Diabetic retinopathy symptoms and stages: This comprehensive guide delves into the various stages of diabetic retinopathy, exploring its symptoms, causes, and how it affects vision. Understanding the progression of this eye condition is crucial for early detection and effective management.
We’ll cover the different types of diabetic retinopathy, examining their unique symptoms and risk factors. This includes a detailed look at the impact of the disease on visual acuity at each stage. We’ll also touch upon the importance of early detection, highlighting the critical role of regular eye exams in preventing vision loss.
Introduction to Diabetic Retinopathy

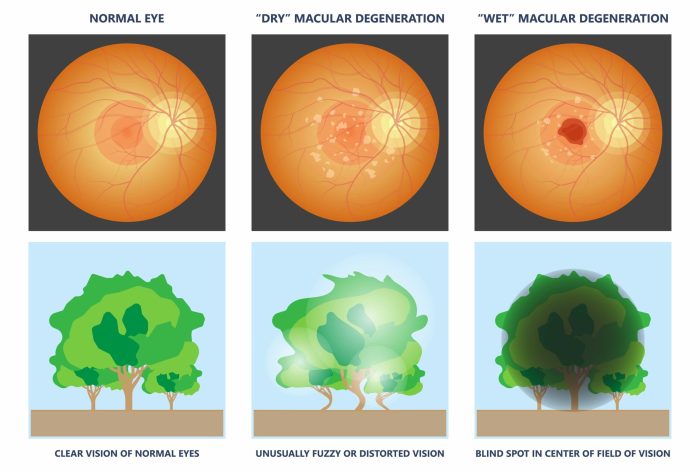
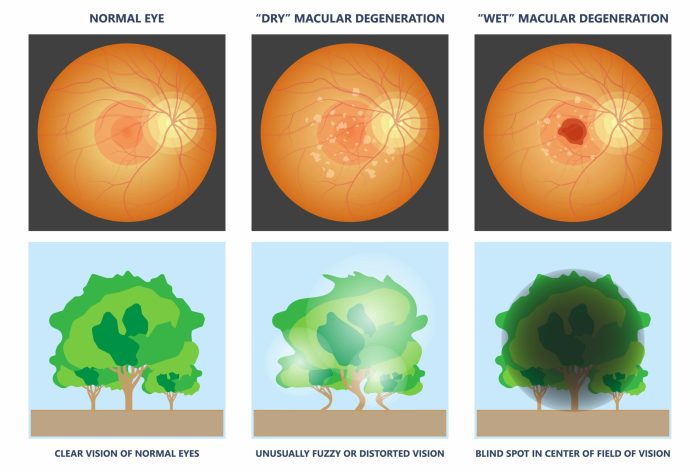
Diabetic retinopathy is a serious complication of diabetes that affects the retina, the light-sensitive tissue lining the back of the eye. It’s a leading cause of vision loss in working-age adults globally. Understanding the underlying mechanisms, prevalence, and types of diabetic retinopathy is crucial for early detection and effective management. Proactive measures can significantly reduce the risk of vision impairment and improve overall health outcomes for individuals with diabetes.The development of diabetic retinopathy is intricately linked to chronic hyperglycemia (high blood sugar).
Understanding diabetic retinopathy symptoms and stages is crucial for early intervention. Blurred vision, floaters, and even trouble seeing straight are common early signs. Learning about skin conditions like vitiligo vs albinism what s the difference here can be interesting, but it’s important to remember that these are different health concerns. Ultimately, recognizing the symptoms of diabetic retinopathy, like gradual vision changes, is key to managing the condition effectively.
High blood sugar levels damage the tiny blood vessels in the retina, leading to abnormal blood vessel growth, leakage, and scarring. This damage interferes with the retina’s ability to transmit clear images to the brain, potentially resulting in vision loss. The longer a person has diabetes and the less well-controlled their blood sugar levels are, the greater the risk of developing diabetic retinopathy.Globally, diabetic retinopathy is a significant public health concern.
