How to use a glucometer is a crucial skill for anyone managing their blood sugar levels. This guide walks you through the entire process, from preparation to disposal, ensuring accurate readings and a better understanding of your health. We’ll cover different glucometer types, proper hand hygiene, and interpreting results, providing a complete picture for safe and effective glucose monitoring.
Understanding how to use a glucometer correctly is essential for accurate blood glucose readings. This detailed guide provides step-by-step instructions, along with explanations of important considerations, making the process easier and more reliable. We’ll cover everything from preparing your hands to interpreting your results, empowering you to take control of your blood sugar management.
Introduction to Glucometers
A glucometer is a small, handheld device used to measure the amount of glucose (sugar) in a person’s blood. It’s a crucial tool for individuals with diabetes, allowing them to monitor their blood sugar levels and make necessary adjustments to their diet and medication. Accurate blood glucose monitoring is essential for managing diabetes effectively and preventing serious health complications.The purpose of a glucometer is to provide real-time feedback on blood glucose levels, empowering individuals to take proactive steps to maintain healthy blood sugar ranges.
This information is vital for personalized diabetes management plans and enables individuals to make informed decisions about their health.
Different Types of Glucometers
Various glucometer types are available, each with unique features and functionalities. Understanding these differences helps individuals choose the most suitable device for their needs and preferences. The most common types include blood strip glucometers and lancet-free glucometers.
Blood Strip Glucometers
These traditional glucometers require a small blood sample obtained by pricking the fingertip with a lancet. The collected blood is then placed on a test strip, which is inserted into the glucometer. The device then measures the glucose concentration and displays the result.
Lancet-Free Glucometers
These innovative devices eliminate the need for finger pricks. Instead, they utilize alternative methods to obtain a blood sample, such as a small, painless skin puncture or a heel prick for infants or children. This feature is particularly beneficial for individuals who find finger pricks uncomfortable or for those with conditions that make frequent finger pricking challenging. The collected blood is then analyzed by the device, which provides the glucose reading.
General Steps in Using a Glucometer
Following the manufacturer’s instructions is crucial for accurate and reliable readings. Generally, the process involves these steps:
- Preparing the necessary materials, including the glucometer, test strips, lancets (for blood strip glucometers), and alcohol swabs.
- Cleaning the testing site with an alcohol swab to prevent infection.
- Pricking the fingertip (or alternative site for lancet-free devices) and obtaining a small blood sample.
- Placing the blood sample on the test strip.
- Inserting the test strip into the glucometer.
- Waiting for the glucometer to display the blood glucose level.
- Recording the result and noting the time of the test.
Comparison of Glucometer Types
| Feature | Blood Strip Glucometers | Lancet-Free Glucometers |
|---|---|---|
| Method of Blood Sampling | Finger prick using lancet | Non-invasive methods (e.g., skin puncture, heel prick) |
| Ease of Use | Generally straightforward, but can be uncomfortable for some | Potentially easier and less painful for some users |
| Cost | Typically more affordable | Generally more expensive |
| Accuracy | Generally comparable to lancet-free glucometers when used correctly | May have slightly higher variability in readings depending on the technology |
| Portability | Often compact and portable | May be larger or bulkier |
| Drawbacks | Can be painful and cause discomfort for some users | Might have limitations in specific user groups or situations |
| Features | Simple designs, often with basic functions | May offer advanced features like memory storage, or easier data transmission |
Preparing for a Glucometer Reading
Proper preparation is crucial for accurate blood glucose readings. Ignoring these steps can lead to inaccurate results, potentially impacting treatment decisions and overall health management. This section details the essential steps to ensure reliable and consistent readings.Accurate blood glucose monitoring is vital for managing diabetes effectively. Following the correct procedures for preparing for a reading minimizes errors and provides a more precise picture of blood sugar levels.
Importance of Hand Hygiene
Proper hand hygiene is paramount before performing a blood glucose test. Contamination from bacteria, dirt, or even residue from lotions can affect the accuracy of the test. Clean hands reduce the risk of introducing contaminants into the blood sample, ensuring a more reliable reading.
