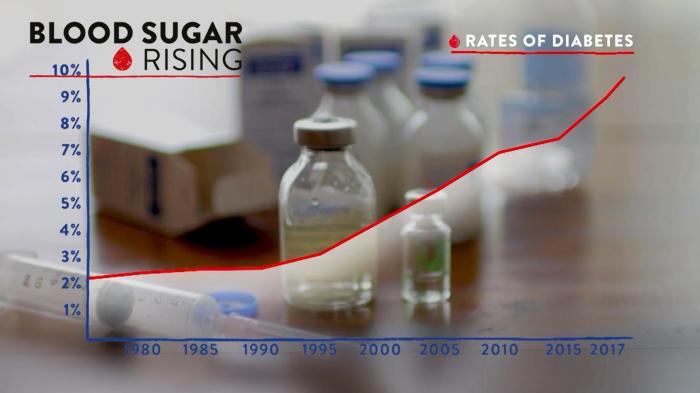
How much protein should a person with diabetes eat? This crucial question impacts blood sugar management, and the answer isn’t one-size-fits-all. Different protein sources affect blood glucose differently, and individual needs vary based on factors like age, activity, and type of diabetes. Understanding the nuances of protein intake for diabetes is key to maintaining optimal health.
This guide delves into the role of protein in diabetes management, offering practical advice on recommended intakes, incorporating protein into meals, and understanding potential interactions. We’ll explore different protein sources, their impact on blood sugar, and strategies for managing blood glucose levels while enjoying a balanced diet.
Understanding Dietary Needs for Diabetes
Protein plays a crucial role in managing blood sugar levels for individuals with diabetes. It’s not just about the quantity of protein, but also the quality and how it interacts with other nutrients in the diet. Understanding the impact of different protein sources on blood glucose response is essential for creating a personalized meal plan that supports healthy blood sugar control.
This knowledge empowers individuals to make informed choices that contribute to their overall well-being.Protein’s role in blood sugar management is multifaceted. It contributes to a feeling of fullness, which can help regulate appetite and prevent large fluctuations in blood glucose. Furthermore, protein slows down the absorption of carbohydrates, preventing rapid spikes in blood sugar after meals. This controlled release of glucose into the bloodstream is a significant benefit for managing diabetes.
Protein Sources and Blood Glucose Response
Different protein sources have varying effects on blood glucose levels. The glycemic index (GI) of a food indicates how quickly it raises blood sugar. Proteins from lean sources tend to have a lower impact on blood sugar compared to processed or high-fat proteins.
Comparison of Protein Sources
This table summarizes the protein content, glycemic index (GI), and potential side effects of various protein sources for individuals with diabetes. Note that GI values can vary based on preparation methods and individual factors.
| Protein Source | Protein Content (grams per 100g) | Approximate Glycemic Index | Potential Side Effects (for individuals with diabetes) |
|---|---|---|---|
| Lean Meats (chicken breast, fish, turkey) | 20-30 | Low | Generally well-tolerated, can be a good source of essential nutrients. |
| Beans and Lentils | 15-25 | Moderate | May cause digestive discomfort in some individuals, rich in fiber. |
| Tofu | 8-15 | Low | Good source of plant-based protein, may have a slightly higher GI if processed with high-sodium ingredients. |
| Eggs | 13 | Low | Excellent source of protein and essential nutrients, should be consumed in moderation as part of a balanced diet. |
| Dairy Products (Greek Yogurt, Milk) | 10-18 | Low | Can be part of a healthy diet, but high-fat dairy products might have a slightly higher GI. |
| Processed Meats (sausages, bacon) | 20-30 | Moderate to High | Often high in saturated fat and sodium, should be consumed in moderation. |
Protein Intake and Blood Sugar Control
The amount of protein needed by an individual with diabetes varies based on factors like activity level, age, and overall health. It’s essential to work with a registered dietitian or healthcare professional to determine the appropriate protein intake for optimal blood sugar management. A balanced diet with an appropriate amount of protein, along with regular exercise and medication (if applicable), is crucial for effective diabetes management.
