Low CSF pressure headache is a condition characterized by a persistent throbbing or aching sensation in the head, often accompanied by other symptoms. Understanding the underlying causes, diagnostic process, and treatment options is crucial for effective management. This comprehensive guide delves into the complexities of low CSF pressure headache, offering insights into its definition, symptoms, potential causes, and treatment strategies.
This article aims to provide a clear and concise explanation of low CSF pressure headache, exploring its various facets, from the underlying physiological mechanisms to practical strategies for prevention and self-care.
Defining Low CSF Pressure Headache
Low cerebrospinal fluid (CSF) pressure headaches are a type of headache characterized by a specific set of symptoms and physiological mechanisms. They are often caused by a leakage of CSF from the brain’s protective membranes, leading to a decrease in the pressure within the skull. Understanding these headaches is crucial for proper diagnosis and effective treatment.
Characteristics of Low CSF Pressure Headache
Low CSF pressure headaches typically present with a unique set of characteristics, making them distinguishable from other types of headaches. The most common symptoms often include a dull, aching pain, and a tendency to worsen with standing. These headaches can vary in intensity, from mild to severe.
Symptoms and Potential Causes of Low CSF Pressure Headache
A variety of symptoms can manifest with low CSF pressure headaches. The specific symptoms experienced by an individual can vary depending on the severity of the leak and the individual’s response.
| Symptom | Description | Potential Causes |
|---|---|---|
| Headache | A persistent, aching pain, often described as a dull, throbbing, or band-like sensation, frequently localized in the back of the head or the top of the head. The pain may worsen when standing upright and improve when lying down. | CSF leakage, often from a dural tear or tear in the meninges. Trauma, prior spinal surgeries, or even spontaneous leaks are also possible causes. |
| Neck pain | Pain in the neck muscles and/or joints, often accompanying or preceding the headache. | May be a result of the head and neck being affected by the reduced pressure, or a result of compensation mechanisms in the body. |
| Visual disturbances | Symptoms such as blurred vision, double vision, or visual field defects. | Can be a result of pressure changes affecting the optic nerve. |
| Vertigo | A sensation of dizziness or spinning, often associated with a loss of balance. | Changes in CSF pressure can affect the inner ear and vestibular system. |
| Tinnitus | A ringing or buzzing sound in the ears, that may be related to the ear structures. | The same physiological mechanisms that affect the inner ear can cause tinnitus. |
| Sensitivity to light and sound | Increased sensitivity to light and sound, often reported as a part of the headache experience. | These are possible symptoms of low CSF pressure headaches, though they are not always present. |
| Meningitis | Inflammation of the membranes surrounding the brain and spinal cord, though this is not the primary cause of low CSF pressure headaches. | This is a possible secondary effect in some cases of CSF leak. |
Physiological Mechanisms
The development of low CSF pressure headaches stems from a decrease in the pressure of cerebrospinal fluid (CSF) within the skull. This decrease is often due to a leak of CSF from the meninges, the protective membranes surrounding the brain and spinal cord. The leak can occur due to various factors such as trauma, prior surgeries, or spontaneous occurrences.
The reduced CSF pressure can lead to the stretching and/or displacement of structures within the brain, leading to pain and other associated symptoms. This explains the worsening of symptoms when standing and improvement when lying down, as gravity influences the CSF distribution.
Symptoms and Diagnosis
Low CSF pressure headaches, while often less severe than other types, can significantly impact daily life. Understanding the specific symptoms and diagnostic process is crucial for accurate identification and appropriate treatment. Accurate diagnosis is key to ensuring the best possible outcome and avoiding misdiagnosis.Identifying the precise cause of a headache, especially one that doesn’t fit typical patterns, requires a careful assessment.
A thorough understanding of the symptoms, coupled with appropriate diagnostic tools, helps distinguish low CSF pressure headaches from other types of headaches, leading to the most effective treatment plan.
Common Symptoms
Low CSF pressure headaches frequently present with a specific set of symptoms that differ from other headache types. These symptoms often include a feeling of the head being loose, as if the head is not firmly attached to the neck. These headaches can also manifest as a dull, aching sensation, sometimes accompanied by a feeling of pressure or fullness around the head.
Low CSF pressure headaches can be a real pain, literally! While I’m no doctor, I’ve been doing some research, and it seems that staying hydrated and focusing on overall well-being can help. One thing I’ve been exploring lately is the potential health benefits of moon milk, a calming beverage said to promote relaxation and better sleep. health benefits moon milk might offer some interesting insights into how it could potentially support general health, which could indirectly help with managing low CSF pressure headaches.
It’s definitely worth considering alongside other treatment options recommended by a healthcare professional, though!
In some cases, the pain might be described as a throbbing sensation. A noticeable feature is the tendency for the pain to worsen when standing upright or performing activities that increase intracranial pressure, such as coughing or straining.
