Progestin only birth control methods offer a diverse range of options for managing fertility. This guide explores the various types, from pills to injections and implants, examining their mechanisms of action and effectiveness. We’ll also delve into safety profiles, potential side effects, and user experiences to help you understand the nuances of each method.
From understanding the different types of progestin-only birth control methods to exploring their effectiveness and safety, we’ll cover a wide range of essential information. This includes detailed comparisons with other birth control options, considerations for different users, and important medical interactions. We’ll also address factors like cost and accessibility to provide a comprehensive overview.
Overview of Progestin-Only Birth Control Methods
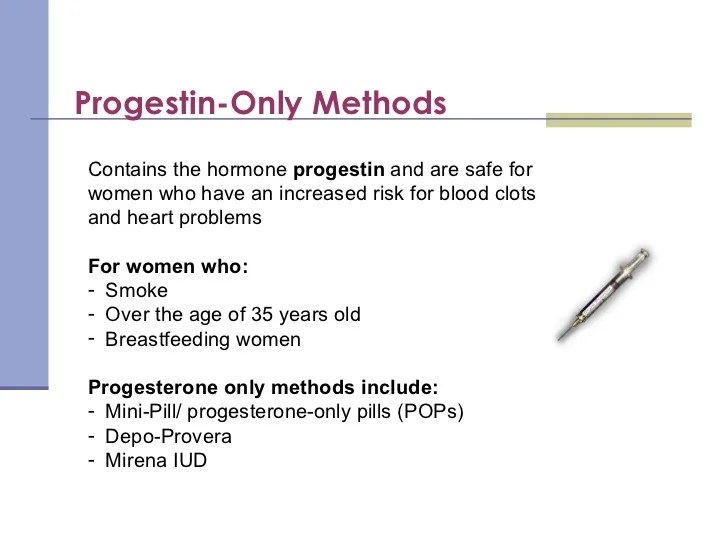
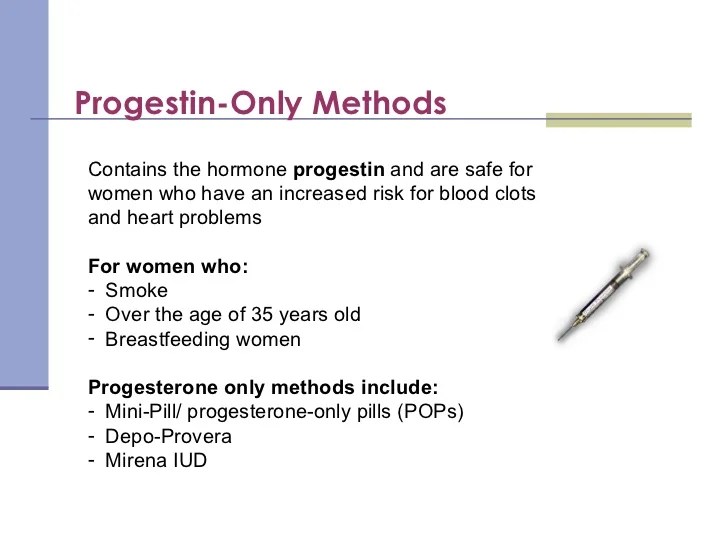
Progestin-only birth control, also known as the mini-pill, is a highly effective method for preventing pregnancy. Unlike combined hormonal contraceptives that contain both estrogen and progestin, these methods rely solely on progestin to prevent ovulation and thicken cervical mucus, making it difficult for sperm to reach the egg. This approach offers a viable alternative for women who can’t or choose not to use estrogen-containing contraceptives.Progestin-only methods come in various forms, each with its own advantages and potential side effects.
Understanding these methods can help individuals make informed decisions about their reproductive health.