It’s also important to consider portion sizes and to combine protein with fiber-rich foods to further control blood glucose levels. For example, a person with type 2 diabetes might benefit from including a serving of beans with lean chicken or fish to create a balanced meal that promotes healthy blood sugar control.
Recommended Protein Intake for People with Diabetes
Protein is a crucial macronutrient for people with diabetes, playing a vital role in blood sugar management, satiety, and overall health. It helps to stabilize blood glucose levels by slowing down the absorption of carbohydrates and promoting a feeling of fullness, which can prevent overeating. Proper protein intake is essential for maintaining muscle mass, particularly important for people with diabetes who may experience muscle loss due to the disease or its treatments.While the general recommendation for protein intake remains consistent across populations, variations in individual needs exist.
Factors like age, activity level, and type of diabetes influence how much protein an individual with diabetes should consume. A personalized approach, guided by a healthcare professional, is vital to ensure optimal health outcomes.
General Dietary Recommendations for Protein
Adequate protein intake is essential for maintaining muscle mass and overall health. For individuals with diabetes, the recommended daily protein intake generally falls within the range of 15% to 20% of total daily caloric intake. This range aligns with the recommended dietary allowance for the general population and accounts for the specific needs of people with diabetes. Individual needs may vary depending on the factors mentioned above.
Protein Intake Variations Based on Factors
Protein requirements vary based on several factors. Age significantly impacts protein needs, with older adults often requiring a higher protein intake to maintain muscle mass and prevent age-related decline. Similarly, activity level influences protein requirements, as athletes and individuals engaging in strenuous physical activity will need more protein to support muscle repair and growth. The type of diabetes also plays a role; for example, individuals with type 1 diabetes might require slightly higher protein intakes compared to those with type 2, depending on individual circumstances.
Recommended Daily Protein Intake
The following table provides a general guideline for protein intake based on age and activity level. Remember, these are estimates and should be personalized by a registered dietitian or healthcare professional.
| Age Group | Sedentary | Moderately Active | Highly Active |
|---|---|---|---|
| 19-30 | 0.8 g/kg | 1.0-1.2 g/kg | 1.2-1.6 g/kg |
| 31-50 | 0.8 g/kg | 1.0-1.2 g/kg | 1.2-1.6 g/kg |
| 51+ | 1.0 g/kg | 1.2-1.4 g/kg | 1.4-1.8 g/kg |
Note: 1 kg = 2.2 pounds. Consult with a healthcare professional to determine your individual needs.
Importance of Professional Consultation
Making significant dietary changes, particularly when managing a chronic condition like diabetes, requires careful consideration. It is crucial to consult a registered dietitian or healthcare professional before making any substantial changes to your diet, including adjusting protein intake. They can assess your individual needs, medical history, and current health status to provide personalized recommendations and ensure safety and effectiveness.
This personalized approach is critical to avoid potential complications and achieve optimal health outcomes.
Figuring out how much protein a person with diabetes should eat can be tricky. While a balanced diet is key, it’s important to consider portion sizes and the overall impact on blood sugar levels. For instance, understanding the nutritional value of snacks and side dishes like pickles can influence your choices. Want to know if pickles are a healthy addition to your weight loss plan?
Check out this article on are pickles good for weight loss. Ultimately, consulting a registered dietitian or your doctor is crucial for personalized dietary advice on protein intake for diabetes management.
Protein and Blood Sugar Management Strategies
Protein plays a crucial role in blood sugar control for individuals with diabetes. It helps slow down the absorption of carbohydrates, preventing rapid spikes in blood glucose levels. By incorporating protein strategically into meals and snacks, individuals can achieve better blood sugar regulation and overall health.Protein’s impact on blood sugar management stems from its effect on digestion. Unlike carbohydrates, which are quickly broken down into glucose, protein takes longer to digest.
This extended digestion time helps to moderate the release of glucose into the bloodstream, preventing those sharp, unwanted peaks. This more gradual release of glucose allows for better blood sugar control.
