Chemotherapy physical decline older breast cancer patients faces unique challenges as aging impacts treatment tolerance and response. This comprehensive exploration delves into the physiological changes that affect chemotherapy’s efficacy and the resulting physical decline in older breast cancer patients. We’ll examine common side effects, discuss how age influences chemotherapy response and toxicity, and explore strategies for managing the physical symptoms and promoting well-being.
From understanding the impact of age on metabolism and organ function to identifying crucial nutritional considerations, this article provides a multi-faceted perspective on this critical issue. We’ll also review support systems and interventions, alongside illustrative case studies, to offer a realistic and insightful understanding of the challenges and management approaches for this vulnerable patient population.
Introduction to Chemotherapy-Related Physical Decline in Older Breast Cancer Patients
Older breast cancer patients facing chemotherapy treatment encounter unique challenges. The physiological changes associated with aging significantly impact how the body tolerates the aggressive therapies. Understanding these challenges is crucial for developing individualized treatment plans that maximize efficacy while minimizing adverse effects. This article delves into the specific considerations for older adults undergoing chemotherapy, focusing on the impact of aging on chemotherapy tolerance and the need for personalized approaches.The aging process brings about numerous physiological changes that can affect a person’s response to chemotherapy.
Muscle mass often diminishes, leading to decreased strength and endurance. Bone density can decrease, making bones more susceptible to fractures. The function of organs like the kidneys and liver may decline, impacting the body’s ability to process and eliminate chemotherapy drugs. These age-related changes can increase the risk of complications and side effects from chemotherapy.
Physiological Changes Affecting Chemotherapy Tolerance in Older Adults
Age-related changes in organ function, muscle mass, and bone density significantly influence the efficacy and safety of chemotherapy. Older adults may experience a slower metabolism, affecting how quickly their bodies process chemotherapy drugs. This can lead to higher drug concentrations in the blood, increasing the risk of side effects. Reduced kidney function can impair the excretion of chemotherapy drugs, further increasing the potential for toxicity.
Changes in the cardiovascular system can also affect how the heart responds to the stress of chemotherapy.
Common Chemotherapy Side Effects and Their Impact on Older Adults
Chemotherapy drugs are designed to target rapidly dividing cells, but this broad action can harm healthy cells, leading to a range of side effects. Common side effects include nausea, vomiting, fatigue, hair loss, and mouth sores. These side effects can be particularly challenging for older adults due to their existing health conditions and potential for functional decline. Furthermore, some side effects, like neuropathy (nerve damage), can be more debilitating in older individuals, potentially impacting mobility and daily activities.
Individualized Treatment Plans for Older Breast Cancer Patients
Recognizing the unique needs of older breast cancer patients is paramount. Treatment plans should be tailored to consider the patient’s overall health, functional status, and co-morbidities. Careful consideration of the patient’s ability to tolerate chemotherapy, alongside other treatment options, is essential. This personalized approach prioritizes quality of life and maximizes the effectiveness of treatment while minimizing adverse effects.