Cleaning the Test Strip and Glucometer
Ensuring the glucometer and test strip are clean before use is essential for accurate results. Any foreign material can interfere with the electrochemical process of the glucometer, leading to inaccurate readings.
- Clean the test strip with a soft, lint-free cloth. Avoid harsh scrubbing or abrasive materials that could damage the test strip’s surface.
- Carefully wipe the glucometer’s testing area and the surrounding area with a clean, damp cloth.
- Ensure that both the test strip and glucometer are completely dry before inserting the strip into the device.
Using the Correct Lancet and Depth
Selecting the appropriate lancet and inserting it at the correct depth is critical for obtaining a sufficient blood sample without causing excessive pain or injury. Using a lancet that is too small or inserting it too deeply can result in an insufficient blood sample, while using a lancet that is too large or inserting it too shallowly can cause discomfort and potential complications.
- Select a lancet that is appropriate for the user’s skin type and the glucometer model. Always refer to the manufacturer’s instructions for the recommended lancet size.
- Insert the lancet at the recommended depth for the glucometer. Excessive depth can lead to pain and potentially inaccurate readings. The correct depth is usually indicated on the lancet and the glucometer instruction manual.
- Ensure that the lancet is properly secured in the lancing device before use. Loose lancets may cause difficulty in obtaining a blood sample and can be painful.
Lancing the Finger: A Step-by-Step Procedure
The technique used for lancing the finger significantly affects the quality of the blood sample. A consistent and controlled approach minimizes pain and promotes accurate readings.
- Clean the testing site with an alcohol swab, allowing it to dry completely.
- Position the lancet correctly over the testing site. Avoid areas with visible veins or scars. Using the fleshy part of the fingertip is usually recommended.
- Gently press the lancing device to pierce the skin at the designated depth. Avoid excessive pressure, which can lead to discomfort.
- Allow the blood to flow freely onto the test strip, ensuring a sufficient amount for accurate testing.
- Remove the lancet and gently apply a small amount of gauze or cotton to the lanced area to stop any bleeding. Apply gentle pressure for a few seconds.
Performing the Test
Taking an accurate blood sugar reading is crucial for managing diabetes effectively. Following the correct procedures ensures reliable results and helps you make informed decisions about your health. This section details the precise steps involved in performing the test, from preparing the test strip to interpreting the results.
Inserting the Test Strip
The test strip is a vital component of the glucometer. Proper insertion ensures accurate readings. Carefully align the test strip with the designated slot in the glucometer. Avoid touching the testing area of the strip. Incorrect placement can lead to inaccurate results.
Applying the Lancet
A lancet is a small, sterile needle used to puncture the skin and collect a blood sample. Proper lancet application is essential for a quick and painless procedure. Select a suitable lancet and carefully apply it to the fingertip, ensuring the lancet is placed perpendicular to the skin.
Collecting the Blood Sample
Collecting the blood sample involves puncturing the fingertip and allowing a small amount of blood to collect on the test strip. The collected blood sample should be adequate for a reliable reading. Using a clean and sanitized fingertip will help in collecting a good quality sample.
Pressing the Blood Sample onto the Test Strip
Gently pressing the blood sample onto the test strip ensures the sample is absorbed correctly. Applying excessive pressure can cause the blood to spread unevenly. This will affect the accuracy of the reading. Press firmly enough to allow the sample to saturate the test strip, but avoid applying undue pressure.
Inserting the Test Strip into the Machine
After obtaining the blood sample, carefully insert the test strip into the designated slot in the glucometer. Ensuring the test strip is fully inserted and properly seated is vital for the machine to recognize the sample. The glucometer will typically have clear markings and indicators to guide the correct insertion.
Waiting for Results
The glucometer will automatically begin processing the sample. The device will display the result after a predetermined amount of time. Avoid disturbing the glucometer during this period to ensure an accurate reading. Observe the display carefully for the numerical result.
