How to relieve gas pains fast? This guide delves into the various causes, effective home remedies, dietary considerations, lifestyle adjustments, medical interventions, and prevention strategies to combat those uncomfortable gas pains quickly and safely. We’ll explore common triggers, from specific foods to underlying medical conditions, and equip you with practical solutions for swift relief.
Understanding the root causes of gas pain, whether dietary or medical, is crucial for effective management. This detailed guide offers insights into the physiological processes involved and provides a comprehensive overview of different types of gas pain. Furthermore, we’ll discuss the efficacy of various home remedies and provide a comparative analysis of their pros and cons.
Understanding Gas Pains
Gas pains, a common ailment affecting many, can range from mild discomfort to severe agony. Understanding the underlying causes, physiological processes, and diverse manifestations of gas pain is crucial for effective management and seeking appropriate medical attention when necessary. This section delves into the intricacies of gas pain, providing a comprehensive overview.Common causes of gas pain encompass dietary choices, medical conditions, and lifestyle factors.
Diet plays a significant role, with certain foods triggering increased gas production in the digestive tract. Medical conditions like irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD) can lead to chronic gas pain. Lifestyle habits such as insufficient hydration, lack of physical activity, and stress can also contribute to gas discomfort.
Causes of Gas Pain
Dietary factors often contribute to gas pain. Certain foods, like beans, lentils, broccoli, and cabbage, contain complex carbohydrates that are difficult for the body to digest. This undigested material ferments in the colon, producing gas and leading to bloating, cramping, and flatulence. Dairy products, especially for individuals with lactose intolerance, can also cause gas pain. Medical conditions like IBS and IBD can lead to chronic gas pain, often accompanied by other symptoms such as diarrhea or constipation.
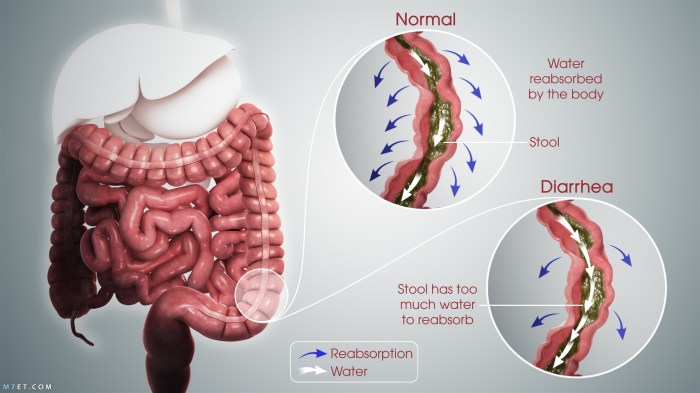
The exact mechanisms are complex but involve issues with intestinal motility and inflammation. Lifestyle choices can also affect gas pain. Dehydration can lead to harder stools, making it more difficult for the digestive system to process food and potentially causing gas. A sedentary lifestyle can also contribute to gas discomfort. Stress and anxiety can influence gut motility, resulting in increased gas production and discomfort.
Physiological Processes Leading to Gas Pain
Gas pain arises from the build-up of gas within the digestive tract. Swallowed air, as well as gas produced during the digestion of certain foods, contributes to this accumulation. The expanding gas exerts pressure on the intestinal walls, triggering discomfort, cramping, and bloating. The specific type of gas pain experienced often depends on the underlying cause.
Types of Gas Pain
Gas pain manifests in various forms, including cramping, bloating, and sharp pain. Cramping is a common symptom characterized by intermittent, rhythmic contractions of the abdominal muscles. Bloating involves a sensation of fullness and distension in the abdomen. Sharp pain is often sudden and intense, potentially radiating to other parts of the body. Understanding the nature of the pain can help in identifying the potential cause.