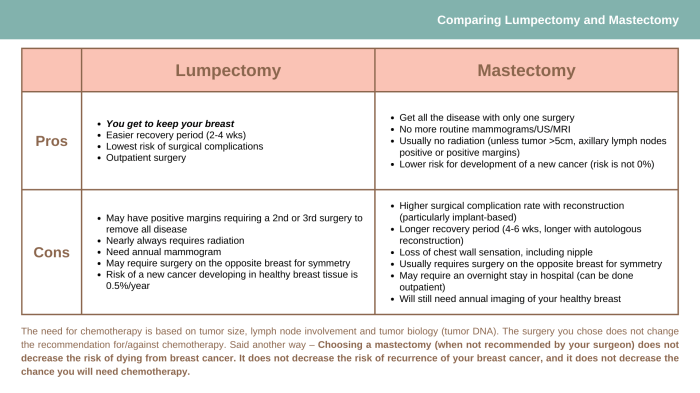
Comparison of Chemotherapy Side Effects Across Different Age Groups
| Side Effect | Older Adults (65+) | Younger Adults (18-64) |
|---|---|---|
| Nausea and Vomiting | Potentially more severe and prolonged; may require higher doses of antiemetics; susceptibility to dehydration. | Generally manageable with standard antiemetic regimens. |
| Fatigue | Can be profound and debilitating, significantly impacting daily activities. | Often manageable with rest and supportive care. |
| Hair Loss | May be more noticeable and prolonged. | Usually temporary and regrows after treatment. |
| Mouth Sores | Can be severe and painful, impacting nutrition and quality of life. | Generally less severe than in older adults. |
| Neuropathy | Increased risk and potential for more severe symptoms, affecting mobility and daily functioning. | Generally less severe than in older adults, though can still be problematic. |
| Cardiotoxicity | Increased risk and potential for more severe cardiac issues due to pre-existing conditions. | Generally lower risk, though cardiac monitoring is still important. |
This table provides a general comparison. Individual responses to chemotherapy vary significantly. Clinicians must carefully assess each patient’s specific situation and adjust treatment plans accordingly. Factors such as pre-existing health conditions, current functional abilities, and overall health status should be taken into account to optimize treatment outcomes and quality of life.
Impact of Age on Chemotherapy Response and Toxicity
Navigating the complexities of chemotherapy for older adults requires a nuanced understanding of how age affects treatment efficacy and potential side effects. This is particularly crucial for breast cancer patients, as aging often brings physiological changes that can impact the body’s ability to handle the rigors of chemotherapy. This blog post will delve into the specific ways age influences chemotherapy response and toxicity, offering insights into the considerations for older breast cancer patients undergoing treatment.Age significantly impacts the body’s ability to process and eliminate chemotherapy drugs.
This is largely due to changes in organ function, particularly in the liver and kidneys. These organs play critical roles in metabolizing and excreting medications, and their efficiency declines with age. Consequently, older patients may experience higher drug concentrations in their bloodstream, increasing the risk of adverse effects.
Age-Related Changes in Drug Metabolism
The liver and kidneys are vital for processing chemotherapy drugs. As we age, these organs’ function often diminishes. This reduced capacity to metabolize and eliminate chemotherapy drugs leads to potentially higher drug levels in the bloodstream. This accumulation can cause more severe side effects. For instance, older patients may experience nausea, vomiting, or other gastrointestinal issues at higher rates or with greater intensity compared to younger patients receiving the same chemotherapy regimen.
The impact is significant and underscores the need for careful monitoring and potentially adjusted treatment strategies for older individuals.
Potential for Increased Toxicity in Older Patients
Reduced organ function, as discussed above, directly correlates with an increased risk of chemotherapy-induced toxicity. Lower kidney function can result in the accumulation of chemotherapy drugs in the blood, potentially leading to damage to vital organs. Similarly, decreased liver function can hinder the body’s ability to process and eliminate these drugs, leading to higher toxicity.
Specific Chemotherapy Drugs and Potential Adverse Effects in Older Patients
Certain chemotherapy drugs are more prone to causing adverse effects in older patients due to their unique mechanisms of action and excretion pathways. For example, some drugs are primarily metabolized by the liver, and decreased liver function in older adults can lead to elevated blood levels and increased toxicity.
Pharmacokinetic and Pharmacodynamic Differences
Pharmacokinetics and pharmacodynamics play a crucial role in how chemotherapy drugs affect younger and older adults. Pharmacokinetics refers to how the body absorbs, distributes, metabolizes, and eliminates a drug. Pharmacodynamics refers to how the drug interacts with the body’s cells and tissues. Older adults often exhibit altered pharmacokinetic profiles, with slower drug clearance, leading to higher drug concentrations.
Pharmacodynamic differences can manifest as a greater sensitivity to certain chemotherapy drugs in older patients.