Strategies for Incorporating Protein
Protein is a valuable component of a diabetes management plan. To maximize its benefits in maintaining stable blood sugar, it’s essential to incorporate it strategically into meals and snacks. Here are some effective strategies:
- Prioritize protein at the start of your meal: Eating protein first can help slow down the absorption of carbohydrates consumed later in the meal. This can lead to a more gradual increase in blood sugar levels.
- Combine protein with complex carbohydrates: Pairing protein with complex carbohydrates like whole grains, vegetables, and legumes creates a balanced meal. The protein helps regulate the release of glucose from the carbohydrates, preventing blood sugar spikes.
- Include protein in snacks: Protein-rich snacks can help prevent blood sugar crashes between meals. Examples include Greek yogurt with berries, a handful of almonds, or a hard-boiled egg.
- Choose lean protein sources: Lean protein sources like fish, poultry without skin, and beans are preferable to fatty cuts of meat. These choices offer the necessary protein without excess fat, which can contribute to blood sugar fluctuations.
- Pay attention to portion sizes: While protein is beneficial, overconsumption can also have negative effects. Maintaining appropriate portion sizes is crucial for effective blood sugar management.
Balanced Meal Plans, How much protein should a person with diabetes eat
Creating balanced meal plans that incorporate protein sources appropriate for managing blood sugar requires careful consideration. These meal plans should promote stable blood sugar levels while providing the necessary nutrients.
| Meal | Protein Source | Carbohydrate Source | Vegetable Source |
|---|---|---|---|
| Breakfast | Scrambled eggs with spinach and whole-wheat toast | Whole-wheat toast | Spinach |
| Lunch | Grilled chicken salad with mixed greens and quinoa | Quinoa | Mixed greens, cucumber, tomatoes |
| Dinner | Baked salmon with roasted vegetables | Sweet potato | Broccoli, carrots |
Portion Control
Portion control is essential for effective blood sugar management when consuming protein-rich foods. Overconsumption of protein, like any other nutrient, can have negative consequences. Understanding appropriate portion sizes is crucial for maintaining a healthy balance. By controlling portions, you can effectively manage your blood sugar levels and support your overall health.
A general guideline is to aim for a portion of protein that fills about one-fourth of your plate.
Protein in Different Diets
Protein can be incorporated into various dietary approaches while maintaining blood sugar control.
- Vegetarian Diet: Vegetarian diets can easily incorporate protein from sources like tofu, lentils, beans, and chickpeas. These sources provide sufficient protein without animal products. For example, a lentil soup with whole-wheat bread would be a balanced meal.
- Vegan Diet: Vegan diets, similar to vegetarian diets, rely on plant-based protein sources. This includes a variety of legumes, nuts, seeds, and soy products. For instance, a vegan chili with brown rice offers a complete protein meal.
- Mediterranean Diet: The Mediterranean diet emphasizes lean protein sources like fish, poultry, and beans. It also includes healthy fats and plenty of vegetables and fruits. This diet’s focus on whole foods helps to manage blood sugar levels effectively.
Potential Interactions and Considerations
Navigating the delicate balance of protein intake for diabetes management requires careful consideration of potential interactions with other medications and lifestyle factors. Understanding these interactions is crucial for preventing adverse effects and optimizing blood sugar control. This section delves into potential pitfalls and strategies for mitigating them.
Potential Interactions with Medications
Certain medications used to manage diabetes, such as some blood pressure medications or diuretics, can interact with protein intake. These interactions might affect how the body absorbs or processes protein, potentially impacting blood sugar levels. For example, some medications can reduce the body’s ability to absorb amino acids, impacting protein synthesis and thus, the overall effect on blood sugar.
Consulting a doctor or registered dietitian is essential to discuss any potential interactions between your protein intake and your current medication regimen.
Potential Side Effects of High Protein Intake
While protein is essential, consuming excessively high amounts can lead to potential side effects. Kidney strain is a significant concern. Individuals with pre-existing kidney conditions may experience heightened risks. In some cases, high protein intake might lead to an increase in uric acid levels, potentially contributing to gout. Furthermore, some individuals might experience digestive issues, such as bloating or gas, particularly if the protein source is not well-tolerated.