Signs and Symptoms of Gas Pain
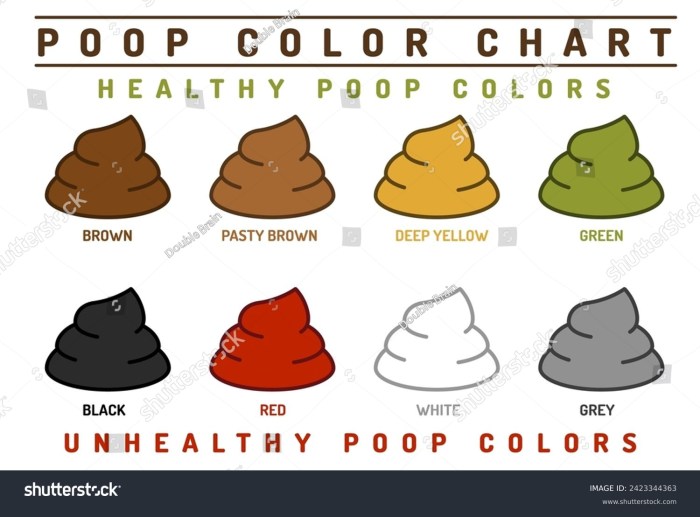
Common signs and symptoms of gas pain include bloating, cramping, flatulence, and abdominal distension. These symptoms can vary in intensity and duration depending on the underlying cause. Other potential signs include nausea, vomiting, and fever. In some cases, gas pain can be accompanied by other digestive issues, such as diarrhea or constipation.
Comparison of Gas Pain Causes
| Cause | Symptoms | Duration | Severity |
|---|---|---|---|
| Dietary Factors | Bloating, cramping, flatulence | Variable | Mild to moderate |
| Medical Conditions | Severe cramping, bloating, fever | Variable | Moderate to severe |
| Lifestyle Choices | Mild bloating, occasional discomfort | Variable | Mild |
Fast Relief Methods
Dealing with gas pains can be incredibly uncomfortable, and sometimes, quick relief is crucial. Fortunately, several readily available home remedies can provide effective, temporary relief. Understanding the mechanisms behind these remedies can empower you to make informed choices about your treatment.
Common Home Remedies
Many common household items can help alleviate gas pain. These remedies work through various physiological pathways, aiming to reduce bloating, cramping, and discomfort.
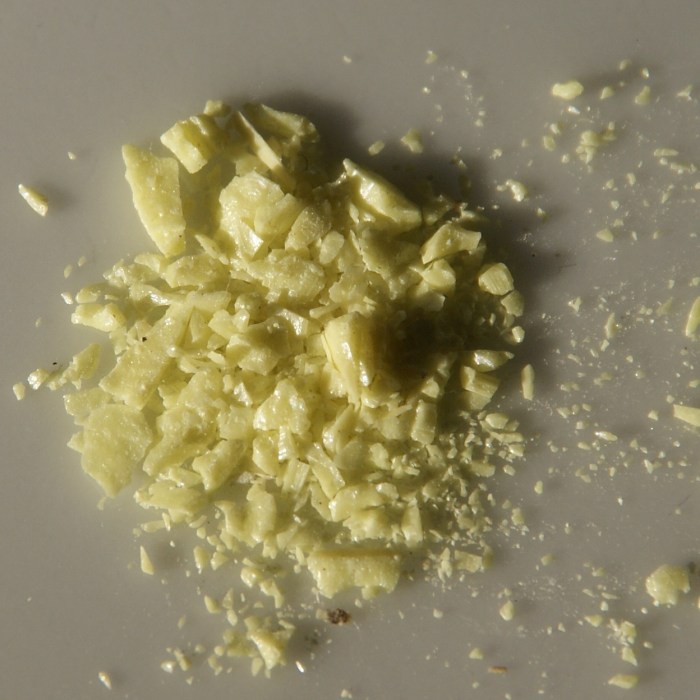
- Ginger: Ginger’s anti-inflammatory properties can soothe digestive upset. Gingerol, the active compound, is believed to relax smooth muscles in the digestive tract, reducing cramping. Ginger is commonly consumed in tea or as a supplement. To use ginger for gas relief, simply steep a small piece of fresh ginger in hot water for a few minutes to make a tea.
Quick relief for gas pains can be a lifesaver, right? While some swear by certain foods or drinks, I’ve found that gentle stretching and mindful breathing often work wonders. However, don’t forget to consider the potential risks of neck cracking, which can sometimes be connected to health issues. For a comprehensive overview of the potential downsides of cracking your neck, check out this article on is cracking your neck bad for you.
