The benefits of lactase supplements are significant for those dealing with lactose intolerance. Lactase supplements work by aiding the body’s digestion of lactose, the sugar found in dairy products. This allows individuals to consume dairy without experiencing the common digestive discomfort often associated with lactose intolerance. From immediate relief to expanded dietary choices, understanding the different forms, benefits, and potential considerations is key to making informed decisions.
This guide will delve into the science, forms, benefits, and important considerations surrounding lactase supplements.
This article explores the various ways lactase supplements can improve digestion and enhance dietary flexibility. We’ll discuss how these supplements work, compare different forms, and analyze the potential side effects to help you make the best choices for your needs. We’ll also look at the research behind their effectiveness and how to integrate them into a healthy lifestyle.
Introduction to Lactase Supplements

Lactase supplements are enzymes that help individuals with lactose intolerance digest milk sugar (lactose). They work by breaking down lactose into simpler sugars, glucose, and galactose, which are more easily absorbed by the body. This process alleviates the digestive distress often associated with lactose intolerance, such as bloating, gas, and diarrhea.The science behind lactose intolerance stems from a deficiency or absence of the lactase enzyme in the small intestine.
Normally, lactase breaks down lactose into its component sugars. When lactase is insufficient, lactose remains undigested, ferments in the gut, and produces the uncomfortable symptoms mentioned above. Lactase supplements provide the missing enzyme, allowing lactose digestion to occur without the associated discomfort.
Lactase supplements can be a real lifesaver for those struggling with lactose intolerance. They help break down lactose, making dairy products easier to digest. However, while these supplements offer relief, it’s important to remember that many challenges still exist for the deaf community, like ensuring equal access to healthcare and communication. Understanding these hurdles is crucial for creating a more inclusive society, which is equally as important as the digestive benefits of lactase supplements.
This is why I’ve linked to a blog post discussing those challenges for further reading, what challenges still exist for the deaf community , and hopefully it’ll help people think more deeply about the importance of inclusivity for all. Fortunately, lactase supplements can bring relief to those who struggle with lactose, making it easier to enjoy dairy products.
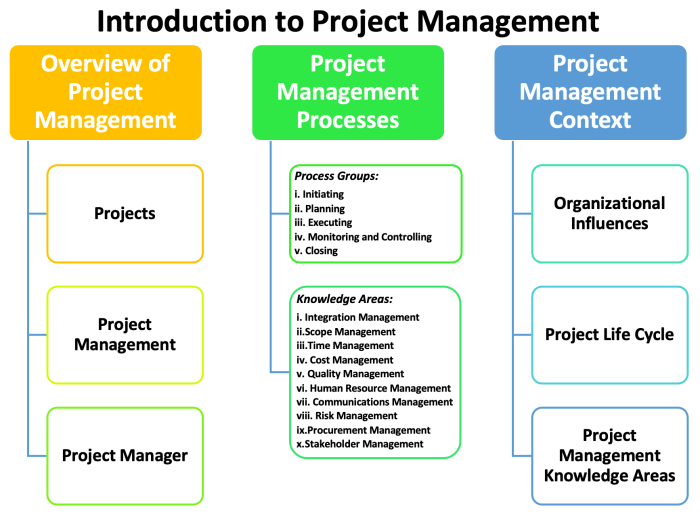
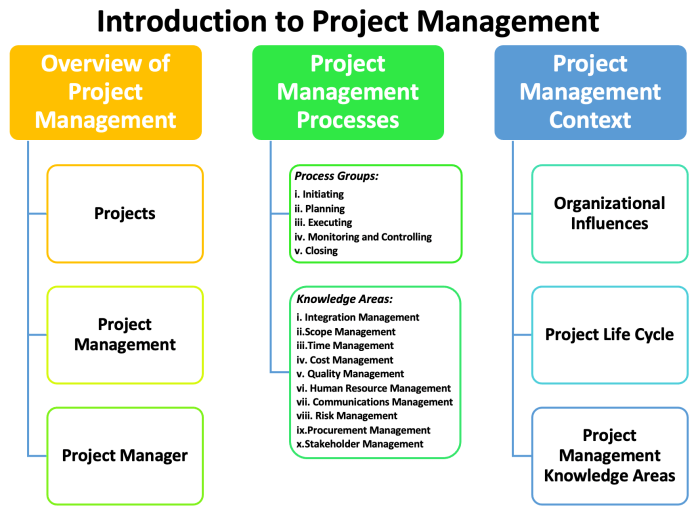
Forms of Lactase Supplements
Lactase supplements come in various forms, each with its own advantages and disadvantages. Understanding these differences can help individuals choose the best option for their needs.