Different Types of Progestin-Only Birth Control
These methods utilize different delivery systems to provide consistent progestin levels. Each approach has a unique impact on the body’s hormonal balance and potential side effects.
| Method | Description | Key Benefits |
|---|---|---|
| Progestin-Only Pill (POP) | A daily oral contraceptive containing a small dose of progestin. It’s crucial to take the pill consistently at the same time each day to maintain effectiveness. The pill works by preventing ovulation and thickening cervical mucus. | Convenient, easily accessible, and effective if taken correctly. May be a good option for women who can’t use estrogen-containing contraceptives due to health concerns. |
| Injectable Progestin | A long-acting progestin injection administered every 3 months. This injection works by suppressing ovulation and altering the cervical mucus to make it difficult for sperm to reach the egg. | Offers extended protection from pregnancy, requiring less frequent attention than daily pills. Potentially good for those who struggle with remembering daily medication. |
| Progestin-Only Implant | A small, flexible rod implanted under the skin of the upper arm. It releases a steady stream of progestin into the body, preventing pregnancy for up to 3 years. This method is designed for long-term, consistent protection against pregnancy. | Provides long-term contraception without the need for daily reminders. Suitable for women seeking a highly effective and convenient long-term birth control solution. |
| Progestin-Releasing Intrauterine Device (IUD) | A small, T-shaped device inserted into the uterus. It releases progestin to prevent pregnancy. The IUD creates a hostile environment for sperm, inhibiting fertilization. | Highly effective method of contraception, providing long-term protection. May be a good option for women who want a non-oral contraceptive. |
Mechanism of Action
The primary mechanism of action for all progestin-only methods is to prevent ovulation and make the cervical mucus hostile to sperm. This combined effect reduces the likelihood of fertilization. Different delivery systems achieve this through various hormonal profiles.
Progestin-only methods work primarily by suppressing ovulation, altering cervical mucus, and potentially changing the lining of the uterus to make it less receptive to a fertilized egg.
Progestin-only birth control methods are a popular choice for many women, offering a reliable way to prevent pregnancy. However, understanding the potential long-term health implications is crucial. Factors like the potential impact on life expectancy in conditions like Alzheimer’s disease and dementia are an important consideration when making choices about birth control methods. Life expectancy in Alzheimer’s disease and dementia can vary greatly, depending on factors like the individual’s overall health and the progression of the disease.
Ultimately, women should discuss their options with their healthcare providers to make the best decisions about their reproductive health.
For example, the progestin-only pill prevents ovulation in the majority of cycles, while the implant provides a sustained release of progestin to maintain consistent suppression. Injectable progestin works by delivering a concentrated dose of progestin every three months, maintaining a constant hormonal level. The IUD acts by continuously releasing progestin into the uterus, creating a hostile environment for sperm and preventing implantation.
Effectiveness and Safety
Progestin-only birth control methods, while effective, come with a range of potential side effects. Understanding the nuances of each method, its effectiveness, and the possible trade-offs between effectiveness and safety is crucial for informed decision-making. This section delves into the effectiveness of these methods, details potential side effects, and compares various options to help you navigate the choices available.These methods, often a great alternative to combined hormonal contraceptives, rely on progestin to prevent pregnancy.
The varying formulations and dosages of progestin influence both the effectiveness and potential side effects.
Effectiveness in Preventing Pregnancy
Progestin-only methods, when used correctly, demonstrate high effectiveness in preventing pregnancy. Their efficacy is comparable to combined hormonal contraceptives, although user adherence is a significant factor. Consistent use, as per the prescribed regimen, is paramount to achieving the intended contraceptive effect. Failure rates are typically lower for those who strictly adhere to the recommended usage instructions.