Diagnostic Process, Low csf pressure headache
The diagnostic process for low CSF pressure headaches involves a multifaceted approach, combining medical history, physical examination, and imaging techniques. A detailed clinical history is crucial, as it helps to establish a pattern of symptoms and rule out other potential causes. Questions regarding the onset, frequency, duration, and intensity of headaches, as well as any associated symptoms, are vital.
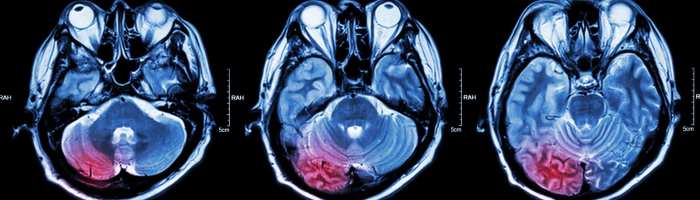
Role of Medical Imaging
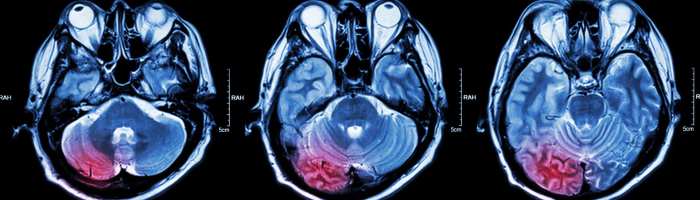
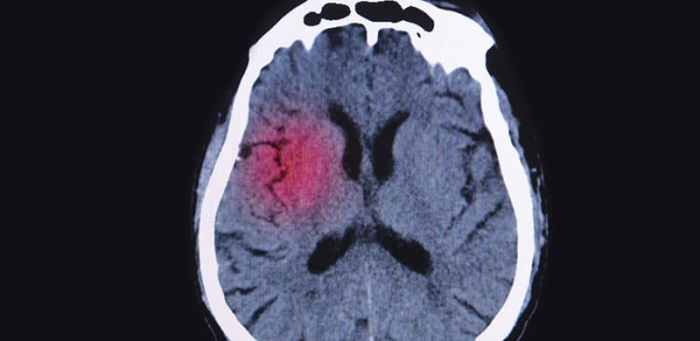
Medical imaging plays a significant role in the diagnostic process. Techniques like MRI (magnetic resonance imaging) and CT scan (computed tomography scan) are used to visualize the brain and spinal cord, looking for any abnormalities that might explain the symptoms. MRI scans provide detailed images of soft tissues, which are particularly useful for evaluating the structures surrounding the brain.
CT scans, on the other hand, offer cross-sectional images, enabling visualization of bone and other hard tissues. The combination of both types of scans provides a comprehensive view of the head and neck region, offering valuable insights into the presence or absence of structural abnormalities.
Clinical History and Physical Examination
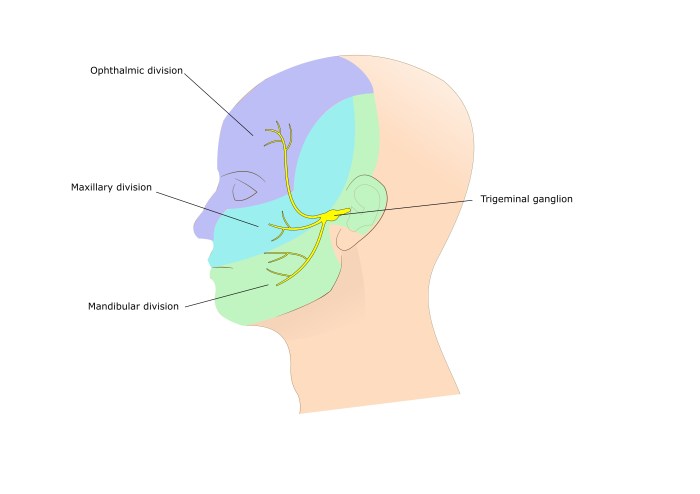
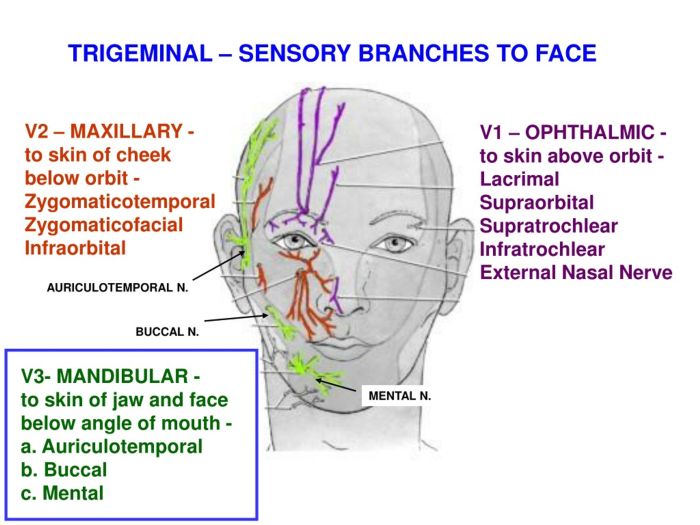
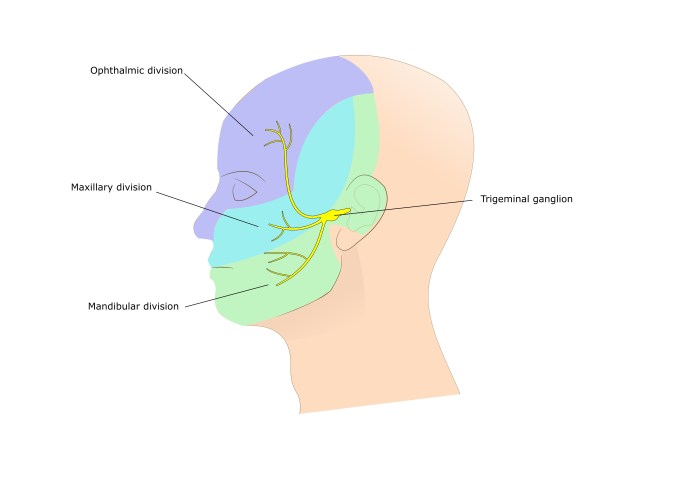
A thorough physical examination is an integral part of the diagnostic process. It includes evaluating the patient’s neurological status, checking for any signs of nerve damage, and assessing for any other underlying conditions. The examination might involve checking reflexes, assessing balance, and evaluating the patient’s cranial nerves. The examiner also assesses posture and movement to look for clues about the patient’s head and neck alignment, and any pain or discomfort during specific movements.
Differential Diagnosis
| Headache Type | Symptoms | Potential Causes |
|---|---|---|
| Low CSF Pressure Headache | Headache worsened by standing, worsened by coughing or straining, dull or aching pain, feeling of head looseness, pressure or fullness | Decreased cerebrospinal fluid (CSF) pressure, trauma, or other medical conditions |
| Tension-Type Headache | Aching, pressing, or tightening pain, often located around the head and neck, mild to moderate intensity | Stress, anxiety, muscle tension, poor posture |
| Migraine | Throbbing or pulsing pain, often on one side of the head, accompanied by nausea, vomiting, and/or sensitivity to light and sound | Genetic predisposition, hormonal changes, stress, environmental factors |