Comparison of Lactase Supplement Forms
| Form | Pros | Cons |
|---|---|---|
| Tablets | Convenient to take, often available in various dosages, relatively affordable. | May not be as effective as other forms for some individuals, can have a slightly bitter taste for some. |
| Drops | Can be easily measured, potentially higher bioavailability compared to tablets in some cases, and can be added directly to food or beverages. | May require precise measurement, and potential for leakage or spills, and some individuals might find the taste unpleasant. |
| Capsules | Similar to tablets in terms of convenience, but often have a more palatable form for those who find tablets less desirable. | Can be less effective compared to drops, potentially less affordable than drops in some cases. |
| Chewable Tablets | Easier to take than regular tablets, particularly for those who have difficulty swallowing. | Can be less potent than other forms and may not be available in as wide a range of dosages as other forms. |
Factors to Consider When Choosing a Lactase Supplement
Several factors can influence the selection of a lactase supplement. Individual needs and preferences, the severity of lactose intolerance, and the cost are crucial considerations. Consult with a healthcare professional or a registered dietitian for personalized advice on choosing the right supplement and dosage.
Benefits for Digestive Health
Lactase supplements offer significant relief for individuals experiencing digestive discomfort associated with lactose intolerance. These supplements work by directly addressing the root cause of the problem, improving digestion and significantly enhancing overall well-being. Understanding how these supplements function and how they interact with other dietary choices is key to maximizing their benefits.Lactase supplements work by providing the enzyme lactase, which is essential for breaking down lactose, a sugar found in dairy products.
When lactase is present in adequate amounts, the body can efficiently digest lactose, preventing the fermentation process that leads to uncomfortable symptoms. This efficient breakdown translates into improved digestive health and a more comfortable experience for those with lactose intolerance.
Immediate Relief from Digestive Discomfort
Lactase supplements can provide almost immediate relief from the uncomfortable symptoms associated with lactose ingestion. By rapidly breaking down lactose, the digestive system can process dairy products without the buildup of undigested lactose, reducing the chances of gas, bloating, and diarrhea. This rapid relief allows individuals to enjoy dairy-containing foods without the usual digestive distress.
Preventing or Reducing Symptoms
Lactase supplements can significantly prevent or reduce the severity of common symptoms like bloating, gas, and diarrhea, frequently experienced by those with lactose intolerance. By breaking down lactose more efficiently, the digestive system is less likely to ferment the undigested lactose, reducing the production of gas and other uncomfortable symptoms. This allows for a more comfortable and enjoyable dietary experience.
Supporting Overall Digestive Health
By promoting efficient lactose digestion, lactase supplements support overall digestive health. A healthy digestive system is essential for nutrient absorption and overall well-being. Efficient lactose digestion ensures that the body absorbs the necessary nutrients from dairy products without the discomfort and inefficiencies caused by lactose intolerance. This can have a positive impact on various bodily functions.
Effectiveness Compared to Other Digestive Aids
While other digestive aids might address specific digestive issues, lactase supplements target the specific problem of lactose intolerance by providing the necessary enzyme. Their effectiveness is typically higher when compared to other digestive aids in addressing the uncomfortable symptoms of lactose intolerance. The direct action on lactose digestion often yields quicker and more noticeable results than other approaches.
