extending life expectancy. For example, a patient diagnosed with HFrEF and exhibiting symptoms of shortness of breath might be prescribed an ACE inhibitor such as enalapril.
- Chronic Kidney Disease (CKD): ACE inhibitors can be beneficial in managing blood pressure and preserving kidney function in patients with CKD. This effect is particularly important in preventing further decline in kidney function and slowing the progression of the disease. For example, a patient with stage 3 CKD and hypertension could see benefits from a medication like ramipril, helping to control blood pressure and kidney function.
So, I’ve been researching ACE inhibitors versus beta-blockers lately, and it’s a fascinating comparison. Understanding how these medications affect the body is crucial for patients, and the different effects they have on blood pressure are important to note. To better understand the nuances of patient care, especially with cognitive function, you might find the Allen Cognitive Level Screen helpful.
This assessment tool, what is the Allen cognitive level screen , can be instrumental in determining a patient’s cognitive abilities, which can ultimately impact their response to medications like ACE inhibitors and beta-blockers. Ultimately, choosing the right medication requires a holistic approach, considering both physical and cognitive factors.
Clinical Scenarios Favoring Beta-Blockers
Beta-blockers, with their diverse mechanisms, are crucial in certain clinical scenarios. Their primary role often centers around the heart’s response to stress.
- Angina: Beta-blockers effectively reduce the workload on the heart by slowing the heart rate and decreasing the force of contractions. This is particularly beneficial in managing angina, where the heart’s oxygen demand exceeds its supply. For example, a patient experiencing frequent episodes of chest pain due to angina could benefit from a beta-blocker like metoprolol.
- Post-Myocardial Infarction (MI): After a heart attack, beta-blockers are often used to reduce the risk of further cardiac events. They help control heart rate and blood pressure, decreasing the strain on the heart. For instance, a patient who has recently suffered a myocardial infarction and is experiencing elevated blood pressure could benefit from a beta-blocker like carvedilol.
- Hypertension with Associated Arrhythmias: In patients with hypertension who also exhibit cardiac arrhythmias, beta-blockers can help control both conditions. By regulating the heart’s electrical activity, they can reduce the frequency of abnormal heart rhythms. For example, a patient with hypertension and episodes of atrial fibrillation might find that a beta-blocker such as atenolol is beneficial.
Importance of Monitoring Patients
Thorough monitoring is paramount when prescribing ACE inhibitors or beta-blockers. Unforeseen side effects can arise and require adjustments to the treatment plan.
Monitoring Parameters for ACE Inhibitors
- Blood pressure: Regular monitoring is crucial to assess the effectiveness of the medication and detect any potential hypotension.
- Kidney function tests (creatinine, BUN): These tests help identify any potential decline in kidney function, a significant concern with ACE inhibitors.
- Potassium levels: ACE inhibitors can affect potassium balance, necessitating regular checks to prevent hyperkalemia.
Monitoring Parameters for Beta-Blockers
- Heart rate and blood pressure: Regular monitoring is crucial to assess the medication’s impact on the heart and circulatory system.
- Blood glucose levels: Beta-blockers can mask symptoms of hypoglycemia, necessitating careful monitoring in patients with diabetes.
- Respiratory function (in some cases): Beta-blockers can affect respiratory function, so monitoring is important, particularly in patients with underlying respiratory conditions.
Potential Side Effects and Interactions
Understanding the potential side effects of ACE inhibitors and beta-blockers is crucial for safe and effective management of hypertension. These medications, while vital in controlling blood pressure, can sometimes lead to unwanted reactions. Careful monitoring and knowledge of potential interactions with other medications are essential for optimizing treatment outcomes.
Potential Side Effects of ACE Inhibitors
ACE inhibitors, while effective, can cause various side effects. These are typically manageable but require vigilance. Dry cough is a common complaint, often described as a persistent, non-productive cough. It’s important to distinguish this from other respiratory issues. Other potential side effects include dizziness, lightheadedness, and fatigue.
Angioedema, a potentially serious swelling of the face, lips, tongue, and throat, is a rare but severe side effect. Kidney problems are also possible, though less frequent. Always report any unusual symptoms to your healthcare provider immediately.