Ultimately, if the gas pains persist, consulting a doctor is always a good idea, no matter what you try first.
Alternatively, you can consume ginger candy or chew on fresh ginger root. Note that excessive ginger consumption might lead to digestive issues for some individuals.
- Peppermint Tea: Peppermint is a well-known remedy for digestive discomfort. Peppermint oil has a relaxing effect on the smooth muscles of the digestive system. This relaxation can help to reduce cramping and ease gas pain. Peppermint tea is a simple and effective remedy. Brew a cup of peppermint tea and sip it slowly.
Dealing with those pesky gas pains? Try some gentle, over-the-counter remedies like peppermint tea or ginger ale. Sometimes, adjusting your diet by cutting back on beans and cruciferous veggies can help too. Knowing how to delay your period can be helpful for some, and there are resources available to explore that option here. But if the pain persists, it’s always best to consult a doctor.
Ultimately, the best approach to relieving gas pains is to find what works for you!
It’s important to note that peppermint might not be suitable for everyone, especially those with pre-existing digestive conditions or allergies.
- Over-the-Counter Medications: Over-the-counter medications, such as simethicone, are designed to break down gas bubbles in the digestive tract. Simethicone works by coating the gas bubbles and making them easier to pass through the digestive system. These medications provide rapid relief from gas pain. Always follow the dosage instructions carefully and consult a healthcare professional if you have any concerns or pre-existing conditions.
Comparative Analysis of Effectiveness and Safety
Different remedies offer varying degrees of effectiveness and potential risks. The table below provides a comparative overview of common home remedies.
| Method | Pros | Cons | Effectiveness |
|---|---|---|---|
| Ginger | Anti-inflammatory, may reduce nausea, readily available | Potential for digestive upset in some, less potent than simethicone | Moderate |
| Peppermint Tea | Relax smooth muscles, reduce cramping, relatively safe | May not be suitable for everyone, less potent than simethicone | Moderate |
| Over-the-counter Medications (e.g., simethicone) | Fast relief, often effective | Potential side effects, not suitable for everyone, requires adherence to dosage instructions | High |
Dietary Considerations
Dietary choices play a significant role in managing gas pain. Understanding which foods contribute to gas formation and adopting strategies to minimize their consumption can significantly reduce discomfort. By incorporating healthy alternatives and avoiding problematic foods, you can effectively control gas pain and improve your overall digestive health.Foods high in fiber, particularly insoluble fiber, are often culprits in gas production.
This is because our bodies lack the enzymes to fully break down certain types of fiber, leading to fermentation in the gut and the release of gas. However, fiber is essential for a healthy digestive system. The key is finding a balance between getting enough fiber and minimizing gas-inducing varieties.
Foods Commonly Contributing to Gas Pain
Certain foods are notorious for their gas-producing properties. These include beans, lentils, broccoli, cabbage, cauliflower, onions, and garlic. These foods contain complex carbohydrates that are difficult for the body to digest, resulting in the production of gas during fermentation in the large intestine. While these foods are often nutritious, their potential for causing gas should be considered.
Strategies for Minimizing Gas
Implementing strategies to minimize gas production while maintaining a healthy diet is achievable. A crucial strategy is to gradually increase your fiber intake. This allows your digestive system to adjust to higher fiber content and minimize the risk of excessive gas. Also, chewing food thoroughly and eating smaller portions can aid digestion and reduce gas formation.
Sample Meal Plan Minimizing Gas-Producing Foods
This sample meal plan provides examples of how to incorporate healthy foods while minimizing gas-inducing ones. Adjust portions and choices to suit your individual needs and preferences. Note that this is a sample, and professional dietary advice is always recommended.
| Meal | Dish | Description |
|---|---|---|
| Breakfast | Oatmeal with Berries | A bowl of oatmeal with mixed berries provides a balanced breakfast. |
| Lunch | Grilled Chicken Salad with Quinoa | Lean protein from grilled chicken, fiber from quinoa, and leafy greens. |
| Dinner | Baked Fish with Steamed Asparagus and Brown Rice | Healthy protein from fish, light vegetables, and a small portion of brown rice. |
Foods to Avoid to Reduce Gas
Avoiding certain foods can significantly reduce gas production. A list of common culprits is provided below, but this is not exhaustive. Consult with a healthcare professional or registered dietitian for personalized recommendations.