The prevalence varies across different regions and populations, but it’s estimated that millions of people worldwide suffer from this condition. Its impact extends beyond visual impairment, affecting daily activities, quality of life, and economic productivity. The high cost of treatment and potential loss of independence underscore the importance of preventative measures and early detection.
Types of Diabetic Retinopathy
Diabetic retinopathy progresses through several stages, each with varying degrees of retinal damage. Classifying these stages is crucial for timely intervention and effective management strategies. The stages are broadly categorized into early, moderate, severe, and proliferative retinopathy, each with specific characteristics.
Comparison of Diabetic Retinopathy Types
| Type | Description | Symptoms | Risk Factors |
|---|---|---|---|
| Early | Characterized by minor changes in the retinal blood vessels, such as microaneurysms (small bulges) and small hemorrhages. These changes may not cause noticeable symptoms, but they indicate the initial stages of the disease. | Often asymptomatic. Patients might not experience any noticeable vision problems at this stage. | Poorly controlled blood sugar levels, duration of diabetes, high blood pressure, high cholesterol, and family history of diabetes. |
| Moderate | Shows more pronounced changes in the retinal blood vessels. These include more numerous microaneurysms, hemorrhages, and hard exudates (yellowish deposits). These changes might begin to impact vision subtly. | Mild vision blurring, or slight distortion of images. Patients might notice difficulty reading small print or seeing colors clearly. | Poorly controlled blood sugar levels, duration of diabetes, high blood pressure, high cholesterol, and family history of diabetes. Uncontrolled blood pressure can exacerbate the progression of retinopathy. |
| Severe | Significant damage to retinal blood vessels, leading to increased hemorrhages, hard exudates, and macular edema (swelling of the macula, the central part of the retina responsible for sharp central vision). Vision loss becomes more apparent. | Decreased visual acuity, significant distortion of images, and possible floaters (spots or specks that appear in the visual field). | Poorly controlled blood sugar levels, long duration of diabetes, high blood pressure, high cholesterol, lack of regular eye exams, and failure to adhere to treatment plans. |
| Proliferative | Advanced stage characterized by new blood vessel growth (neovascularization) on the retina. These fragile vessels are prone to leakage and bleeding, potentially leading to retinal detachment. This stage carries the highest risk of vision loss. | Significant vision loss, distortion, and floaters. Patients might experience sudden vision changes or complete vision loss in extreme cases. Symptoms can include flashing lights or a veil over the vision. | Poorly controlled blood sugar levels, long duration of diabetes, high blood pressure, high cholesterol, lack of regular eye exams, and failure to adhere to treatment plans. Smoking is another significant risk factor. |
Symptoms of Diabetic Retinopathy

Diabetic retinopathy, a serious complication of diabetes, gradually damages the blood vessels in the retina, the light-sensitive tissue lining the back of the eye. Early detection is crucial to prevent vision loss. Understanding the symptoms at different stages is vital for timely intervention.
Common Early Symptoms
Early diabetic retinopathy often presents with subtle symptoms that may be easily overlooked. These initial signs can include blurred vision, which might appear as a gradual change in sharpness or clarity. Some individuals experience a gradual decrease in their visual acuity, making fine details harder to distinguish. Color perception might also be affected, with colors appearing slightly less vibrant or saturated.
These subtle changes are often the first indicators of the disease, and recognizing them is key to seeking prompt medical attention.
Symptoms in Later Stages
As diabetic retinopathy progresses, the symptoms become more pronounced and impactful on vision. In moderate stages, vision loss becomes more noticeable, with a decrease in overall clarity. Straight lines might appear wavy or distorted, and the sufferer may experience difficulty reading or driving. More advanced stages can lead to significant vision impairment, blurring or distortion of vision, floaters (small, dark spots or shapes moving in the field of vision), and even complete vision loss in severe cases.
Importance of Early Detection
Early detection of diabetic retinopathy is paramount for preventing severe vision loss. Prompt diagnosis and management of the condition can slow its progression and help preserve vision. Individuals with diabetes should undergo regular eye exams to monitor for any signs of the disease. Regular checkups can help detect early changes and allow for timely intervention, preventing significant vision loss and maintaining a better quality of life.