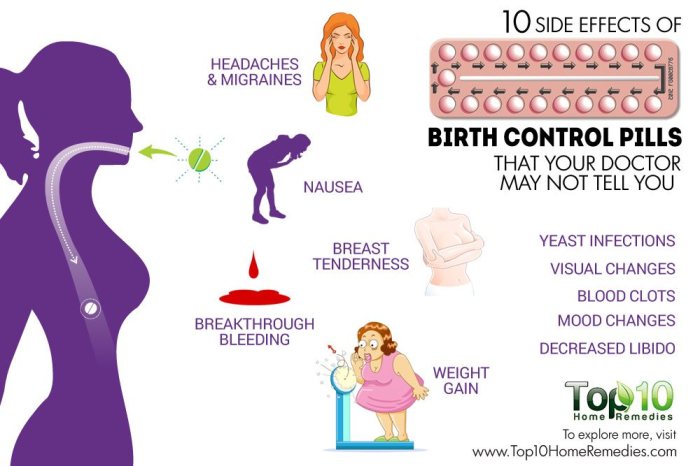
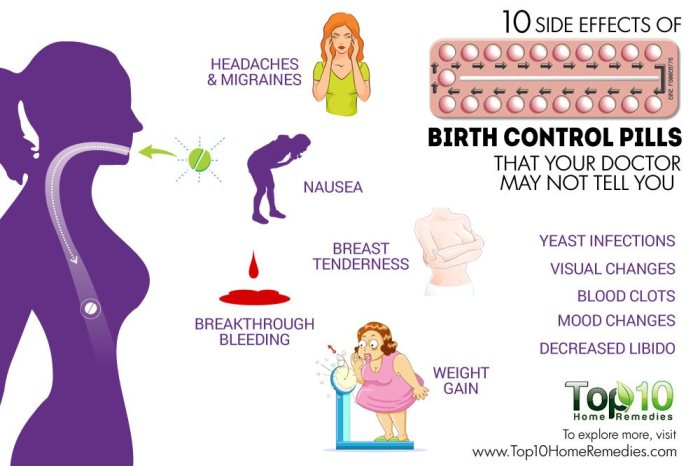
Potential Side Effects of Different Methods
Different progestin-only methods may have varying side effect profiles. The specific progestin used, the dosage, and the route of administration can all contribute to the experience. Some common side effects include irregular bleeding, mood changes, weight fluctuations, and breast tenderness. The severity and duration of these side effects can differ significantly between individuals. Importantly, it’s crucial to remember that not everyone experiences these side effects, and some may experience them to a lesser degree.
Comparison of Progestin-Only Methods
The following table provides a comparison of various progestin-only methods based on effectiveness, potential side effects, and user experience. This table is not exhaustive, and individual experiences may vary.
| Method | Effectiveness (typical failure rate per year) | Potential Side Effects | User Experience (general feedback) |
|---|---|---|---|
| Progestin-only pills (POPs) | 3-8% | Irregular bleeding, headaches, breast tenderness, mood changes | Generally well-tolerated; often cited as easier to manage than combined pills |
| Progestin-releasing IUD (e.g., Mirena) | 0.1-0.5% | Irregular spotting or bleeding, cramping, expulsion risk | Generally highly effective and long-lasting; some users report heavier bleeding initially |
| Progestin implant (e.g., Nexplanon) | 0.05% | Irregular bleeding, acne, mood changes, headaches | Very effective and long-lasting; requires a minor surgical procedure for insertion and removal |
| Progestin injection (e.g., Depo-Provera) | 0.3-6% | Weight gain, irregular bleeding, bone density concerns (long-term use) | Long-acting method; users may experience more pronounced hormonal changes |
Factors Influencing User Experience
Individual factors can influence how a progestin-only method affects a user. Age, pre-existing medical conditions, and lifestyle choices can all play a role in the experience. For example, women with a history of migraines may experience increased frequency or intensity of migraines with some progestin-only methods. It’s essential to discuss any concerns with a healthcare provider before making a decision.
Benefits and Considerations
Progestin-only birth control methods offer a viable alternative to other contraceptive options, but careful consideration of their advantages and disadvantages is crucial for informed decision-making. Understanding the nuances of these methods, including their suitability for various age groups and health conditions, is essential for selecting the most appropriate approach for individual needs. This section delves into the specifics, exploring potential benefits and drawbacks, and outlining suitable user groups.Choosing a birth control method is a personal decision.
While progestin-only methods have their advantages, it’s important to weigh them against potential drawbacks. Individual factors like age, medical history, and lifestyle preferences all play a role in determining the optimal choice.
Advantages of Progestin-Only Methods, Progestin only birth control methods
Progestin-only methods, often preferred for their potential benefits, present certain advantages over other options. These methods can be a good choice for individuals who experience side effects with combined hormonal contraceptives or those who wish to avoid estrogen. They are generally well-tolerated and may be more suitable for breastfeeding mothers, given their minimal impact on milk production.