- Beans and Legumes: Foods like kidney beans, black beans, and lentils are high in complex carbohydrates that are difficult to digest, leading to gas production.
- Cruciferous Vegetables: Broccoli, cabbage, cauliflower, and Brussels sprouts contain complex sugars that can be tough to digest, potentially causing excessive gas.
- Fruits with High Fructose Content: Fruits like apples, pears, and peaches contain fructose, a sugar that can be challenging for some individuals to digest, leading to gas.
- Carbonated Beverages: Carbonated drinks introduce excess air into the digestive system, contributing to bloating and gas.
- Dairy Products: Individuals with lactose intolerance may experience gas after consuming dairy products due to the difficulty in digesting lactose.
Lifestyle Adjustments
Dealing with gas pain can sometimes feel like a constant battle. While dietary changes are crucial, lifestyle factors can also significantly impact your digestive health and gas production. Understanding how these factors influence your system can help you identify potential triggers and make proactive adjustments.Lifestyle choices like stress levels, activity levels, and even sleep patterns can play a role in the overall comfort and function of your digestive tract.
These adjustments, when implemented correctly, can often result in noticeable improvements in gas relief.
Factors Exacerbating Gas Pain
Certain lifestyle habits can worsen gas pain. Stress, for example, can disrupt the normal rhythm of the digestive system. This can lead to increased bowel movements and the release of trapped air. Similarly, a lack of regular physical activity can slow down the digestive process, allowing for more gas to build up. Poor sleep habits can also negatively impact digestive health.
Quick relief from gas pains often involves simple remedies like peppermint tea or gentle exercise. Understanding how your body processes food and adjusting your diet can also help. Knowing how long the HBV vaccine’s protection lasts is crucial for scheduling booster shots, as detailed in this helpful article how long the hbv vaccine last. Ultimately, prioritizing a healthy digestive system through mindful eating and regular movement can significantly reduce instances of gas pain.
Impact on the Digestive System
Stress hormones, released during periods of stress, can affect the muscles involved in digestion. This can cause spasms and slow down the movement of food through the intestines, leading to the accumulation of gas. Lack of exercise can lead to a sluggish digestive system, allowing food to sit longer in the gut and ferment, resulting in gas production.
Poor sleep quality can further disrupt the delicate balance of gut bacteria, leading to increased gas.
Modifying Lifestyle Choices
Making small, manageable changes to your daily routine can significantly reduce gas pain. Prioritizing stress reduction techniques, incorporating regular exercise, and ensuring sufficient sleep can all contribute to a healthier digestive system. Understanding the impact of these factors allows for targeted interventions to alleviate symptoms.
Lifestyle Modifications to Reduce Gas
- Stress Management: Incorporating stress-reducing activities like meditation, yoga, deep breathing exercises, or spending time in nature can help regulate digestive function. Stress management techniques help calm the nervous system, allowing the digestive system to operate more smoothly. Even a short walk in the park or listening to calming music can be effective.
- Regular Exercise: Physical activity stimulates bowel movements, promoting the expulsion of gas. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. This can include brisk walking, swimming, cycling, or dancing. Regular exercise helps maintain a healthy gut microbiome and can improve digestion.
- Adequate Sleep: Aim for 7-9 hours of quality sleep each night. Sleep deprivation can disrupt the gut’s natural rhythm and negatively impact digestive function. Establish a consistent sleep schedule and create a relaxing bedtime routine to optimize sleep quality.
- Hydration: Drinking plenty of water throughout the day helps soften stools and promotes regular bowel movements, reducing the buildup of gas. Water helps keep things moving through the digestive tract.
- Mindful Eating: Eating slowly and mindfully, paying attention to your body’s signals, can reduce the amount of air swallowed during meals. Chewing food thoroughly before swallowing helps minimize air intake. This also allows for better nutrient absorption and prevents overeating, both of which can impact digestion.