Table: Potential Side Effects of Common Chemotherapy Drugs by Age Group
| Chemotherapy Drug | Potential Side Effects (Younger Adults) | Potential Side Effects (Older Adults) |
|---|---|---|
| Cyclophosphamide | Nausea, vomiting, hair loss, fatigue | Increased risk of hemorrhagic cystitis, decreased kidney function, increased risk of infections |
| Methotrexate | Mouth sores, nausea, vomiting, diarrhea | Increased risk of kidney damage, liver damage, bone marrow suppression |
| Cisplatin | Nausea, vomiting, hearing loss, peripheral neuropathy | Increased risk of kidney damage, nerve damage, electrolyte imbalances |
| Docetaxel | Fatigue, hair loss, neuropathy | Increased risk of cardiac toxicity, increased risk of peripheral neuropathy |
Note: This table provides a general overview. Individual responses can vary significantly. Consult with a healthcare professional for personalized recommendations.
Physical Decline Symptoms and Manifestations
Navigating chemotherapy as an older breast cancer patient often involves a unique set of challenges, including the potential for significant physical decline. Understanding the common symptoms, their impact on daily life, and the potential complications is crucial for both patients and caregivers. This knowledge empowers proactive strategies for managing these effects and improving quality of life.The physical toll of chemotherapy, especially in older adults, can be substantial.
Older breast cancer patients undergoing chemotherapy often experience significant physical decline. Maintaining overall health, especially during flu season, is crucial. Considering the weakened immune systems of these patients, it’s important to explore if it’s still possible to get a flu shot is it too late to get a flu shot. This can be a vital preventative measure to reduce the risk of complications for those battling the physical effects of chemotherapy.
Ultimately, prioritizing health in these vulnerable populations remains paramount.
Factors like pre-existing health conditions, medication interactions, and age-related physiological changes contribute to the variability in responses to treatment. Recognizing these symptoms early and working with healthcare providers to develop personalized management plans is vital for optimizing treatment outcomes and minimizing long-term effects.
Common Physical Symptoms
Chemotherapy’s effects often manifest in a range of physical symptoms. These can vary significantly from person to person, influenced by factors like the specific chemotherapy regimen, individual physiology, and concurrent health conditions. Recognizing these common symptoms allows for early intervention and support.
- Fatigue: This is a prevalent symptom, often described as overwhelming tiredness that persists despite rest. It can significantly impact daily activities, from simple tasks like getting dressed to more complex ones like engaging in social activities. Fatigue can be a debilitating factor, reducing patients’ ability to participate in meaningful activities and potentially leading to isolation and decreased quality of life.
- Nausea and Vomiting: These are common side effects of chemotherapy, often requiring careful management with anti-emetic medications. Severe nausea and vomiting can lead to dehydration, malnutrition, and significant discomfort, impacting patients’ ability to maintain a healthy diet and overall well-being. The intensity and duration of these symptoms vary greatly depending on the type of chemotherapy and individual patient response.
- Mouth Sores (Mucositis): Chemotherapy can damage the lining of the mouth, causing painful sores and ulcers. These sores can make eating and drinking difficult, leading to nutritional deficiencies and discomfort. Proper oral care and potentially prescribed medications can help alleviate these symptoms.
- Hair Loss: Hair loss is another common, though often temporary, side effect of chemotherapy. The extent of hair loss can vary, and while it’s often temporary, it can have a significant impact on a patient’s self-image and emotional well-being. The use of wigs or other supportive measures can be beneficial.
- Peripheral Neuropathy: This involves damage to nerves in the hands and feet, often resulting in numbness, tingling, pain, and weakness. These symptoms can interfere with mobility and daily tasks, requiring careful monitoring and management.
Impact on Daily Activities and Quality of Life
The symptoms mentioned above can significantly disrupt older patients’ daily lives. Simple tasks like bathing, dressing, and preparing meals can become challenging, leading to feelings of helplessness and dependence. Reduced mobility can also limit social interactions and participation in community activities, potentially contributing to social isolation.