Potential Drawbacks and Considerations
While progestin-only methods have positive attributes, potential drawbacks need careful consideration. Irregular bleeding patterns, including spotting or breakthrough bleeding, can occur. The risk of unintended pregnancy, while lower than with no contraception, is not zero. This necessitates a commitment to consistent use for maximum effectiveness.
Suitability for Different Age Groups and Health Conditions
The appropriateness of progestin-only methods depends on individual circumstances. For instance, adolescents may experience fluctuating hormone levels, which might influence how their bodies respond to these methods. Women with certain medical conditions, such as a history of blood clots, should consult their healthcare providers before choosing this type of birth control. For women in specific age groups or with particular health concerns, progestin-only methods might be more suitable than other options.
Comparison of Progestin-Only Methods
| Method | Potential Benefits | Potential Drawbacks | Suitable Users |
|---|---|---|---|
| Depot Medroxyprogesterone Acetate (DMPA) | High effectiveness, relatively convenient (injection every 3 months), may improve acne in some users. | Irregular bleeding, potential weight gain, and bone mineral density changes. | Individuals who prefer infrequent dosing and prioritize high effectiveness. Should be considered carefully for those concerned about bone health. |
| Progestin-only pills (POPs) | Minimal impact on milk production (useful for breastfeeding mothers), generally well-tolerated by many. | Requires strict adherence to dosing schedule, potential for irregular bleeding. | Breastfeeding mothers, women with a history of estrogen-related issues, or those seeking a method with lower systemic estrogen exposure. |
| Progesterone Implant | High effectiveness, long-lasting (3 years), consistent hormone release. | Irregular bleeding, potential for pain during insertion, and difficulty with removal. | Individuals seeking a highly effective and long-term method, who are comfortable with an infrequent procedure. |
Medical Considerations and Interactions
Progestin-only birth control methods, while generally safe, may not be suitable for everyone. Understanding potential medical conditions that might interact with these methods is crucial for making informed decisions. Furthermore, knowing how other medications and supplements might affect their effectiveness is vital for optimizing their use. This section details these interactions, emphasizing the importance of consulting a healthcare provider before starting or continuing these methods.Certain medical conditions can influence the suitability of progestin-only birth control.
A thorough medical history is essential to assess potential risks and benefits.
Potential Medical Conditions
Several medical conditions can affect the efficacy or safety of progestin-only birth control. Conditions like liver disease, undiagnosed vaginal bleeding, or a history of blood clots can impact the method’s suitability. Thorough medical evaluation is paramount to ensure the method is appropriate for an individual’s health status.
Medication and Supplement Interactions
Many medications and supplements can interact with progestin-only birth control, potentially affecting its effectiveness. For instance, certain antibiotics or anticonvulsants might reduce the effectiveness of the birth control. Similarly, some herbal supplements can also interfere with the method’s efficacy. It’s important to disclose all medications and supplements to your healthcare provider to avoid any potential interactions.
Potential Interactions Table
| Medication/Supplement | Potential Interaction | Impact on Birth Control |
|---|---|---|
| Antibiotics (e.g., rifampin, rifabutin) | Increased metabolism of progestin | Reduced effectiveness of birth control; increased risk of pregnancy |
| Anticonvulsants (e.g., phenytoin, carbamazepine) | Increased metabolism of progestin | Reduced effectiveness of birth control; increased risk of pregnancy |
| St. John’s Wort | Increased metabolism of progestin | Reduced effectiveness of birth control; increased risk of pregnancy |
| Certain Herbal Supplements (e.g., some that contain St. John’s Wort) | Increased metabolism of progestin | Reduced effectiveness of birth control; increased risk of pregnancy |
| Some HIV medications | Increased metabolism of progestin | Reduced effectiveness of birth control; increased risk of pregnancy |
Importance of Professional Consultation
It’s crucial to discuss any existing medical conditions, including those not directly related to the reproductive system, with a healthcare professional before starting or continuing progestin-only birth control. Furthermore, a complete list of all medications, including over-the-counter drugs and supplements, must be provided. This comprehensive approach ensures the best possible outcomes, minimizing potential risks and maximizing the effectiveness of the method.