Variability of Symptoms Based on Type
Symptoms of diabetic retinopathy can vary slightly based on the specific type of the disease. Non-proliferative diabetic retinopathy often begins with subtle changes in vision, progressing to more noticeable issues as the condition advances. Proliferative diabetic retinopathy, characterized by the growth of abnormal blood vessels, can present with floaters, blurry vision, or even sudden vision loss. Understanding the different types and their associated symptoms can aid in more precise diagnosis and personalized treatment strategies.
Symptoms Across Stages
| Stage | Symptoms | Description |
|---|---|---|
| Early | Blurred vision | Gradual changes in sharpness or clarity of vision, often subtle and overlooked. Potential decrease in visual acuity and altered color perception. |
| Moderate | Vision loss | Decreased overall clarity, straight lines appearing wavy or distorted. Difficulty with tasks like reading or driving. |
| Advanced | Floaters, significant vision impairment | Floaters (small, dark spots or shapes moving in the field of vision), substantial blurring or distortion of vision, potential for complete vision loss. |
Stages of Diabetic Retinopathy
Diabetic retinopathy, a serious complication of diabetes, progressively damages the tiny blood vessels in the retina, the light-sensitive tissue lining the back of the eye. Understanding the different stages of this disease is crucial for early detection and timely intervention, potentially preventing vision loss. Early diagnosis allows for prompt treatment, potentially slowing or halting the progression of the disease.
Non-Proliferative Diabetic Retinopathy
This is the initial stage, characterized by the development of microaneurysms, small bulges in the weakened blood vessels of the retina. These microaneurysms are often the first visible signs of damage. As the disease progresses, the blood vessels may begin to leak fluid and blood into the retina, causing swelling (edema). These changes are often subtle and may not impact vision significantly at this stage.
Small hemorrhages, or tiny spots of bleeding, may also appear in the retina.
Diabetic retinopathy, a serious complication of diabetes, shows up in various stages with symptoms ranging from mild vision changes to severe loss. Early detection is key, and understanding the different stages, like blurry vision or even floaters, is crucial for managing the condition. For a boost in your overall health, you might consider preventative measures like getting the nasal flu vaccine, what is the nasal flu vaccine flumist , to avoid potential health issues.
Ultimately, staying informed about diabetic retinopathy symptoms and stages is important for proactive healthcare.
Pre-Proliferative Diabetic Retinopathy
Pre-proliferative retinopathy represents a more advanced stage, building on the changes seen in non-proliferative retinopathy. Significant leakage of fluid and blood into the retina occurs, along with the development of more extensive areas of macular edema. The retina’s blood vessels become more damaged and exhibit some narrowing. The body’s response to this damage can be detected by the formation of abnormal blood vessels.
Proliferative Diabetic Retinopathy
Proliferative retinopathy is a severe stage, marked by the growth of new, fragile blood vessels in the retina. These new blood vessels are often abnormal and prone to leaking blood, which can cause scarring. This new vessel growth can lead to the formation of scar tissue on the retina and detachment. This scar tissue can pull on the retina, potentially causing vision distortion or loss.
Macular Edema
Macular edema is a specific type of swelling that occurs in the macula, the central part of the retina responsible for sharp central vision. Macular edema can develop at any stage of diabetic retinopathy, but it is more common in later stages. The presence of macular edema can significantly impair vision, leading to blurriness, distortion, and difficulty recognizing fine details.