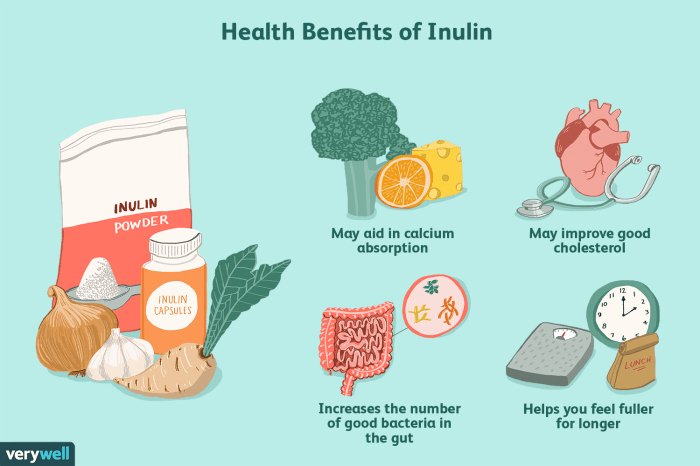
Dietary Changes for Enhanced Digestion
Combining lactase supplements with certain dietary changes can further enhance digestive health. For instance, consuming smaller portions of dairy products more frequently throughout the day can help manage lactose digestion more effectively. Reducing the overall intake of dairy products, or strategically choosing low-lactose options, can also be beneficial. Furthermore, incorporating foods high in probiotics and fiber into the diet can promote a healthy gut microbiome, supporting overall digestive health and potentially reducing the severity of lactose intolerance symptoms.
Benefits for Dietary Flexibility
Lactase supplements offer a significant advantage for individuals with lactose intolerance, enabling them to enjoy a wider variety of foods and maintain a balanced diet. By breaking down lactose, these supplements unlock the nutritional value of dairy products, promoting a healthier and more diverse culinary experience. This is crucial for overall well-being as a varied diet supports optimal health.Expanding dietary options is a key benefit for those with lactose intolerance.
Lactase supplements work by providing the necessary enzyme to digest lactose, the sugar found in dairy products. This allows individuals to consume dairy without experiencing the unpleasant digestive symptoms often associated with lactose intolerance, such as bloating, gas, and diarrhea.
Expanded Dietary Choices
Lactase supplements dramatically broaden the range of dairy-based foods accessible to individuals with lactose intolerance. They effectively remove the barrier of digestive distress, making dairy products more palatable and nutritious. This opens doors to a wider array of culinary possibilities, enriching dietary choices.
Enjoying Dairy Products
Dairy products are an excellent source of essential nutrients like calcium, protein, and vitamin D. These nutrients are vital for maintaining strong bones, supporting muscle function, and bolstering overall health. Lactase supplements empower individuals with lactose intolerance to incorporate dairy into their diet without suffering negative reactions. This means they can enjoy the full nutritional benefits of dairy products.
Diverse Dairy-Based Foods
A wide range of dairy-based foods can be enjoyed with lactase supplements. The following list highlights just a few examples, demonstrating the diversity available:
- Milk (cow’s milk, almond milk, soy milk, etc.): A staple beverage offering essential nutrients.
- Yogurt (Greek yogurt, plain yogurt, flavored yogurt): A probiotic-rich dairy product with numerous health benefits.
- Cheese (cheddar, mozzarella, parmesan, etc.): A versatile ingredient in various dishes, providing calcium and protein.
- Ice cream: A delicious treat that can be enjoyed with lactase support, satisfying cravings without compromising digestive comfort.
- Cottage cheese: A high-protein dairy product, useful in various dietary plans.
- Cream: A creamy addition to many recipes, from soups to sauces.
- Butter: A common culinary staple, providing healthy fats.
These are just a few examples. The flexibility offered by lactase supplements enables the consumption of a vast array of dairy-based foods, significantly expanding the dietary options available to those with lactose intolerance. This allows for a more balanced and varied diet, ultimately contributing to overall health and well-being.
Potential Side Effects and Considerations
While lactase supplements can be incredibly helpful for managing lactose intolerance, it’s crucial to understand the potential side effects and take necessary precautions. Knowing the potential risks and how to mitigate them empowers you to make informed decisions about incorporating these supplements into your routine.Understanding potential side effects allows for proactive management and ensures the supplements are used safely and effectively.
Careful consideration of individual needs, especially those with existing health conditions, is paramount.