Importance of Monitoring Blood Sugar Levels
Monitoring blood sugar levels after consuming protein-rich meals is crucial for personalized diabetes management. The impact of protein on blood sugar levels varies from person to person, and individual responses differ. Tracking blood sugar levels after meals containing protein allows for adjustments to dietary strategies and medication to maintain optimal blood sugar control.
Table: Potential Side Effects and Management Strategies
| Potential Side Effect | Description | Management Strategies |
|---|---|---|
| Kidney Strain | Increased workload on the kidneys due to excess protein processing. | Maintaining a balanced protein intake, monitoring kidney function with regular checkups, and adjusting protein intake as needed. This is crucial for those with pre-existing kidney conditions. |
| Increased Uric Acid Levels | Elevated uric acid levels, potentially leading to gout. | Limiting intake of high-purine foods (some protein sources are higher in purines), staying hydrated, and consulting a doctor for potential medication adjustments. |
| Digestive Issues (Bloating/Gas) | Discomfort due to poorly digested protein. | Identifying and avoiding protein sources that cause discomfort, gradually increasing protein intake, and choosing well-tolerated protein sources. |
| Blood Sugar Fluctuations | Unpredictable blood sugar changes after protein-rich meals. | Monitoring blood sugar levels post-meal, adjusting carbohydrate intake to balance protein, and consulting with a dietitian to develop a personalized meal plan. |
Protein-Rich Food Examples and Recipes
Choosing protein-rich foods is crucial for people with diabetes to maintain stable blood sugar levels. Protein helps regulate blood sugar by slowing down the absorption of carbohydrates into the bloodstream. This gradual release prevents sharp spikes in blood glucose, making it easier to manage diabetes effectively. Finding delicious and satisfying protein sources is essential for a healthy and balanced diet.
Figuring out the right amount of protein for someone with diabetes can be tricky. While a balanced diet is key, the impact of sleep apnea on blood sugar levels needs consideration. Recent research suggests that getting a good night’s sleep, often improved by treatments like an implant for sleep apnea , can have a significant positive effect on insulin sensitivity, which directly relates back to how much protein a person with diabetes should consume.
Ultimately, consulting a doctor or registered dietitian is the best approach to determine the optimal protein intake for individual needs.
Protein-Rich Foods for Diabetes Management
A variety of protein sources are beneficial for individuals with diabetes. Lean meats, poultry without skin, fish, beans, lentils, tofu, and nuts are all excellent choices. These foods provide essential amino acids needed for bodily functions while helping to control blood sugar. Crucially, selecting protein sources low in saturated and unhealthy fats is important for overall cardiovascular health, a concern often linked to diabetes.
Simple and Healthy Recipes
Here are a couple of simple and healthy recipes incorporating protein-rich ingredients, designed to support blood sugar management:
Grilled Salmon with Roasted Asparagus and Quinoa
This recipe provides a balanced meal with lean protein, healthy fats, and complex carbohydrates.
- Grilled Salmon (4 oz): Provides a good source of protein and omega-3 fatty acids, beneficial for heart health and blood sugar regulation.
- Roasted Asparagus (1 cup): A low-calorie vegetable rich in vitamins and minerals, contributing to overall health and a low glycemic index.
- Quinoa (1/2 cup cooked): A complete protein and complex carbohydrate source, providing sustained energy release.
Instructions: Marinate salmon fillets in lemon juice, herbs, and spices. Roast asparagus with olive oil and salt/pepper. Cook quinoa according to package directions. Combine the grilled salmon, roasted asparagus, and quinoa for a complete meal.
Nutritional Information (Approximate):
- Protein: Approximately 30 grams
- Carbohydrates: Approximately 30 grams
- Fat: Approximately 15 grams
Chicken Stir-Fry with Brown Rice
This recipe offers a quick and flavorful way to enjoy protein and fiber.