Identifying and Managing Side Effects
Early detection and appropriate management are key to minimizing the impact of side effects. Patients should be educated on recognizing symptoms like persistent cough, swelling, or unusual fatigue. Regular follow-up appointments with healthcare providers are vital for monitoring blood pressure and kidney function. If side effects are experienced, adjustments to the medication regimen, including dosage or switching to a different medication, can be considered.
Open communication with the prescribing physician is essential.
Potential Side Effects of Beta-Blockers
Beta-blockers, another crucial class of antihypertensives, also have potential side effects. Common side effects include fatigue, dizziness, and bradycardia (slow heart rate). Patients may also experience depression, insomnia, and sexual dysfunction. These side effects are often dose-dependent and can vary between individuals. It is important to note that beta-blockers can mask symptoms of hypoglycemia (low blood sugar) in diabetic patients.
Identifying and Managing Side Effects
Recognizing symptoms such as fatigue, slow heart rate, or sleep disturbances is crucial. Regular monitoring of heart rate and blood pressure by healthcare providers is essential. Adjustments to the medication, including dosage or switching to a different class of medication, can mitigate these side effects.
Drug Interactions
Drug interactions can significantly alter the effectiveness and safety of antihypertensive medications. Certain medications, including NSAIDs (nonsteroidal anti-inflammatory drugs), diuretics, and potassium supplements, can interact with ACE inhibitors and beta-blockers. This is why a thorough medication history is crucial for effective prescribing.
Table of Potential Drug Interactions
| Medication | ACE Inhibitors | Beta-Blockers |
|---|---|---|
| NSAIDs (e.g., ibuprofen, naproxen) | Increased risk of kidney problems, reduced blood pressure effect | Potential for decreased blood pressure control |
| Diuretics (e.g., furosemide, hydrochlorothiazide) | Increased risk of dehydration and electrolyte imbalance | Increased risk of dehydration and electrolyte imbalance; may potentiate bradycardia |
| Potassium Supplements | Increased risk of hyperkalemia (high potassium levels) | Increased risk of hyperkalemia |
| Lithium | Increased risk of lithium toxicity | Increased risk of lithium toxicity |
| Antidiabetic Medications | May decrease the effectiveness of some antidiabetic medications | May mask symptoms of hypoglycemia in diabetic patients |
Illustrative Information: Ace Inhibitors Vs Beta Blockers
Understanding how blood pressure is regulated and how ACE inhibitors and beta-blockers work is crucial for effectively managing hypertension. This section delves into the physiological mechanisms, providing a visual representation of the processes involved, to better grasp the actions of these medications.The intricate interplay of various systems, including the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system, dictates blood pressure.
Disruptions in these pathways can lead to hypertension, highlighting the importance of targeted interventions like ACE inhibitors and beta-blockers.
Blood Pressure Regulation: A Physiological Overview
Blood pressure is maintained by a complex interplay of factors, primarily the cardiovascular system and the autonomic nervous system. The primary goal is to maintain adequate blood flow to all vital organs. Fluctuations in blood pressure can significantly impact organ function, and sustained high blood pressure (hypertension) can lead to severe health complications. This delicate balance is regulated through various mechanisms.
The Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS is a crucial hormonal pathway that plays a significant role in regulating blood pressure and fluid balance. Activation of the RAAS leads to the production of angiotensin II, a potent vasoconstrictor, and aldosterone, which promotes sodium retention. This cascade ultimately elevates blood pressure.  Diagram Description: A diagram illustrating the renin-angiotensin-aldosterone system. The diagram depicts the sequential activation of enzymes and hormones, culminating in the production of angiotensin II and aldosterone. The diagram should show the key components like renin, angiotensinogen, angiotensin-converting enzyme (ACE), angiotensin II, and aldosterone. It should also visually demonstrate the effects of these hormones on blood vessels and the kidneys.
Diagram Description: A diagram illustrating the renin-angiotensin-aldosterone system. The diagram depicts the sequential activation of enzymes and hormones, culminating in the production of angiotensin II and aldosterone. The diagram should show the key components like renin, angiotensinogen, angiotensin-converting enzyme (ACE), angiotensin II, and aldosterone. It should also visually demonstrate the effects of these hormones on blood vessels and the kidneys.