Potential Digestive Discomfort
Lactase supplements, like any digestive aid, can sometimes cause mild digestive upset in some individuals. This can manifest as bloating, gas, or stomach cramps. These reactions are often temporary and resolve on their own. However, if the discomfort persists or worsens, it’s essential to discontinue use and consult a healthcare professional. This ensures that any underlying issues are addressed promptly.
Importance of Following Recommended Dosages
Adhering to the recommended dosage is critical for maximizing the benefits of lactase supplements and minimizing potential side effects. Overconsumption can lead to increased digestive discomfort. Always follow the instructions provided by the manufacturer and consult with your healthcare provider for personalized guidance. This ensures you’re receiving the correct amount for your specific needs.
Allergic Reactions and Sensitivities
Although less common, allergic reactions to lactase supplements are possible. Symptoms can range from mild skin rashes to more severe reactions, such as difficulty breathing or swelling. If you experience any unusual or concerning symptoms after taking the supplement, discontinue use immediately and seek medical attention. Recognizing and responding to allergic reactions promptly is crucial for safety.
Pre-existing Health Conditions and Consultation
Individuals with pre-existing health conditions, such as digestive disorders, should consult with a healthcare professional before starting any new supplement, including lactase supplements. Interactions with other medications or underlying conditions could influence the effectiveness and safety of the supplement. This consultation ensures the supplement aligns with overall health goals.
Comparison of Lactase Supplement Brands
| Brand | Potential Side Effects |
|---|---|
| Brand A | Mild stomach upset, gas in some users. |
| Brand B | Rare instances of allergic reactions, bloating in some users. |
| Brand C | Generally well-tolerated, but some users reported mild cramping. |
| Brand D | No significant side effects reported in clinical trials, but individual responses may vary. |
This table provides a general overview of potential side effects reported for different lactase supplement brands. Individual responses can vary. Always consult your healthcare professional before starting any new supplement, especially if you have pre-existing conditions.
Effectiveness and Research

Understanding the effectiveness of lactase supplements in managing lactose intolerance relies heavily on scientific research. Studies using various methodologies have provided valuable insights, but ongoing research continues to refine our understanding and address lingering questions. This section delves into the current state of research, highlighting key findings and methodologies.Research on lactase supplements consistently demonstrates their potential to alleviate lactose intolerance symptoms.
The degree of effectiveness, however, varies based on factors like the specific supplement, dosage, and individual tolerance.
Summary of Research Findings
Numerous studies have investigated the efficacy of lactase supplements in reducing symptoms associated with lactose intolerance. These studies often involve controlled trials, comparing individuals taking lactase supplements to those receiving a placebo or no treatment. The outcomes typically measure the reduction in symptoms such as bloating, gas, and abdominal pain after consuming lactose-containing foods.
Studies Demonstrating Positive Outcomes
A notable body of research showcases positive outcomes. One study, published in theJournal of Gastroenterology and Hepatology*, observed a significant reduction in reported gastrointestinal symptoms among participants consuming lactase supplements with lactose-rich meals. This study employed a double-blind, placebo-controlled design, ensuring objectivity in the results. Other studies have demonstrated similar improvements in symptom scores, particularly in the immediate post-meal period.
These findings generally corroborate the notion that lactase supplements can effectively reduce lactose intolerance symptoms.
Methodologies Used in Studies
The methodologies used in these studies are crucial for evaluating the reliability of findings. Commonly, studies utilize a double-blind, placebo-controlled design, where neither the participants nor the researchers know who is receiving the actual supplement versus the placebo. This approach minimizes bias and enhances the accuracy of results. Additionally, the amount of lactose consumed and the time elapsed after consumption are carefully controlled to isolate the impact of lactase supplementation.
These measures ensure that the observed changes are directly attributable to the supplement, not other factors.
Comparison of Different Research Findings
While many studies show positive effects, variations exist in the reported magnitude of symptom reduction. Factors like the type of lactase enzyme used, the dosage, and the individual’s baseline sensitivity to lactose can influence the outcomes. Some studies might focus on specific symptoms, like bloating, while others examine a broader range of discomfort. These variations highlight the need for further investigation to understand the optimal dosage and formulation for individual needs.