Importance of Regular Exercise
Regular exercise is essential for maintaining digestive health. It strengthens the abdominal muscles, promoting better bowel regularity and reducing the chances of gas buildup. It also enhances the overall well-being, which in turn positively impacts the digestive system. Exercise, when incorporated into a healthy lifestyle, has many benefits.
Medical Interventions
Sometimes, despite lifestyle changes and dietary adjustments, gas pain persists or worsens. In such cases, medical intervention becomes necessary to address the underlying cause and alleviate discomfort. Understanding when and how to seek medical help is crucial for effective management and preventing potential complications.Medical interventions for gas pain vary depending on the root cause. It’s important to remember that a doctor can properly diagnose the cause of the gas pain and recommend the most appropriate treatment.
Self-treating without a proper diagnosis can sometimes lead to misdiagnosis and ineffective treatment.
When Medical Intervention Is Necessary
Persistent or severe gas pain, accompanied by other symptoms like fever, abdominal pain, weight loss, or blood in the stool, warrants immediate medical attention. These symptoms could indicate more serious conditions requiring medical intervention, and self-treatment might delay proper diagnosis and treatment. For instance, if a person experiences severe abdominal pain that radiates to the back, along with fever, they should seek immediate medical attention, as this could be a sign of appendicitis.
Similarly, significant blood in the stool demands immediate medical evaluation to rule out conditions like diverticulitis or colon cancer.
Different Medical Approaches
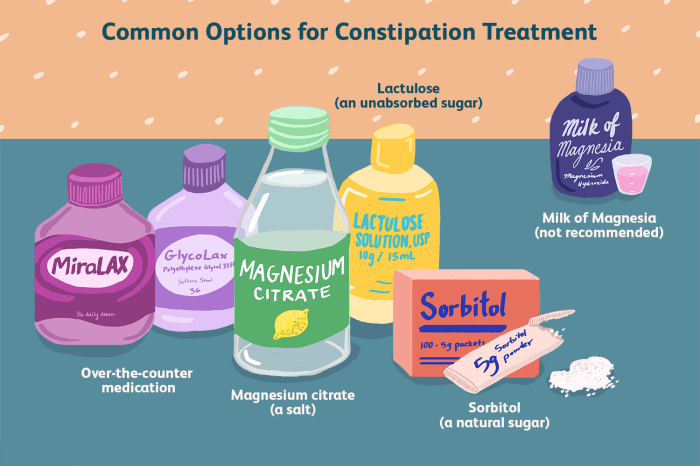
Medical approaches for treating gas pain are diverse, ranging from over-the-counter medications to more intensive treatments.
- Over-the-Counter Medications: Many over-the-counter medications, such as simethicone, can help reduce gas discomfort by breaking down gas bubbles. However, these medications are often effective for mild to moderate cases and should be used according to the product instructions. It’s important to consult a doctor before taking any over-the-counter medications, especially if you have underlying health conditions.
- Prescription Medications: In cases of more severe or chronic gas pain, a doctor might prescribe medications to address the underlying cause. These medications can target specific conditions like irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD). Examples include laxatives, antispasmodics, and medications to reduce inflammation.
- Diagnostic Procedures: In some situations, a doctor may recommend diagnostic procedures to identify the root cause of the gas pain. These procedures can include colonoscopies, endoscopies, or imaging tests like X-rays or CT scans. These procedures help pinpoint the cause of the gas pain and enable the doctor to tailor the treatment plan to the specific condition.
Role of a Doctor in Managing Gas Pain
A doctor plays a critical role in managing gas pain by:
- Thorough Assessment: A doctor conducts a thorough assessment, taking into account the patient’s medical history, symptoms, and lifestyle factors to understand the underlying cause of the gas pain.
- Diagnosis: Based on the assessment, the doctor formulates a diagnosis, determining whether the gas pain is related to a specific condition or is simply a symptom of a different issue.
- Treatment Plan: The doctor develops a personalized treatment plan tailored to the individual’s needs and the underlying cause of the gas pain. This might include lifestyle modifications, dietary changes, medications, or referrals to other specialists.