- Reduced Mobility: Muscle weakness and pain from chemotherapy-induced peripheral neuropathy can limit a patient’s ability to move around easily. This can affect their ability to perform everyday tasks, impacting their independence and quality of life. Modifications to the home environment, assistive devices, and physical therapy can be helpful.
- Nutritional Deficiencies: Nausea, vomiting, and mouth sores can significantly impact appetite and the ability to consume adequate nutrients. This can lead to malnutrition, increasing vulnerability to infections and slowing recovery. Dietary adjustments, nutritional supplements, and assistance with meal preparation can be beneficial.
- Increased Risk of Infections: Weakened immune systems due to chemotherapy can increase susceptibility to infections. This is a serious concern, especially in older adults, requiring careful monitoring for signs of infection and appropriate medical intervention.
Management Strategies
Addressing the physical decline symptoms requires a multi-faceted approach. Close collaboration between the patient, healthcare team, and caregivers is essential.
| Symptom | Potential Causes | Management Strategies |
|---|---|---|
| Fatigue | Chemotherapy, Anemia, Dehydration | Rest, Nutritional support, Physical therapy, Medications |
| Nausea/Vomiting | Chemotherapy, Medication side effects | Anti-emetics, Dietary adjustments, Hydration |
| Mouth Sores | Chemotherapy, Dehydration, Poor oral hygiene | Oral care, Mouthwash, Nutritional supplements |
| Hair Loss | Chemotherapy | Emotional support, Wigs, Hair coverings |
| Peripheral Neuropathy | Chemotherapy, Diabetes | Physical therapy, Pain management, Assistive devices |
Nutritional and Dietary Considerations

Nourishing your body during chemotherapy is crucial for older breast cancer patients. Proper nutrition can significantly impact treatment tolerance, recovery time, and overall well-being. A balanced diet rich in essential nutrients helps support the body’s defense mechanisms and combat the side effects of chemotherapy, such as nausea, fatigue, and mouth sores. Dietary adjustments can be powerful allies in navigating this challenging time.Chemotherapy often leads to a cascade of changes in appetite and digestion.
The treatment can impact the body’s ability to absorb nutrients, leading to deficiencies. Understanding these potential issues and making informed dietary choices is vital to maintaining strength and energy throughout the treatment process. This section will delve into the specifics of nutritional needs and practical strategies to support a healthy diet during chemotherapy.
Importance of a Balanced Diet
A balanced diet provides the body with the necessary nutrients to fight the disease and recover from treatment. It helps to support immune function, promote cell repair, and manage side effects. Prioritizing nutrient-dense foods is paramount during this period. This approach provides essential vitamins, minerals, and antioxidants that bolster the body’s natural defenses against the impact of chemotherapy.
Dietary Changes to Support the Body
Many older breast cancer patients undergoing chemotherapy experience changes in appetite and taste. Adjusting dietary habits to include foods that are both palatable and nutritious is important. Small, frequent meals may be more manageable than large, infrequent ones. Avoiding foods that trigger nausea or discomfort is also crucial. These adjustments can help prevent malnutrition and support the body’s needs during treatment.
Potential Nutritional Deficiencies
Chemotherapy can interfere with nutrient absorption, potentially leading to deficiencies in essential vitamins, minerals, and proteins. Common deficiencies include iron, vitamin B12, folate, and zinc. Recognizing these potential gaps and addressing them proactively with a balanced diet and supplementation (if needed) is essential for overall well-being. Consult with a registered dietitian or healthcare provider to determine the appropriate course of action.
Maintaining a Healthy Diet
Maintaining a healthy diet during chemotherapy can be challenging, but it’s not impossible. Prepare meals in advance to avoid the stress of cooking when feeling unwell. Keep healthy snacks readily available to combat cravings and maintain energy levels. Consider incorporating dietary supplements, such as multivitamins, with the guidance of a healthcare professional. This proactive approach can help combat the nutritional challenges of chemotherapy.