Importance of Ongoing Research
Ongoing research is crucial for improving our understanding of lactase supplements and their role in managing lactose intolerance. Future studies should explore the long-term effects of lactase supplementation, examine different populations (e.g., children, elderly), and investigate the interaction with other medications or dietary factors. These ongoing investigations will help tailor lactase supplement recommendations to specific needs and improve their overall effectiveness.
By continuously investigating different aspects, we can further refine our understanding of how these supplements can optimize digestive health.
Practical Application and Usage: The Benefits Of Lactase Supplements
Lactase supplements offer a practical solution for managing lactose intolerance, allowing individuals to enjoy dairy products without discomfort. Understanding how to use these supplements effectively is key to maximizing their benefits and minimizing potential side effects. This section details the practical application of lactase supplements, covering dosage, integration into daily routines, and selection of the appropriate product.
Step-by-Step Instructions for Taking Lactase Supplements
Taking lactase supplements is generally straightforward. Most products are designed for easy consumption. A typical regimen involves taking the supplement immediately before or with a meal containing lactose. This allows the lactase enzyme to break down the lactose in the food, reducing the likelihood of digestive issues. Always follow the specific instructions provided by the manufacturer on the product label.
Integrating Lactase Supplements into Daily Routines
Integrating lactase supplements into daily life is relatively simple. For example, if you regularly consume dairy products for breakfast, take the supplement with your breakfast cereal or yogurt. For lunch or dinner, take the supplement with any dairy-containing foods like cheese, milk, or ice cream. Timing is crucial, as taking the supplement before or with the meal allows the lactase to act on the lactose while it is being consumed.