Your healthcare provider can assess your individual needs and determine the most suitable birth control option. They can also guide you on managing potential interactions between medications and the birth control method.
Progestin-only birth control methods are a great option for some women, offering a simple way to prevent pregnancy. However, understanding potential side effects is key. Sometimes, similar hormonal imbalances can arise that might be comparable to the differences between medications like Desoxyn and Adderall, impacting different aspects of the body. For a deeper dive into how these medications compare, check out this helpful resource on desoxyn vs adderall how do they differ.
Ultimately, the best birth control method depends on individual needs and health considerations.
User Experiences and Reviews
Progestin-only birth control methods offer a viable option for many women, but understanding the diverse user experiences is crucial for informed decision-making. Personal accounts and feedback provide valuable insights into the effectiveness, side effects, and overall satisfaction with these methods. This section delves into common user experiences, concerns, and potential long-term effects.Many women find progestin-only pills, injections, implants, or IUDs to be a convenient and effective way to manage their reproductive health.
However, individual experiences can vary significantly, influenced by factors like dosage, method type, and personal physiology. It’s important to approach this information with a balanced perspective, acknowledging that personal experiences are subjective and may not represent the norm for every user.
Typical User Experiences
User experiences with progestin-only birth control methods encompass a wide spectrum of positive and negative feedback. Positive experiences often highlight the convenience and effectiveness of the chosen method, particularly in cases where it aligns well with lifestyle and health needs. Women appreciate the reduced risk of some side effects associated with combined hormonal contraceptives.Conversely, some users report side effects such as irregular bleeding, mood changes, or weight fluctuations.
These experiences can range from mild to significant, affecting the overall user experience. Understanding these potential side effects is crucial for informed decision-making.
Common Questions and Concerns
Common questions and concerns frequently raised by users of progestin-only birth control methods often revolve around the potential for irregular bleeding patterns, mood changes, or changes in menstrual cycles. Users may also question the long-term implications of hormonal exposure, seeking reassurance about the safety of these methods. Furthermore, the potential for decreased effectiveness if the medication is not taken as prescribed is also a significant concern.
Progestin-only birth control methods are a popular choice for many women, offering a convenient way to prevent pregnancy. However, it’s important to be aware of potential health considerations, including potential heart health risks. For a deeper understanding of heart disease risk factors, check out our expert’s insights at ask the expert heart disease risk factors. Ultimately, open communication with your doctor about any concerns surrounding progestin-only birth control is crucial for informed decision-making.
Summary of User Experiences by Method
| Method | Positive Experiences | Negative Experiences | Common Concerns |
|---|---|---|---|
| Progestin-only pills | Convenience, potential for reduced side effects compared to combined pills, relatively affordable. | Irregular bleeding, spotting, headaches, breast tenderness, mood changes. | Consistency of pill-taking, potential for missed pills affecting effectiveness. |
| Progestin-only injection | Long-lasting protection, convenient administration schedule. | Irregular bleeding, weight gain, bone density changes (in some cases). | Potential for irregular periods, limited reversibility. |
| Progestin-only implant | Extended protection, minimal daily management. | Irregular bleeding, mood changes, headaches, breast tenderness. | Potential for irregular periods, cost. |
| Progestin-only IUD | Long-term protection, minimal daily management, reduced risk of side effects associated with other methods. | Irregular bleeding, spotting, cramping, pelvic pain. | Potential for expulsion, cost. |
Potential Long-Term Effects
While progestin-only methods are generally considered safe, potential long-term effects, though rare, exist. For instance, some studies suggest a possible association between prolonged use and bone density changes. However, the overall risk-benefit profile of these methods remains favorable for many women. Individual experiences may vary, and it is essential to discuss any concerns with a healthcare provider.
Furthermore, the long-term impact of hormonal exposure needs to be viewed in the context of other factors such as lifestyle and family history. For example, a woman with a family history of osteoporosis might need to discuss the potential impact of long-term progestin use with her physician.
Contraindications and Precautions
Progestin-only birth control methods offer a viable option for many women, but understanding potential contraindications and precautions is crucial for informed decision-making. These methods, while generally safe, may not be suitable for everyone. Careful consideration of individual health history and circumstances is essential to ensure optimal safety and effectiveness.Knowing when a progestin-only method might not be the best choice, or when extra care is needed, empowers you to have a productive conversation with your healthcare provider.