| Stage | Description | Visual Acuity Impact | Treatment Options |
|---|---|---|---|
| Non-proliferative | Early stage with microaneurysms, small hemorrhages, and possible retinal edema. | Usually minimal or no impact on vision. | Regular eye exams, lifestyle modifications (diet, exercise) to manage blood sugar. |
| Pre-proliferative | More advanced stage with increased leakage, blood vessel narrowing, and the development of abnormal blood vessels. | Potential for vision blurring or distortion. | Regular eye exams, blood sugar control, potential laser treatment to reduce leakage. |
| Proliferative | Severe stage with new blood vessel growth, possible scarring, and retinal detachment. | Significant vision loss, including distortion and blurriness, possible blindness. | Laser treatment to reduce abnormal blood vessel growth, potential surgery to repair retinal detachment. |
| Macular Edema | Specific swelling in the macula, the central part of the retina. | Blurred central vision, distortion, difficulty with fine details. | Laser treatment, injections into the eye, and/or other treatments to reduce swelling. |
Risk Factors and Prevention: Diabetic Retinopathy Symptoms And Stages
Diabetic retinopathy, a serious complication of diabetes, can lead to vision loss if left untreated. Understanding the risk factors and implementing preventive measures is crucial for protecting your eye health. Early detection and proactive management play a pivotal role in mitigating the progression of this condition.Controlling blood sugar levels is paramount in preventing and managing diabetic retinopathy. Consistent blood glucose management significantly reduces the risk of developing the condition and slows its progression if it has already begun.
This proactive approach protects the delicate blood vessels in the eyes from damage, ultimately safeguarding vision.
Major Risk Factors
Several factors contribute to the development and progression of diabetic retinopathy. These include prolonged high blood sugar levels, duration of diabetes, and the presence of other related health conditions. The longer someone has diabetes and the less effectively their blood sugar is managed, the higher the risk of developing this eye complication.
- Uncontrolled Blood Sugar: Sustained high blood glucose levels damage the tiny blood vessels in the retina, the light-sensitive tissue lining the back of the eye. This damage is a primary driver of diabetic retinopathy.
- Duration of Diabetes: The longer a person has diabetes, the greater the risk of developing diabetic retinopathy. Years of elevated blood sugar levels progressively damage blood vessels over time.
- High Blood Pressure: Hypertension adds to the strain on the blood vessels, exacerbating the damage caused by high blood sugar and increasing the risk of diabetic retinopathy.
- High Cholesterol: Elevated cholesterol levels can also contribute to the narrowing and hardening of blood vessels, potentially increasing the risk of diabetic retinopathy.
- Pregnancy: Women with diabetes who become pregnant often experience fluctuating blood sugar levels, increasing the risk of developing or worsening diabetic retinopathy during pregnancy.
Role of Blood Glucose Control
Maintaining optimal blood glucose levels is essential in preventing diabetic retinopathy. Consistent control helps prevent damage to the blood vessels in the retina. This proactive approach significantly reduces the risk of developing the condition and its potential complications.
“Strict blood glucose control is the cornerstone of prevention for diabetic retinopathy.”
Tight control of blood sugar levels through medication, diet, and lifestyle modifications is essential in reducing the risk of this serious eye complication. Monitoring and managing blood glucose levels regularly is critical in preventing damage to the blood vessels in the retina.
Importance of Regular Eye Exams
Regular eye exams are critical in detecting diabetic retinopathy early, even before symptoms appear. Early detection allows for timely intervention and treatment, significantly reducing the risk of vision loss. Prompt diagnosis and management strategies can halt or slow the progression of the condition.
- Early Detection: Early detection through regular eye exams allows for prompt intervention and treatment, reducing the risk of vision loss.
- Proactive Management: Regular eye exams enable proactive management of diabetic retinopathy, allowing for the identification and monitoring of changes.
- Improved Outcomes: Prompt diagnosis and management strategies can halt or slow the progression of diabetic retinopathy, resulting in better outcomes for patients.
Lifestyle Choices
Adopting healthy lifestyle choices can significantly minimize the risk of diabetic retinopathy. These choices focus on managing blood sugar levels, promoting overall well-being, and safeguarding eye health.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains can help maintain healthy blood sugar levels.
- Regular Exercise: Regular physical activity improves blood sugar control and promotes overall health.
- Stress Management: Effective stress management techniques can help regulate blood sugar levels.
- Smoking Cessation: Quitting smoking is crucial for reducing the risk of eye complications associated with diabetes.