Potential Issues During Blood Collection and Solutions
| Issue | Solution |
|---|---|
| Insufficient blood sample | Ensure proper lancing technique. Try a different fingertip, ensuring it is clean and dry. |
| Blood sample is too large | Apply gentle pressure to the lancet to control the blood flow. |
| Blood sample is too small | Repeat the lancing procedure using a different finger or increasing the pressure slightly. |
| Blood sample has dried out | Discard the test strip and repeat the procedure with a new test strip and finger. |
| Blood sample is not fully absorbed | Apply gentle pressure to the test strip to help the blood sample absorb completely. If necessary, repeat the procedure with a new test strip. |
Interpreting the Results
Understanding your blood glucose readings is crucial for managing your diabetes effectively. Accurate interpretation helps you make informed decisions about your diet, activity levels, and medication. This section will guide you through deciphering your glucometer results and their significance.Interpreting your blood glucose results goes beyond simply looking at the number on the display. It involves understanding the context of your reading in relation to your overall health, meal timing, and physical activity.
This knowledge empowers you to adjust your lifestyle to maintain stable blood glucose levels.
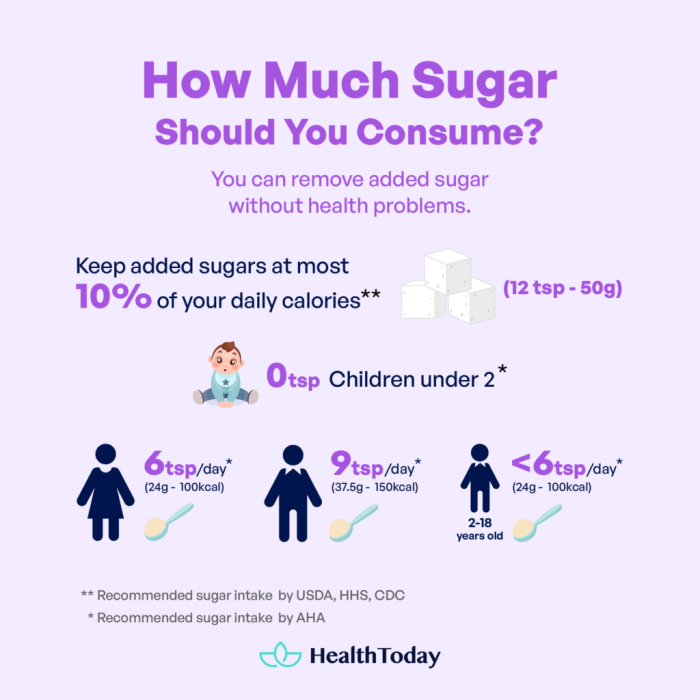
Understanding Target Blood Glucose Levels
Target blood glucose levels vary depending on individual needs and health conditions. It’s essential to discuss your target ranges with your doctor or healthcare professional. They can tailor recommendations based on your specific situation. Achieving and maintaining these targets is key to preventing complications associated with diabetes.
Blood Glucose Levels and Health Implications
Different blood glucose levels have different implications for your health. A table below provides a general guideline, but remember to consult your doctor for personalized recommendations.
| Blood Glucose Level (mg/dL) | Health Implications |
|---|---|
| Below 70 | Hypoglycemia (low blood sugar): Symptoms can include shakiness, dizziness, confusion, and sweating. Immediate action is required to raise blood sugar levels. |
| 70-99 | Normal range. This is a desirable range to maintain for optimal health. |
| 100-125 | Slightly elevated. May indicate a need for adjustments in diet or activity. Monitoring and consultation with a healthcare professional are advised. |
| 126-180 | Elevated. May require adjustments in diet, exercise, or medication. Frequent monitoring is important. |
| Above 180 | High blood sugar (hyperglycemia). Frequent high readings may indicate a need to adjust medication or dietary intake. Seek guidance from a healthcare professional. |
Consistent Monitoring of Blood Glucose Levels, How to use a glucometer
Consistent monitoring is vital for managing diabetes. Regular testing provides valuable insights into how your body responds to various factors. This allows for proactive adjustments to maintain stable blood glucose levels. Tracking your readings over time helps you identify patterns and trends that can influence your management strategy. A logbook or dedicated app can help you document these readings, allowing you to see how your blood glucose levels fluctuate throughout the day.