This allows for personalized guidance and the selection of the most appropriate birth control option.
Specific Contraindications
Certain medical conditions can make progestin-only methods unsuitable. These include, but are not limited to, undiagnosed vaginal bleeding, known or suspected pregnancy, a history of blood clots, liver disease, or breast cancer. It’s vital to disclose all relevant medical history to your healthcare provider to determine if these methods are appropriate for your individual circumstances. This proactive approach ensures your safety and well-being.
Important Precautions
Beyond contraindications, certain precautions are essential when using progestin-only methods. Regular check-ups with your healthcare provider are critical for monitoring your health and ensuring the method’s effectiveness and safety. Prompt reporting of any unusual symptoms, such as persistent headaches, severe abdominal pain, or vision changes, is also important. This proactive approach helps ensure early detection and management of any potential issues.
Table of Contraindications and Precautions by Method
| Method | Contraindications | Precautions |
|---|---|---|
| Depot Medroxyprogesterone Acetate (DMPA) | History of blood clots, liver disease, undiagnosed vaginal bleeding, pregnancy, or breast cancer. | Regular check-ups, prompt reporting of unusual symptoms, and awareness of potential side effects like irregular bleeding or weight changes. |
| Progestin-only pills (POPs) | History of blood clots, liver disease, undiagnosed vaginal bleeding, pregnancy, or breast cancer. Certain medications may interact with POPs. | Consistent pill-taking is critical for effectiveness. Reporting any unusual side effects like depression or mood swings is crucial. |
| Progesterone-releasing IUDs | History of pelvic inflammatory disease, abnormal uterine bleeding, pregnancy, or undiagnosed pelvic pain. | Regular check-ups, prompt reporting of any signs of infection or discomfort, and awareness of potential side effects like spotting or cramping. |
Importance of Open Communication with Healthcare Provider
Honest and open communication with your healthcare provider is essential. This includes discussing your complete medical history, any current medications you are taking, and any concerns or questions you may have. This dialogue empowers you to make informed decisions about your health and well-being. Your provider can offer tailored advice and support based on your unique situation.
Comparison with Other Birth Control Options
Choosing the right birth control method is a personal decision, and understanding the various options available is key. Progestin-only methods offer a unique set of advantages and disadvantages compared to other approaches. This comparison will help you weigh the pros and cons of each method to find the best fit for your individual needs and lifestyle.
Comparison Table
A table summarizing the key differences between progestin-only methods, combined hormonal methods, barrier methods, and IUDs can provide a clear overview:
| Method | Mechanism | Effectiveness | Side Effects | Advantages | Disadvantages |
|---|---|---|---|---|---|
| Progestin-only pills (POPs) | Thicken cervical mucus, thin uterine lining, and inhibit ovulation. | 91-99% effective with perfect use, 88-94% effective with typical use. | Spotting, breast tenderness, headaches, mood changes. | Lower risk of some side effects compared to combined hormonal methods, available in various forms. | Requires strict adherence to the schedule, can cause irregular bleeding. |
| Combined Hormonal Methods (e.g., birth control pills) | Prevent ovulation and thicken cervical mucus. | 91-99% effective with perfect use, 91-95% effective with typical use. | Nausea, headaches, breast tenderness, mood changes, blood clots. | Highly effective, regulate menstrual cycles. | Potential for more significant side effects than progestin-only methods, potential interactions with other medications. |
| Barrier Methods (e.g., condoms, diaphragms) | Physically block sperm from reaching the egg. | 78-88% effective with typical use. | Allergic reactions, discomfort, potential for breakage or slippage. | No hormonal side effects, readily available. | Requires consistent use, may not be as effective as hormonal methods. |
| Intrauterine Devices (IUDs) | Prevent implantation of a fertilized egg, thicken cervical mucus, or release hormones. | 99% effective with consistent use. | Spotting, cramping, heavier periods, expulsion risk. | Long-lasting, highly effective, can be reversible. | Insertion can be uncomfortable, potential for infection. |
Strengths and Weaknesses of Progestin-Only Methods
Progestin-only methods, such as the mini-pill, offer advantages over combined hormonal methods for some individuals. A key strength is the reduced risk of some side effects associated with estrogen. However, consistent daily use is crucial for optimal effectiveness.