Risk Factors and Prevention Strategies
| Risk Factor | Description | Prevention Strategies |
|---|---|---|
| Uncontrolled Blood Sugar | Sustained high blood glucose levels damage retinal blood vessels. | Maintain consistent blood sugar levels through medication, diet, and exercise. |
| Duration of Diabetes | Longer duration of diabetes increases risk of damage to blood vessels. | Strict blood glucose control, regular eye exams, and adherence to medical advice. |
| High Blood Pressure | Hypertension increases strain on blood vessels, exacerbating damage. | Control blood pressure through medication and lifestyle changes. |
| High Cholesterol | Elevated cholesterol contributes to blood vessel narrowing. | Maintain healthy cholesterol levels through diet and medication if necessary. |
| Pregnancy (in women with diabetes) | Fluctuating blood sugar levels during pregnancy increase risk. | Close monitoring of blood sugar levels during pregnancy, regular eye exams. |
Diagnosis and Treatment
Discovering diabetic retinopathy early is crucial for preventing vision loss. Accurate diagnosis and timely treatment are key to preserving sight and managing the progression of the disease. The process involves a combination of eye examinations and potential interventions tailored to the specific stage of the disease.
Diagnostic Procedures
Diabetic retinopathy is diagnosed through a comprehensive eye exam. This typically includes a dilated funduscopic examination, where a specialized ophthalmoscope is used to visualize the retina. The ophthalmologist examines the retina for signs of damage, such as microaneurysms, hemorrhages, and neovascularization. The presence and severity of these signs are carefully assessed to determine the stage of the disease.
Additional tests, such as optical coherence tomography (OCT), can provide detailed images of the retina and help in identifying subtle changes. These detailed images can further aid in diagnosis and treatment planning.
Understanding diabetic retinopathy symptoms and stages is crucial for early intervention. Often, subtle symptoms like blurry vision can be a warning sign. Sometimes, these visual changes are accompanied by dry eyes and floaters, which can be a common symptom of other conditions as well, including dry eyes and floaters. Regardless, a thorough eye exam by an ophthalmologist is vital for proper diagnosis and management of diabetic retinopathy.
Treatment Options for Different Stages
The treatment approach for diabetic retinopathy varies depending on the severity and stage of the disease. Early-stage non-proliferative retinopathy often requires careful monitoring, while advanced stages may necessitate more aggressive interventions.
- Early-stage management focuses on meticulous blood sugar control and regular eye examinations. This proactive approach helps slow the progression of the disease. Maintaining healthy blood sugar levels through diet, exercise, and medication is paramount.
- Moderate to severe non-proliferative retinopathy may require laser therapy to seal leaking blood vessels. This procedure, called laser photocoagulation, targets and seals damaged blood vessels preventing further leakage and vision loss.
- Proliferative retinopathy is often treated with laser therapy, as well as vitrectomy. Vitrectomy is a surgical procedure where the vitreous gel in the eye is removed and replaced with a clear solution. This procedure can help reduce the risk of retinal detachment, a potentially sight-threatening complication.
- Macular edema, a swelling in the macula (the central part of the retina), is a serious complication of diabetic retinopathy. Laser therapy and anti-VEGF injections are often used to reduce the swelling and protect vision. Anti-VEGF (vascular endothelial growth factor) injections work by reducing the production of proteins that promote the growth of new blood vessels, which can contribute to macular edema.
The choice of treatment often depends on the severity and response to previous therapies.
Importance of Early Intervention, Diabetic retinopathy symptoms and stages
Early detection and intervention are crucial in managing diabetic retinopathy. The longer the disease progresses without treatment, the greater the risk of vision loss. Early intervention aims to prevent or delay the onset of more severe complications. This approach allows for more effective treatment strategies, reducing the potential for severe visual impairment. Regular eye examinations are essential for early diagnosis and prompt treatment.
Role of Preventative Measures
Maintaining good blood sugar control is the cornerstone of preventing diabetic retinopathy. A healthy lifestyle, including a balanced diet, regular exercise, and adherence to medication regimens, is critical. This approach helps to minimize the risk factors associated with the disease. Individuals with diabetes should undergo regular eye examinations to detect any signs of retinopathy early on, before vision loss becomes a concern.