Learning how to use a glucometer accurately is crucial for managing blood sugar levels. It’s important to follow the specific instructions that come with your device, which usually involves pricking your finger, applying the test strip, and then placing the device onto the strip to get a reading. When choosing healthy alternatives to full fat dairy products, like those found at healthy alternatives to full fat dairy products , remember to check nutritional labels to ensure you’re not inadvertently increasing your blood sugar.
This awareness is just as important as knowing the proper procedure for taking a glucometer reading.
Interpreting Readings in Relation to Meals and Activities
Your blood glucose levels are affected by meals and physical activity. Readings taken after meals or after periods of strenuous activity can provide insights into how your body processes food and responds to exertion. Monitoring these readings allows you to understand the impact of your lifestyle choices on your blood glucose levels.
Understanding how your blood glucose reacts to specific foods and activities is a key component of effective diabetes management.
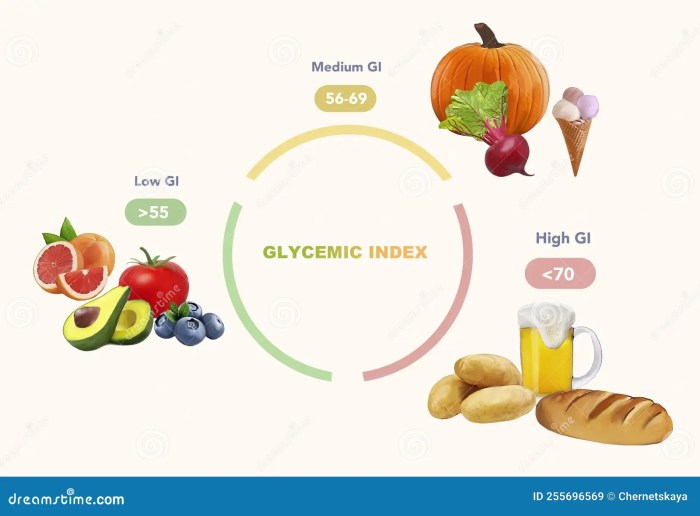
For example, a sudden increase in blood glucose after eating a high-carbohydrate meal may indicate the need to adjust portion sizes or consider the glycemic index of the foods consumed. Conversely, increased physical activity can lead to lower blood glucose levels. Recognizing these patterns helps you fine-tune your approach to maintain stable blood glucose levels.
Learning how to use a glucometer properly is crucial for managing blood sugar levels. It’s a simple process, really – just follow the instructions that come with your device. However, if you’re noticing unusual rashes on your child, especially if it’s accompanied by other symptoms like drooling or mouth sores, it’s essential to differentiate between drool rash and hand-foot-and-mouth disease.
For a detailed comparison, check out this helpful guide on drool rash vs hand foot mouth. Once you’ve got a better understanding of these conditions, you can focus back on using the glucometer effectively and accurately.
After the Test: How To Use A Glucometer
Taking care of your glucometer and its accessories after each use is crucial for accurate readings and maintaining a healthy lifestyle. Proper disposal, storage, and record-keeping are all essential steps to ensure the longevity of your device and the reliability of your blood glucose monitoring.Following the correct procedures after each test ensures your readings are precise and your health is well-managed.
A well-maintained glucometer is a key tool in your diabetes management journey.
Safe Disposal of Lancets and Test Strips
Proper disposal of used lancets and test strips is vital for safety and to prevent potential contamination. Never attempt to reuse these items, as this can introduce infection risks. Always follow the manufacturer’s instructions for disposal. Typically, used lancets are disposed of in a sharps container specifically designed for this purpose, and test strips should be placed in a sealed container according to the manufacturer’s instructions.
Never flush lancets or test strips down the toilet.
Proper Storage of Glucometer and Accessories
Maintaining the cleanliness and integrity of your glucometer and its components is essential. Store the glucometer in a cool, dry place, away from direct sunlight and extreme temperatures. Keep the lancets and test strips in their original packaging until ready for use, to preserve their quality and prevent contamination. Store them in a cool, dry place, away from direct sunlight.