Adjust the timing as needed to suit your specific dietary habits.
Lactase supplements can be a game-changer for those struggling with lactose intolerance. They break down lactose, making dairy products more digestible. This can lead to fewer digestive issues, and more energy. But sometimes, dealing with the after effects of dairy can cause a temporary state of mental fogginess or a feeling of being disconnected. This is similar to the concept of “spacing out”, which is often a temporary disconnect from the environment or surroundings what is spacing out.
Fortunately, a well-timed lactase supplement can help you navigate those tricky dairy-related moments, and keep you feeling your best.
Choosing the Right Lactase Supplement
Several factors influence the selection of the appropriate lactase supplement. Consider the amount of lactose you typically consume in a day. Higher lactose intake might necessitate a higher dosage of the supplement. Also, look for products that are formulated with high potency and are well-tolerated by most users. Read reviews from other users to understand potential side effects or issues with specific brands.
Consulting with a doctor or registered dietitian can provide personalized recommendations.
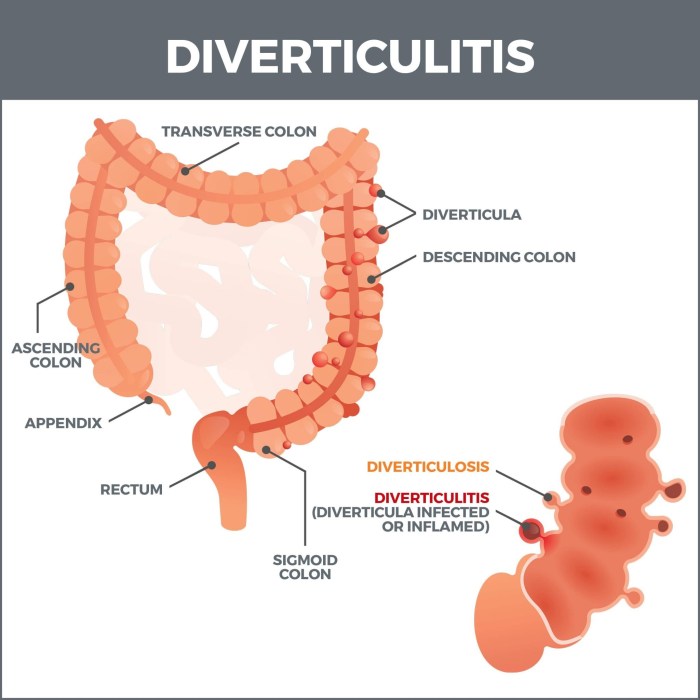
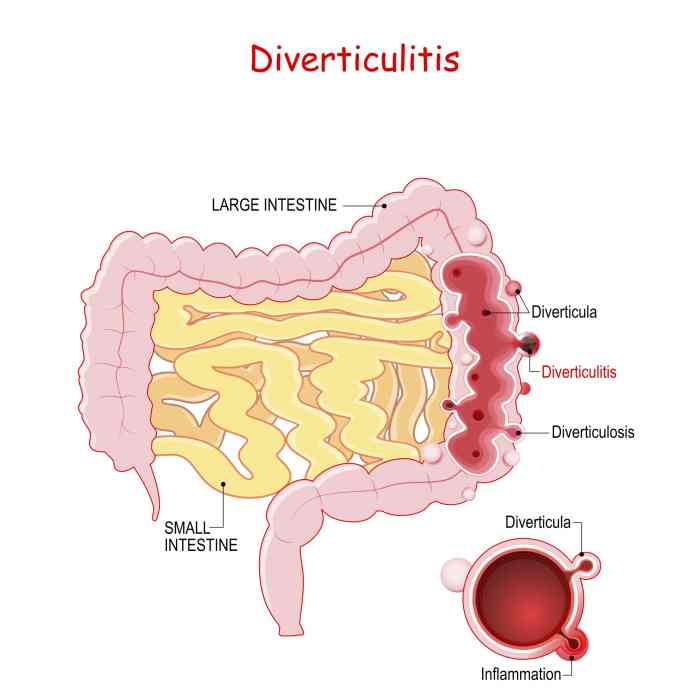
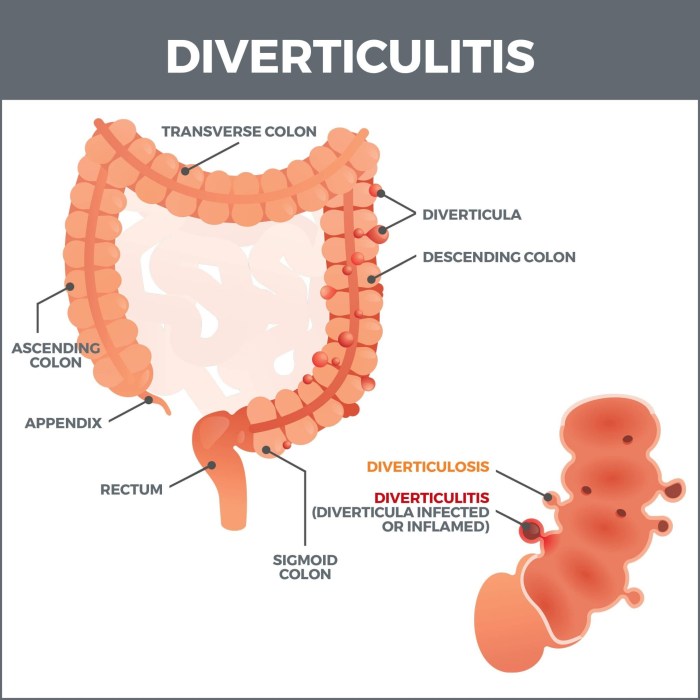
Lactase supplements can be a real game-changer for those struggling with lactose intolerance. They help your body break down lactose, preventing digestive distress. This is particularly helpful if you’re exploring treatment options for conditions like diversion colitis, which can significantly impact your gut health. Learning about diversion colitis treatment options can offer insights into managing symptoms and improving overall well-being.
Ultimately, understanding how lactase supplements can improve digestion is key to feeling your best.