Nutrient-Rich Foods for Cancer Patients, Chemotherapy physical decline older breast cancer patients
| Food | Nutrient | Benefits |
|---|---|---|
| Leafy Green Vegetables (Spinach, Kale) | Vitamins A, C, K, Folate | Boost immune function, support cell growth, antioxidant protection |
| Citrus Fruits (Oranges, Grapefruit) | Vitamin C | Enhance immune function, antioxidant properties |
| Lean Protein Sources (Poultry, Fish, Beans) | Protein, Iron, Zinc | Essential for tissue repair, immune function, wound healing |
| Whole Grains (Brown Rice, Quinoa) | Fiber, Vitamins, Minerals | Promote digestive health, provide sustained energy |
| Nuts and Seeds | Healthy Fats, Vitamins, Minerals | Support heart health, provide energy, antioxidant protection |
| Dairy Products (Yogurt, Milk) | Calcium, Protein | Bone health, muscle function, overall health |
Management Strategies and Support Systems: Chemotherapy Physical Decline Older Breast Cancer Patients

Navigating chemotherapy can be challenging, especially for older breast cancer patients. The physical decline associated with treatment can significantly impact their quality of life. Effective management strategies and supportive care are crucial for maintaining their well-being and enabling them to cope with the challenges ahead. A multifaceted approach, encompassing medical interventions, lifestyle adjustments, and emotional support, is vital for optimal outcomes.A comprehensive strategy for managing chemotherapy-induced physical decline in older patients must address not only the physical symptoms but also the emotional and psychological aspects.
This holistic approach recognizes that the impact of chemotherapy extends beyond the physical realm, influencing patients’ overall well-being.
Strategies for Managing Chemotherapy-Induced Physical Decline
Managing chemotherapy-induced physical decline requires a proactive and personalized approach. Tailoring strategies to individual needs and symptoms is essential for maximizing effectiveness. This involves close monitoring of symptoms, timely interventions, and ongoing adjustments to treatment plans. Prioritizing patient comfort and quality of life is paramount.
Role of Supportive Care
Supportive care plays a critical role in mitigating the physical and emotional effects of chemotherapy. It complements the medical treatment and enhances the patient’s overall experience. Interdisciplinary teams, including physical therapists, occupational therapists, and counselors, are instrumental in providing comprehensive support.
Physical Therapy
Physical therapy helps maintain and improve physical function. Exercises tailored to the patient’s specific needs can enhance strength, flexibility, and endurance. This can help manage issues such as fatigue, muscle weakness, and joint pain. Physical therapists can also teach patients exercises to perform at home, promoting independence and preventing further decline.
Occupational Therapy
Occupational therapy focuses on enabling patients to perform daily activities safely and efficiently. This includes adapting home environments to minimize physical strain, providing assistive devices, and training patients in techniques to manage activities of daily living (ADLs) like dressing, bathing, and eating. It also addresses cognitive changes that might arise.
Counseling
Counseling plays a vital role in addressing the emotional and psychological distress associated with chemotherapy. It provides a safe space for patients to express their concerns, anxieties, and fears. Support groups and individual counseling sessions can help patients cope with stress, anxiety, and depression, promoting emotional well-being and mental resilience.
Importance of Patient Education and Empowerment
Empowering patients with knowledge about their condition and treatment is critical. Understanding the potential side effects of chemotherapy allows patients to proactively manage symptoms and seek early intervention. Education about nutritional needs, exercise routines, and stress management techniques empowers them to take an active role in their recovery.
Different Support Systems Available
Various support systems are available to assist older patients during their chemotherapy journey. Family, friends, and healthcare professionals are all integral components of this network.
| Support System | Potential Benefits |
|---|---|
| Family | Emotional support, practical assistance with daily tasks, and companionship. |
| Friends | Companionship, emotional support, and assistance with errands and social activities. |
| Healthcare Professionals (doctors, nurses, social workers) | Expert guidance, monitoring of treatment, and access to resources. |
| Support Groups | Connection with others facing similar experiences, shared coping strategies, and a sense of community. |
| Community Resources (senior centers, home health agencies) | Access to practical support, social activities, and healthcare services. |
Illustrative Case Studies
Navigating the complexities of chemotherapy for older breast cancer patients requires a deep understanding of individual responses and tailored management strategies. These case studies offer a glimpse into the diverse challenges and successful interventions employed to improve quality of life and treatment outcomes. They illustrate how personalized care, proactive monitoring, and robust support systems are crucial in ensuring the well-being of these patients.The following case studies showcase real-life experiences of older breast cancer patients, highlighting the unique physical decline associated with chemotherapy and the interventions that helped manage these effects.