Comparison with Other Methods
Progestin-only pills often demonstrate a lower risk of side effects, such as blood clots, compared to combined hormonal methods. However, they may lead to irregular bleeding or spotting, which can be a drawback for some women. Barrier methods, like condoms, offer a non-hormonal alternative but are less effective in preventing pregnancy than hormonal methods. IUDs provide long-lasting, highly effective contraception, but insertion can be uncomfortable for some.
The best choice depends on individual circumstances, health history, and preferences. Consider discussing these options with your healthcare provider to determine the most suitable method for you.
Access and Affordability
Progestin-only birth control methods offer a viable option for many individuals, but their accessibility and cost can vary significantly across different regions and socioeconomic groups. Understanding these factors is crucial for informed decision-making. Factors such as insurance coverage, local regulations, and individual financial situations can all play a role in determining the practicality of these methods.The availability of progestin-only birth control methods varies greatly depending on the location.
Access in some regions might be more readily available through healthcare providers and pharmacies, while other areas may face challenges in terms of provider availability or affordability. This variation impacts the ease with which individuals can obtain these methods.
Accessibility Across Regions
Progestin-only birth control methods are generally available globally, but their accessibility varies significantly. Factors like healthcare infrastructure, cultural norms, and government policies influence access. In developed nations, access tends to be more straightforward through various healthcare channels, including clinics, family planning centers, and pharmacies. Conversely, in developing countries, access might be limited due to factors like a lack of comprehensive healthcare systems, financial constraints, or social stigmas.
Even within developed nations, rural areas or underserved communities may face challenges in obtaining these methods.
Cost Factors and Insurance Coverage
The cost of progestin-only birth control methods can vary based on several factors, including the specific method, the provider, and insurance coverage. Some methods, like the Depo-Provera injection, may involve a single high cost, while others, like the mini-pill, require ongoing monthly expenses. Out-of-pocket costs can vary significantly based on individual insurance plans, and those without insurance or with limited coverage might face higher costs.
It is crucial to understand the specific cost structure of each method before making a decision.
Summary Table of Cost and Availability
| Method | Typical Cost (per month/dose)
|
Availability (general estimate) | Comments |
|---|---|---|---|
| Mini-pill | $15-$50 per month | Widely available in most regions | Requires daily intake, potential side effects like spotting |
| Progestin-only injection (Depo-Provera) | $300-$600 per injection | Widely available in most regions | Given every 3 months, may have higher cost compared to other options |
| Progestin-releasing IUD (Mirena, Kyleena) | $500-$1000 (initial cost for insertion) | Widely available in most regions | Long-term, high efficacy method |
| Progestin implant | $400-$800 (initial cost for insertion) | Widely available in most regions | Long-term, highly effective method |
Note: Prices are estimates and may vary based on location, provider, and insurance coverage. It is crucial to check with local providers for current pricing.
Choosing the Right Method
Finding the perfect progestin-only birth control method is a deeply personal journey. It involves careful consideration of your individual needs, lifestyle, and health history. The right choice depends on factors ranging from your overall health to your comfort level with different administration methods. This section will guide you through the key considerations for selecting the most suitable progestin-only method for your unique circumstances.Choosing the right progestin-only birth control method is a significant decision.
It’s essential to approach this choice with a thorough understanding of the various options and their potential effects on your body and life. Open communication with your healthcare provider is crucial for navigating the process effectively.
Factors to Consider
Understanding your priorities and preferences is paramount when selecting a progestin-only method. Consider factors like how often you take medication, how well you manage a schedule, your comfort level with various administration methods, and any potential side effects. Your healthcare provider can provide personalized advice based on your unique situation.
Importance of Open Communication
Open and honest communication with your healthcare provider is absolutely vital. They can assess your medical history, discuss potential side effects, and help you determine which method aligns best with your health goals. This collaborative approach empowers you to make informed decisions. Don’t hesitate to ask questions; your provider is there to support you.