If possible, keep the lancets and strips in the refrigerator to further prolong their life. This storage method is recommended by many manufacturers.
Maintaining Accurate Records of Blood Glucose Readings
Thorough record-keeping is essential for monitoring blood glucose levels and identifying trends. This information is invaluable for discussing your progress with your healthcare provider and adjusting your treatment plan as needed. Use a dedicated logbook or an app designed for blood glucose tracking. Record the date, time, reading, and any relevant information such as meals consumed, medication taken, or level of activity.
Checking your blood sugar with a glucometer is pretty straightforward. Just remember to clean the lancet and your fingertip, prick your finger gently, and then place the test strip in the device. Knowing how to properly use your glucometer is essential, but sometimes managing other health conditions, like a cortisone flare, what is a cortisone flare , can affect blood sugar levels.
So, if you’re experiencing any changes, it’s always a good idea to double-check your readings and consult your doctor.
Regular review of these records helps you to identify patterns in your blood sugar levels.
Cleaning the Glucometer
Cleaning your glucometer regularly is important to prevent contamination and ensure accurate readings. Use a soft, damp cloth to wipe the device clean, avoiding harsh chemicals or abrasive materials. Do not submerge the glucometer in water. The manufacturer’s instructions should provide specific cleaning guidelines. Adhering to the manufacturer’s instructions will help ensure the glucometer remains in excellent working condition.
Following Manufacturer’s Instructions
Always prioritize following the manufacturer’s instructions for optimal performance and safety. This ensures that the device is used correctly, preventing potential errors in readings and potential damage to the equipment. These instructions are designed to help you achieve accurate readings and maintain the integrity of your glucometer. The manufacturer’s instructions will often include information on cleaning, storage, and disposal.
Troubleshooting Common Glucometer Issues
Sometimes, glucometers may exhibit unexpected behavior. Here are some potential troubleshooting steps for common issues:
- Incorrect Readings: If you suspect your readings are inaccurate, check the test strip expiration date, ensure the lancet is properly inserted, and verify that the device is functioning correctly. If the issue persists, consult your healthcare provider.
- Low Battery: A low battery can affect the glucometer’s performance. Replace the battery according to the manufacturer’s instructions.
- Clogged Test Strip Port: If the test strip port is clogged, clean it with a soft, damp cloth.
- Incorrect Calibration: If the device displays an error message or readings seem inconsistent, check if the glucometer needs calibration. Contact the manufacturer or your healthcare provider for assistance.
Special Considerations
Mastering glucometer use goes beyond the basic steps. Understanding how to adapt to different needs, from children’s unique requirements to the elderly’s potential challenges, is crucial for accurate and effective blood glucose monitoring. This section dives deeper into special considerations for optimal glucometer use.
Glucometer Use for Children and the Elderly
Children and the elderly often require specific adjustments to the glucometer process. Children may have smaller fingers, requiring a different lancing depth or a different lancing device. Elderly individuals might have reduced dexterity, potentially impacting their ability to handle the glucometer and lancing device. Careful consideration of these factors ensures accurate readings and minimal discomfort.
Adjusting the Glucometer for Different User Needs
Glucometers offer various features designed for individual needs. Some glucometers have larger displays or simplified interfaces for individuals with visual impairments or dexterity issues. Options for different lancing depths are available for individuals with thinner skin or more sensitive areas. Choosing a glucometer that best suits the individual’s needs can improve the overall experience and accuracy of blood glucose monitoring.
Addressing Concerns or Questions about Glucometer Use
If you have concerns or questions about glucometer use, consult your healthcare provider or a certified diabetes educator. They can provide personalized guidance and address any specific concerns you may have. They can also help you select the appropriate glucometer for your needs and provide ongoing support.