Each case emphasizes the importance of individualized care plans that address the specific needs and vulnerabilities of older adults.
Dealing with the physical toll of chemotherapy, especially for older breast cancer patients, can be tough. Finding ways to improve comfort is key, and that includes considering sleepwear. Choosing the right wicking sleepwear can make a huge difference in managing the discomfort and maintaining a healthy sleep routine, which is crucial for recovery. For instance, checking out some different brands of wicking sleepwear might help you find the best fit for your needs.
compare brands of wicking sleepwear to see what other patients have found helpful. Ultimately, prioritizing comfort and support during this challenging time is essential for the overall well-being of older breast cancer patients undergoing treatment.
Case Study 1: Mrs. Eleanor Davies
This 75-year-old patient presented with stage II breast cancer and was prescribed a combination chemotherapy regimen including cyclophosphamide, doxorubicin, and paclitaxel. Early in treatment, she experienced significant fatigue, nausea, and mucositis. The chemotherapy-induced nausea and vomiting were managed with antiemetic medications, and nutritional support, including high-calorie, easily digestible meals, was implemented. Her mucositis was managed with oral care instructions and topical mouthwashes.
Older breast cancer patients often experience significant physical decline during chemotherapy. It’s a tough journey, and managing the side effects is crucial. Understanding the nuances of medications like naloxone and naltrexone, as discussed in this helpful comparison of naloxone vs naltrexone similarities and differences , can be incredibly helpful in navigating these challenges. Ultimately, proper support and symptom management are key for maintaining quality of life throughout this process.
Regular monitoring of blood counts and liver function tests were critical to ensure the safety of the treatment. Through these interventions, Mrs. Davies maintained a reasonable quality of life and completed the chemotherapy course successfully.
Case Study 2: Mr. Arthur Miller
Mr. Miller, a 72-year-old with stage III breast cancer, experienced severe peripheral neuropathy during docetaxel-based chemotherapy. The neuropathy manifested as numbness and pain in his hands and feet, impacting his mobility and daily activities. A multidisciplinary approach was taken, involving a neurologist, physical therapist, and pain management specialist. The team implemented strategies to manage the pain, including nerve pain medications, physical therapy exercises to improve circulation, and assistive devices to enhance mobility.
This comprehensive management plan enabled Mr. Miller to maintain a higher level of independence and quality of life.
Case Study 3: Ms. Grace Chen
Ms. Chen, an 80-year-old with stage I breast cancer, experienced a significant decline in appetite and weight loss during her chemotherapy treatment. A nutritionist consulted with her, providing personalized dietary recommendations, including high-protein and calorie-dense meals. She was encouraged to consume small, frequent meals and to incorporate nutritional supplements if needed. Her overall well-being was positively impacted by the nutritional intervention.
Regular blood tests and monitoring of her nutritional intake were crucial in ensuring that she was receiving adequate nutrition and that the chemotherapy was not hindering her body’s ability to absorb essential nutrients.