- Chicken Breast (4 oz): A lean protein source that provides essential amino acids.
- Mixed Vegetables (1 cup): Provides essential vitamins, minerals, and fiber.
- Brown Rice (1/2 cup cooked): A complex carbohydrate that provides sustained energy and fiber.
Instructions: Cut chicken into bite-sized pieces. Stir-fry vegetables with a small amount of oil. Add chicken and cook until done. Serve over brown rice.
Nutritional Information (Approximate):
- Protein: Approximately 35 grams
- Carbohydrates: Approximately 40 grams
- Fat: Approximately 10 grams
Protein-Rich Food Nutritional Values
The table below provides a glimpse of the nutritional content of various protein-rich foods suitable for people with diabetes. This data highlights the variety of options available.
| Food | Protein (grams/100g) | Carbohydrates (grams/100g) | Fat (grams/100g) |
|---|---|---|---|
| Chicken Breast (lean) | 30 | 0 | 5 |
| Salmon | 20 | 0 | 15 |
| Lentils | 25 | 15 | 2 |
| Tofu | 8 | 2 | 1 |
| Eggs | 13 | 1 | 11 |
Addressing Specific Dietary Concerns

Navigating dietary needs for diabetes can be complex, especially when considering individual differences and specific health conditions. This section delves into tailoring protein intake strategies for various situations, from different types of diabetes to pregnancy and kidney disease. Understanding these nuances is crucial for effective blood sugar management and overall well-being.Addressing dietary concerns requires a personalized approach, acknowledging the unique needs of individuals with diabetes.
This includes considering factors like pre-existing conditions, cultural backgrounds, and personal preferences. Proper guidance and education are vital for successful dietary management.
Protein Intake for Different Types of Diabetes
Individuals with type 1 diabetes require consistent protein intake to maintain muscle mass and support overall health. Maintaining a balanced diet that includes appropriate amounts of protein is crucial. Type 2 diabetes management often involves careful monitoring of carbohydrate intake, but protein remains an important component of a healthy diet. The focus shifts to controlling carbohydrate and fat intake while maintaining sufficient protein.
Figuring out the right amount of protein for someone with diabetes can be tricky. While a balanced diet is key, the latest weight loss drug saxenda liraglutide latest weight loss drug saxenda liraglutide might also influence protein needs. Ultimately, consulting a doctor or registered dietitian is best to determine the optimal protein intake for your individual diabetes management plan.
Protein Needs During Pregnancy with Diabetes
Pregnant women with diabetes require increased protein intake to support the growing fetus and the mother’s own needs. The exact amount depends on individual factors, including pre-pregnancy weight, activity level, and the severity of the diabetes. A registered dietitian can provide tailored recommendations. Protein is essential for fetal development and maternal health during pregnancy. Adequate protein intake supports growth and development of the fetus and also helps maintain the mother’s health.
Protein-Rich Foods for Diverse Diets
A wide array of protein-rich foods caters to diverse cultural backgrounds and dietary preferences. These foods can be incorporated into meals and snacks in a variety of ways.
- South Asian Cuisine: Lentils, chickpeas, tofu, paneer (Indian cheese), and various dals are excellent protein sources. These are common ingredients in South Asian dishes and can be easily integrated into a diabetes-friendly diet. These options offer a balance of protein and fiber, which is beneficial for managing blood sugar levels.
- Mediterranean Diet: Fish, poultry, beans, and nuts provide protein in the context of a Mediterranean diet. The Mediterranean diet is rich in fruits, vegetables, and healthy fats, which contribute to overall health and can be easily integrated into a diabetes-friendly diet.
- Vegan Options: Tofu, tempeh, lentils, beans, and quinoa are readily available and nutritious sources of plant-based protein for individuals with diabetes who follow a vegan diet. These foods provide essential amino acids and fiber.
Protein Selection for Kidney Disease and Diabetes
Individuals with kidney disease and diabetes need to carefully select protein sources due to the kidneys’ reduced ability to filter waste products. The recommended protein intake is often lower than for those without kidney disease. Consult a nephrologist or registered dietitian to determine the appropriate protein intake and the best protein sources. Protein restriction is a common strategy to help manage kidney function.