Effects of Sympathetic Nervous System Activation on Blood Vessels
The sympathetic nervous system is a key component of the body’s fight-or-flight response. During times of stress or exertion, the sympathetic nervous system activates, causing the release of norepinephrine. This neurotransmitter acts on alpha- and beta-adrenergic receptors in blood vessel walls, resulting in vasoconstriction, thereby increasing blood pressure.  Diagram Description: A diagram showcasing the sympathetic nervous system’s impact on blood vessels. The diagram should depict the pathway of sympathetic nerve impulses, the release of norepinephrine, and the subsequent vasoconstriction of blood vessels. The diagram should highlight the involvement of alpha- and beta-adrenergic receptors in this process.
Diagram Description: A diagram showcasing the sympathetic nervous system’s impact on blood vessels. The diagram should depict the pathway of sympathetic nerve impulses, the release of norepinephrine, and the subsequent vasoconstriction of blood vessels. The diagram should highlight the involvement of alpha- and beta-adrenergic receptors in this process.
Mechanism of Action of ACE Inhibitors
ACE inhibitors prevent the conversion of angiotensin I to angiotensin II, thereby reducing vasoconstriction and lowering blood pressure. The diagram below illustrates the blockage of this conversion.  Diagram Description: A diagram illustrating the mechanism of action of ACE inhibitors. The diagram should visually represent the normal conversion of angiotensin I to angiotensin II, and how ACE inhibitors inhibit this conversion. The diagram should highlight the decreased vasoconstriction and aldosterone release as a result of this inhibition.
Diagram Description: A diagram illustrating the mechanism of action of ACE inhibitors. The diagram should visually represent the normal conversion of angiotensin I to angiotensin II, and how ACE inhibitors inhibit this conversion. The diagram should highlight the decreased vasoconstriction and aldosterone release as a result of this inhibition.
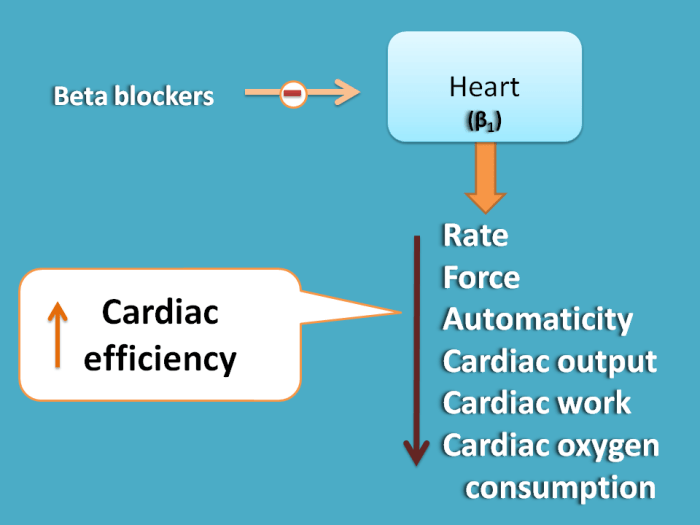
Mechanism of Action of Beta-Blockers
Beta-blockers reduce the effects of circulating catecholamines (epinephrine and norepinephrine) on the heart and blood vessels. This leads to a decreased heart rate, reduced force of contraction, and vasodilation, ultimately resulting in lower blood pressure.  Diagram Description: A diagram illustrating the mechanism of action of beta-blockers. The diagram should visually demonstrate the interaction of beta-blockers with beta-adrenergic receptors in the heart and blood vessels. It should illustrate the resultant decrease in heart rate and contractility, and the potential for vasodilation.
Diagram Description: A diagram illustrating the mechanism of action of beta-blockers. The diagram should visually demonstrate the interaction of beta-blockers with beta-adrenergic receptors in the heart and blood vessels. It should illustrate the resultant decrease in heart rate and contractility, and the potential for vasodilation.
Final Conclusion
In conclusion, choosing between ACE inhibitors and beta-blockers requires careful consideration of individual patient needs and circumstances. Factors like patient history, comorbidities, and lifestyle play a significant role. This comparison highlights the importance of a comprehensive understanding of both classes of medications to tailor treatment strategies for optimal cardiovascular health. Remember to always consult with a healthcare professional for personalized advice.