Method-Specific Considerations
The following table highlights key factors to consider for each progestin-only birth control method. Remember, this is not an exhaustive list, and your healthcare provider will offer more personalized advice.
| Method | Administration | Potential Benefits | Potential Side Effects | Suitability for Specific Needs |
|---|---|---|---|---|
| Injectable (e.g., Depo-Provera) | Injection every 3 months | High efficacy, convenient due to infrequent dosing | Weight gain, irregular bleeding, bone density concerns | Suitable for individuals who prefer infrequent dosing and have reliable access to healthcare for injections. |
| Implantable (e.g., Nexplanon) | Implant placed under the skin | High efficacy, long-lasting protection (up to 3 years) | Irregular bleeding, acne, mood changes | Suitable for individuals who desire long-term, highly effective birth control and have no concerns about potential side effects. |
| Oral (e.g., Microgynon) | Daily pill | Easy to use, potential benefits for menstrual regulation | Potential for nausea, headaches, breast tenderness | Suitable for individuals who prefer a daily pill and are comfortable managing a daily schedule. |
| Progestin-only patch (e.g., Evra) | Weekly patch application | High efficacy, potential benefits for menstrual regulation | Skin irritation, potential for side effects similar to pills | Suitable for individuals who prefer a weekly application and have no skin sensitivity concerns. |
Pregnancy and Lactation Considerations: Progestin Only Birth Control Methods
Progestin-only birth control methods offer a viable option for many women, but their use during pregnancy or while breastfeeding requires careful consideration. Understanding the potential implications and consulting with a healthcare provider is crucial for making informed decisions.Using progestin-only methods during pregnancy is not recommended. These methods are designed to prevent pregnancy, and their use during pregnancy poses potential risks to the developing fetus.
It’s important to discontinue the method immediately and explore alternative family planning options if pregnancy is confirmed.
Using Progestin-Only Methods During Breastfeeding
Progestin-only birth control methods can generally be used while breastfeeding, although individual factors need careful consideration. The hormones in these methods may have minimal impact on milk production, making them a suitable option for some women.
Considerations for Breastfeeding Mothers
Several factors influence the suitability of progestin-only methods for breastfeeding mothers. These include the specific type of progestin used, the duration of breastfeeding, and the mother’s overall health.
- Impact on Milk Production: Most progestin-only methods have a minimal effect on milk production. However, some women may experience minor changes in breast milk volume or consistency. The impact varies depending on the specific progestin used. For example, some formulations may have a slightly stronger effect on milk production than others.
- Timing of Initiation: The timing of starting the method after childbirth is important. Consult with a healthcare provider to determine the appropriate timeframe for initiating use, considering individual circumstances and potential effects on milk production.
- Type of Progestin: The type of progestin in the chosen method plays a significant role. Some progestins are more likely to affect milk production than others. A healthcare provider can provide information specific to the chosen method.
- Individual Health Conditions: Pre-existing health conditions or other medications a mother is taking can influence the suitability of a progestin-only method. The healthcare provider can assess potential interactions and provide personalized recommendations.
Importance of Consulting with a Healthcare Provider
It is essential to discuss all options and potential risks with a healthcare provider before initiating or continuing any progestin-only method during pregnancy or while breastfeeding. A healthcare provider can assess individual circumstances and provide personalized recommendations based on the mother’s specific needs and medical history.
A comprehensive consultation is crucial to ensure the chosen method is safe and effective while minimizing any potential impact on breastfeeding.
This consultation includes a review of medical history, current medications, and any potential interactions with the progestin-only method. A provider can also provide guidance on the potential risks and benefits based on individual circumstances, as well as answer any questions or concerns.
Ultimate Conclusion
In conclusion, progestin-only birth control methods offer a variety of choices for managing fertility. This comprehensive guide has highlighted the different types, effectiveness, safety profiles, user experiences, and medical considerations associated with each. Remember that consulting a healthcare professional is crucial for personalized advice and to determine the most suitable method for your individual needs and circumstances. By weighing the benefits and drawbacks, and considering factors like potential side effects and cost, you can make an informed decision that aligns with your overall well-being.