Dosage Recommendations for Different Brands
| Brand | Dosage (per serving) | Notes |
|---|---|---|
| Lactaid | 1 tablet (1,000 LU) before or with a meal containing lactose | Commonly available and effective for many users. |
| DairyEase | 1 capsule (1,500 LU) before or with a meal containing lactose | Known for higher lactase content, potentially better for higher lactose intake. |
| Lactazyme | 1 tablet (2,000 LU) before or with a meal containing lactose | Higher potency than other brands; consult a doctor for use in specific situations. |
| Lactase Advance | 1 tablet (1,200 LU) before or with a meal containing lactose | A balance between cost and potency, suitable for moderate lactose intake. |
| Lactaid Chewables | 1 chewable tablet (1,000 LU) before or with a meal containing lactose | Easier to consume, suitable for individuals who prefer chewable forms. |
Note: LU stands for Lactase Units. The dosage listed in the table is a general guideline. Always follow the manufacturer’s instructions on the product label for specific dosage recommendations. Consult a healthcare professional for personalized guidance.
Integration into a Healthy Lifestyle
Lactase supplements can be a valuable tool for individuals with lactose intolerance, enabling them to enjoy dairy products while maintaining a healthy lifestyle. However, their effectiveness is contingent upon integrating them into a broader strategy of balanced nutrition, regular exercise, and adequate hydration. This approach ensures the supplements’ benefits are maximized and potential downsides are minimized.A balanced diet is paramount when using lactase supplements.
Dairy products are rich in calcium, vitamin D, and protein, essential nutrients for bone health, muscle function, and overall well-being. However, the lactose in dairy can cause digestive distress in individuals with lactose intolerance. Lactase supplements help break down lactose, allowing the body to absorb these crucial nutrients.
Importance of Balanced Diet
Lactase supplements shouldn’t replace a balanced diet rich in diverse foods. A healthy diet should include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. These foods provide essential vitamins, minerals, and fiber that support overall health. Focusing solely on dairy products, even with lactase, can lead to nutrient deficiencies from a lack of variety.
A balanced diet provides the body with all the necessary components for optimal functioning.
Role of Exercise and Hydration
Regular exercise plays a vital role in maintaining overall health, boosting energy levels, and improving digestion. Hydration is equally important, as water is essential for various bodily functions, including nutrient absorption and waste elimination. These two factors can be synergistic with the use of lactase supplements, allowing for the full absorption and utilization of nutrients from dairy products.
Maintaining a healthy weight, for instance, can help reduce symptoms of digestive distress.
How Lactase Supplements Support a Healthy Lifestyle
Lactase supplements can help individuals with lactose intolerance enjoy a wider variety of dairy products, including milk, yogurt, and cheese, without suffering digestive discomfort. This can lead to improved calcium intake and a more balanced nutritional profile. This is especially beneficial for growing children, pregnant women, and older adults, who need sufficient calcium for strong bones and overall health.
Examples of Dietary Plans
Lactase supplements can be integrated into various dietary plans. For example, a vegetarian or vegan diet can benefit from incorporating dairy products with lactase supplements, offering a wider range of protein and calcium sources. A balanced diet, rich in vegetables, fruits, whole grains, and lean proteins, can provide adequate nutrients, while lactase supplements facilitate dairy consumption. Similarly, a person following a low-carb diet can still consume yogurt or milk with lactase.
Dietary Tips for Lactose Intolerance Management, The benefits of lactase supplements
- Gradual Introduction: Start with small portions of dairy products and gradually increase the amount as tolerated. This allows the body to adjust to the lactase.
- Timing Matters: Consume lactase supplements alongside dairy products to maximize their effectiveness.
- Variety is Key: Maintain a balanced diet, incorporating a variety of fruits, vegetables, and whole grains alongside dairy products.
- Listen to Your Body: Pay attention to your body’s response to dairy products and lactase supplements. Adjust intake accordingly.
- Consult Professionals: Consult with a doctor or registered dietitian for personalized dietary advice.
These tips can help individuals with lactose intolerance manage their condition and enjoy a healthy lifestyle, even with dairy products.
Conclusive Thoughts
In conclusion, lactase supplements can be a valuable tool for managing lactose intolerance and expanding dietary options. While they offer significant benefits in terms of digestive relief and dietary flexibility, it’s crucial to understand the potential side effects and to consult with a healthcare professional before starting any new supplement regimen. By understanding the science behind these supplements, comparing different forms, and weighing the potential risks and rewards, you can make informed decisions about incorporating lactase supplements into your life.
Remember, a balanced diet and lifestyle are essential, even when using these supplements, to achieve optimal results.