Importance of Seeking Medical Advice
Ignoring persistent or severe gas pain can sometimes lead to complications or delay effective treatment. Seeking medical advice is essential for preventing potential problems and ensuring proper management of the condition. For example, neglecting persistent gas pain accompanied by fever and abdominal pain could lead to a misdiagnosis or delayed treatment for appendicitis, potentially resulting in serious complications.
Therefore, timely consultation with a doctor is crucial for prompt diagnosis and treatment.
Prevention Strategies
Preventing gas pain often involves a proactive approach focusing on dietary choices, hydration, and stress management. A balanced lifestyle that incorporates these elements can significantly reduce the frequency and intensity of discomfort. By understanding the triggers and implementing preventative measures, you can minimize the impact of gas pain on your daily life.Implementing preventive strategies for gas pain is crucial for long-term comfort and well-being.
These strategies are not just about reducing symptoms; they’re about fostering a healthier digestive system and overall healthier lifestyle. A preventative approach to gas pain is essential for maintaining daily comfort and overall well-being.
Dietary Considerations for Gas Pain Prevention
A balanced diet plays a pivotal role in preventing gas pain. Foods high in fiber are important for digestive health, but consuming too much too quickly can lead to increased gas production. Gradually increasing fiber intake is often recommended. Certain foods, like beans, lentils, broccoli, and cabbage, are known to be particularly problematic for some individuals. Monitoring your intake of these foods and identifying personal sensitivities can be helpful.
- Gradual Fiber Intake Increase: Slowly introduce high-fiber foods into your diet. Start with smaller portions and gradually increase the amount as your digestive system adjusts. This approach minimizes the risk of sudden digestive upset.
- Identification of Trigger Foods: Keep a food diary to track your diet and identify foods that seem to cause gas pain. Note the timing of meals, the types of food consumed, and any accompanying symptoms. This detailed tracking can help you pinpoint specific triggers.
- Portion Control: Moderation is key when it comes to certain foods that are gas-producing. Avoid overeating, especially meals with known triggers. This can help to minimize the amount of gas produced.
Importance of Hydration in Preventing Gas Pain, How to relieve gas pains fast
Adequate hydration is essential for overall digestive health and can significantly reduce gas pain. Water helps move food through the digestive tract, preventing stagnation and reducing the likelihood of gas buildup. Dehydration can exacerbate existing gas pain and make it more difficult for your body to process foods efficiently. Drinking plenty of water throughout the day is crucial.
- Consistent Water Intake: Aim for a consistent intake of water throughout the day, not just when you feel thirsty. Carry a water bottle and sip on it regularly. This habit will keep your body hydrated and support proper digestion.
- Avoid Sugary Drinks: Sugary drinks and sodas can disrupt the natural balance of fluids in your body and contribute to gas production. Limit your consumption of these drinks to promote better digestive health.
Stress Management Techniques for Gas Pain Prevention
Stress can significantly impact the digestive system, leading to increased gas production and discomfort. Stress hormones can alter the motility of the intestines, making it more difficult for food to pass through smoothly. Stress management techniques can help regulate digestive function and reduce gas pain.
- Mindfulness and Meditation: Incorporating mindfulness and meditation practices can help reduce stress levels and promote relaxation. These practices can help calm the mind and body, which can have a positive effect on digestive function.
- Regular Exercise: Physical activity is a proven stress reliever and can improve digestive health. Exercise promotes blood flow to the digestive system, which aids in the efficient movement of food.
- Sufficient Sleep: Adequate sleep is crucial for overall health, including digestive health. When you’re well-rested, your body can better manage stress and maintain optimal digestive function.
Final Review: How To Relieve Gas Pains Fast
In conclusion, managing gas pain effectively involves a multifaceted approach that combines understanding the causes, employing safe and effective home remedies, making informed dietary choices, adjusting lifestyle habits, and knowing when to seek medical intervention. By implementing the strategies Artikeld in this guide, you can significantly reduce the frequency and severity of gas pain and enjoy a more comfortable and healthy digestive system.
Remember that a balanced diet, hydration, and stress management play a key role in preventing gas pain in the long run.