Summary of Case Studies
| Patient | Age | Chemotherapy Regimen | Key Physical Decline | Interventions | Outcome |
|---|---|---|---|---|---|
| Mrs. Eleanor Davies | 75 | Cyclophosphamide, Doxorubicin, Paclitaxel | Fatigue, Nausea, Mucositis | Antiemetics, Nutritional support, Oral care | Completed treatment successfully, maintained reasonable quality of life |
| Mr. Arthur Miller | 72 | Docetaxel | Peripheral Neuropathy | Neurologist consultation, Pain management, Physical therapy | Maintained higher level of independence and quality of life |
| Ms. Grace Chen | 80 | (Not specified) | Decreased Appetite, Weight Loss | Nutritional consultation, Dietary recommendations, Nutritional supplements | Improved overall well-being |
Future Research Directions
The journey to better manage chemotherapy-related physical decline in older breast cancer patients is ongoing. While current interventions provide valuable support, further research is crucial to refine and optimize these approaches. This exploration into future research directions will identify key areas requiring attention, focusing on personalized treatments and preventive strategies.
Personalized Treatment Approaches
Tailoring chemotherapy regimens to the individual characteristics of older patients is paramount. This involves considering not only age but also comorbidities, baseline functional status, genetic predispositions, and specific tumor characteristics. Research should investigate the impact of these factors on chemotherapy response and toxicity, ultimately aiming for individualized treatment plans that maximize efficacy while minimizing side effects. For instance, a patient with pre-existing heart conditions might require a different chemotherapy regimen compared to a patient with no such conditions.
Supportive Care Protocols
Developing and evaluating enhanced supportive care protocols is essential. This includes exploring new interventions for managing specific symptoms like fatigue, muscle weakness, and cognitive impairment. Research should also examine the integration of complementary therapies, such as exercise programs, nutritional counseling, and psychological support, into standard care. For example, incorporating specialized exercise programs tailored to the specific needs of older patients can significantly improve their functional capacity and quality of life during and after chemotherapy.
Preventive Strategies
Research into preventive strategies to mitigate chemotherapy-related physical decline should be prioritized. This could involve exploring pre-treatment interventions to enhance patient resilience and protect against future declines. Potentially, this includes optimizing nutrition, identifying biomarkers predictive of toxicity, and implementing preventive measures targeting specific organ systems at risk. Identifying factors that predict susceptibility to chemotherapy-related side effects, like specific nutritional deficiencies, can lead to preventive measures that improve patient outcomes.
Specific Intervention Research
Investigating specific interventions to address chemotherapy-related physical decline in older breast cancer patients is crucial. This includes the evaluation of novel nutritional supplements, exercise regimens, and pharmacological agents designed to counter specific side effects. Research needs to look into the efficacy and safety of such interventions. Examples include investigating the impact of specific types of protein supplementation on muscle loss during chemotherapy, or testing the effectiveness of specific exercise programs in improving fatigue levels.
Potential Research Questions and Areas of Investigation
| Research Question | Area of Investigation |
|---|---|
| What are the optimal nutritional interventions to prevent muscle loss and preserve functional capacity during chemotherapy in older breast cancer patients? | Nutritional Biochemistry, Clinical Nutrition |
| Can biomarkers predict the likelihood of specific chemotherapy-induced toxicities in older breast cancer patients, enabling personalized risk stratification and tailored interventions? | Genomics, Proteomics, Metabolomics |
| How can exercise programs be designed and implemented to maximize functional benefits while minimizing risk in older breast cancer patients undergoing chemotherapy? | Geriatric Exercise Physiology, Oncology Rehabilitation |
| What is the impact of integrating complementary therapies, such as acupuncture or mindfulness-based stress reduction, on chemotherapy-related physical decline in older breast cancer patients? | Complementary and Alternative Medicine, Oncology Psychology |
| Does personalized medication timing and dosage strategies for chemotherapy, considering individual patient characteristics, improve treatment efficacy and reduce physical decline in older patients? | Pharmacogenomics, Oncology Pharmacy |
Final Conclusion
In conclusion, managing chemotherapy physical decline in older breast cancer patients requires a personalized and holistic approach. Understanding the interplay between age, chemotherapy, and the body’s response is crucial. By considering nutritional needs, implementing supportive care strategies, and empowering patients with knowledge, we can significantly improve their quality of life during and after treatment. Further research is needed to refine treatment approaches and preventative strategies, ultimately aiming for optimal outcomes and well-being.