Comparison of Glucometers for Various Needs and Conditions
Different glucometers cater to various needs. Some models offer faster testing times, while others feature more detailed results. For individuals with limited dexterity, glucometers with larger buttons or simplified interfaces might be preferable. The best glucometer depends on the individual’s specific needs and preferences. Consider factors such as ease of use, accuracy, and features when making your selection.
| Glucometer Feature | Description | Benefit for Specific Needs |
|---|---|---|
| Large Display | Clear, easy-to-read display | Beneficial for individuals with visual impairments or those who prefer a clear view of results |
| Simplified Interface | Intuitive and easy-to-understand controls | Useful for individuals with dexterity issues or those new to glucometer use |
| Fast Testing Time | Rapid results | Beneficial for those who need quick results or prefer not to wait long |
Specific Considerations for Diabetes Management
Accurate blood glucose monitoring is paramount in diabetes management. Regular testing, coupled with lifestyle adjustments, plays a significant role in controlling blood sugar levels and preventing complications. Consistency is key; regular testing times, and using the same glucometer for consistent results, are vital for effective diabetes management. For example, a patient with Type 1 diabetes might need to test more frequently than someone with Type 2 diabetes.
Adjustments must be made based on individual needs.
“Regular and consistent blood glucose monitoring is essential for effective diabetes management.”
Visual Aids and Examples
Understanding how to use a glucometer effectively involves more than just the steps; it’s about grasping the tools and processes involved. Visual aids can significantly enhance this understanding, making the entire procedure clear and straightforward. This section will provide detailed descriptions of the glucometer, demonstrate proper technique, and illustrate the complete testing process.The visual aids are designed to supplement the written instructions, ensuring a comprehensive understanding of the glucometer’s use.
Glucometer Components and Functions
Glucometers are handheld devices that measure blood glucose levels. A typical glucometer comprises a testing strip reader, a lancing device (often integrated), and a small display screen. The testing strip contains chemicals that react with blood, producing a measurable electrical signal. The display screen shows the glucose level in milligrams per deciliter (mg/dL). Some models also include memory functions, graphs for tracking glucose trends, and alarms.
Proper Finger-Pricking Technique
Proper finger-pricking technique is critical for accurate readings and preventing injury. A lancet, a small, disposable blade, pierces the skin to obtain a blood sample. Select a fingertip with good blood flow, typically the side of the finger, avoiding the fingertip’s center. Apply a small amount of antiseptic to the puncture site. Apply gentle but firm pressure with the lancing device to the selected area, ensuring the lancet is properly aligned.

The image above shows the correct technique: choosing the fingertip, cleaning the area, and gently pressing the lancing device to create a small puncture wound.
Test Strip Placement
The test strip is designed with specific locations for blood sample collection. Ensure the blood sample adheres to the designated area on the test strip. Carefully insert the test strip into the glucometer, aligning it correctly with the designated slots. This is usually a straightforward process; however, it’s crucial to match the strip’s positioning with the glucometer’s specific design.

The image depicts the proper alignment of the test strip within the glucometer slots, ensuring accurate reading results.
Complete Testing Process
The complete process, from preparation to disposal, is Artikeld below.
- Preparation: Cleanse the fingertip with an antiseptic wipe. Wait for the antiseptic to dry completely. Use a lancet to puncture the fingertip.
- Blood Sample: Allow a drop of blood to form on the test strip. Ensure the blood sample completely covers the designated area.
- Insertion: Insert the test strip into the glucometer and close the lid. The glucometer will automatically process the reading.
- Reading: The glucometer will display the blood glucose level.
- Disposal: Dispose of the used test strip and lancet in a designated sharps container.
Glucometer Model Comparison
Different glucometer models vary in features, ease of use, and price. Here’s a table showcasing some key differences:
| Feature | Model A | Model B | Model C |
|---|---|---|---|
| Ease of Use | High | Medium | Low |
| Accuracy | Excellent | Good | Excellent |
| Price | Moderate | Low | High |
| Memory Function | Yes | No | Yes |
This table illustrates a general comparison. Specific features and values may differ based on the manufacturer and model.
Ending Remarks

In conclusion, mastering the art of glucometer use empowers you to effectively manage your blood glucose levels. By following these steps and consistently monitoring your readings, you gain valuable insights into your health and make informed decisions for your well-being. Remember to always consult with a healthcare professional for personalized advice and to address any specific concerns.