Treatment Comparison Table
| Treatment | Description | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Laser Therapy | A laser is used to seal leaking blood vessels and reduce abnormal blood vessel growth. | Generally effective in slowing the progression of the disease, particularly in early and moderate stages. | Potential for mild discomfort, temporary vision changes, or rarely, scarring. |
| Vitrectomy | Surgical removal of the vitreous gel in the eye, often followed by replacement with a clear solution. | Effective in managing complications like retinal detachment and severe macular edema, often in advanced stages. | Potential for infection, bleeding, or other surgical complications, and some temporary visual changes. |
Visual Impairment and Quality of Life
Diabetic retinopathy, if left untreated, can lead to significant vision loss, impacting a person’s daily life and overall well-being. Understanding the effects of vision impairment on quality of life and available support resources is crucial for both patients and healthcare professionals. This section delves into the challenges of vision loss and the strategies for coping.Vision loss, a common consequence of diabetic retinopathy, significantly alters a person’s daily activities and social interactions.
It can lead to difficulties with reading, driving, navigating, and performing everyday tasks, which can have a profound impact on a person’s independence and self-esteem. The challenges extend beyond physical limitations, encompassing emotional and psychological well-being.
Impact of Vision Loss on Daily Activities
Vision loss resulting from diabetic retinopathy can disrupt a person’s daily routine and independence. Activities like reading, writing, cooking, and driving become more challenging or impossible. This can lead to feelings of isolation, frustration, and dependence on others. Individuals may need assistance with essential tasks, impacting their sense of self-sufficiency and confidence.
Effects on Quality of Life
The impact of vision loss extends beyond the practical aspects of daily life. It can affect a person’s emotional well-being, social interactions, and overall quality of life. Depression, anxiety, and feelings of isolation are common responses to significant vision loss. Maintaining social connections and pursuing hobbies may become difficult. The reduced ability to participate in activities can lead to feelings of hopelessness and despair.
Recognizing and addressing these emotional challenges is essential for supporting individuals affected by diabetic retinopathy.
Coping Strategies for Vision Loss
Adaptive strategies are crucial for maintaining a good quality of life despite vision loss. These strategies include learning to use assistive technologies, such as screen readers and magnifiers. This could also involve seeking professional guidance for specific tasks. Adjusting home environments and using large print materials, appropriate lighting, and visual cues can make everyday tasks easier. Support groups and counseling services can help individuals cope with the emotional and psychological effects of vision loss.
Learning new ways to interact with the world and adapt to daily life can greatly improve quality of life.
Resources Available for Support
Numerous resources are available to support individuals with diabetic retinopathy and vision loss. These resources offer practical assistance, emotional support, and access to information. Effective communication between patients and healthcare professionals is essential to explore and leverage these resources. Utilizing these resources empowers patients to manage their condition and maintain a positive outlook.
Support Groups and Resources
- Local Eye Care Professionals: Optometrists and ophthalmologists specializing in diabetic eye care can provide comprehensive eye exams, treatment recommendations, and ongoing support. These professionals can also guide patients toward appropriate resources and support groups.
- Diabetic Support Groups: Local and national organizations offer support groups for individuals with diabetes. These groups provide opportunities for shared experiences, emotional support, and information exchange among individuals living with diabetes and its complications.
- National Institutes of Health (NIH): The NIH offers valuable information about diabetic retinopathy, including treatment options, research advancements, and resources for patients. They often provide up-to-date information and connect patients to relevant clinical trials.
- American Diabetes Association (ADA): The ADA provides extensive information on diabetes management, including resources related to diabetic retinopathy. This includes guidelines, educational materials, and support programs for individuals with diabetes and their families.
- Patient Advocacy Organizations: Many patient advocacy organizations focus on specific eye conditions, including diabetic retinopathy. These organizations provide patient support, advocate for policy changes, and offer information on the latest research and treatment advancements.
Closing Notes
In conclusion, diabetic retinopathy symptoms and stages are crucial to understand for those with diabetes. Early detection, proactive management, and a commitment to lifestyle changes are essential for preserving vision and overall well-being. This guide provides a roadmap to navigate the complexities of this eye condition and empowers readers to take control of their health.