It’s essential to find protein sources that are not too high in phosphorus and potassium.
| Protein Source | Considerations |
|---|---|
| Lean meats (chicken, fish) | Choose lean cuts and limit processed meats. |
| Eggs | Moderate consumption is generally acceptable. |
| Dairy products | Choose low-fat options and be mindful of potassium content. |
| Legumes | Good source of protein and fiber, but can be high in potassium. |
Monitoring and Adjusting Protein Intake: How Much Protein Should A Person With Diabetes Eat
Fine-tuning your protein intake is a crucial aspect of diabetes management. It’s not a one-size-fits-all approach; your body’s response to protein varies, and careful monitoring is essential for maintaining healthy blood sugar levels. Adjusting your protein intake requires a personalized strategy based on your individual needs and how your body reacts.Understanding how your body responds to different protein levels is key to effective blood sugar control.
This involves monitoring blood glucose after meals and snacks high in protein and adjusting your intake accordingly. Consistency in monitoring and appropriate adjustments are essential for maintaining optimal health.
Importance of Monitoring Blood Sugar Levels
Monitoring blood sugar levels after consuming protein-rich meals or snacks is critical for understanding your body’s individual response. This allows you to identify patterns and adjust your intake to prevent spikes or dips in blood glucose. Tracking these responses helps tailor your protein intake to your unique metabolic needs. The data collected helps you and your healthcare provider make informed decisions about your diet.
Methods of Adjusting Protein Intake
Adjusting protein intake involves a multifaceted approach. This includes paying attention to how your body reacts to different amounts of protein and making gradual, measured changes. Consider incorporating a variety of protein sources to ensure adequate nutrition. It’s crucial to maintain a balanced diet, not just focus on protein.
Step-by-Step Guide for Gradual Adjustments
A gradual approach to adjusting protein intake is recommended. Start by making small, incremental changes to your protein intake. For instance, if you typically consume 60 grams of protein daily, increase it to 65 grams for a week, then observe your blood glucose levels. Monitoring your blood sugar response is key to determining if this increase is appropriate for you.
If there are no significant changes, you can increase it further gradually. Conversely, if you notice a pattern of elevated blood sugar, decrease your protein intake slightly. Regular check-ups with your doctor are essential for guidance and support.
Significance of Regular Check-ups
Regular check-ups with your doctor or healthcare professional are paramount. They provide personalized guidance, assess your progress, and adjust your protein intake strategy based on your individual needs. Your doctor can also offer valuable insights into how your body is responding to the changes. A healthcare professional can identify any potential issues and recommend necessary adjustments to your plan.
Regular check-ups ensure that your approach to protein intake is always aligned with your overall health goals and blood glucose management.
Example of a Monitoring Strategy
Suppose you notice a blood sugar spike after consuming a meal high in protein. In this case, you could reduce the portion size of protein or choose a different protein source for that meal. Experiment with different protein sources and amounts to determine your body’s individual response. If the spike persists, consult your healthcare provider for personalized guidance.
By diligently monitoring your blood sugar levels and adjusting your protein intake accordingly, you can effectively manage your diabetes and maintain a healthy lifestyle.
Summary
In conclusion, managing protein intake is an essential part of diabetes care. By understanding the impact of different protein sources, tailoring intake to individual needs, and monitoring blood sugar levels, individuals with diabetes can effectively manage their condition and maintain a healthy lifestyle. Remember to consult a healthcare professional for personalized advice.





 (Note: A visual flowchart depicting the decision-making process, such as the one above, would ideally be included here. However, I cannot create images.)
(Note: A visual flowchart depicting the decision-making process, such as the one above, would ideally be included here. However, I cannot create images.)![Converting 100g Of Sugar To Cups [+ CALCULATOR] Sugar replacements for diabetics](https://lyricapills.com/wp-content/uploads/2025/06/Hidden-sugars-Food-with-sugar-1.jpg)