| Cluster Headache | Severe, intense pain, typically on one side of the head, often around the eye or temple, accompanied by tearing, nasal congestion, and/or rhinorrhea | Neurochemical imbalances, environmental triggers |
Causes and Risk Factors

Low CSF pressure headaches, while often perplexing, are frequently linked to underlying medical conditions. Understanding the potential causes and associated risk factors can be crucial for accurate diagnosis and effective management. This section delves into the various factors that contribute to the development of these headaches, considering their potential impact on different demographic groups.
Potential Causes of Low CSF Pressure Headaches
Several medical conditions can lead to a decrease in cerebrospinal fluid (CSF) pressure, resulting in the characteristic symptoms of low CSF pressure headaches. These include:
- Spinal fluid leaks: A rupture or tear in the membranes surrounding the spinal cord or brain can cause CSF to leak out. This can occur due to trauma, surgery, or even spontaneous events. A common example involves a patient experiencing a significant fall or injury, which can lead to such a leak. Another example involves individuals who have undergone spinal procedures, like a lumbar puncture, where a leak can develop.
- Craniospinal fluid fistulas: These abnormal connections between the CSF-filled spaces of the head and the outside of the body can lead to a leakage of CSF. These can occur in various parts of the body, but often affect the areas around the nose or sinuses, or along the spine.
- Meningiomas: These benign tumors can cause pressure changes and lead to CSF leakage. This is often observed in patients who present with a history of a slowly growing tumor.
- Prior spinal or head trauma: Pre-existing spinal or head injuries can sometimes lead to persistent CSF leaks, which can manifest as low CSF pressure headaches.
- Certain medications: Some medications, particularly those that impact blood vessel function, can contribute to the development of low CSF pressure headaches.
- Inadequate Hydration: Dehydration can contribute to low CSF pressure, especially in vulnerable populations.
Prevalence Across Demographic Groups
The prevalence of these causes varies across different demographics, although more research is needed to precisely understand the factors influencing these differences. For instance, certain types of trauma that can cause CSF leaks may be more prevalent in certain age groups. Additionally, factors like the use of specific medications or certain underlying medical conditions might have varying prevalence rates across diverse populations.
More research is needed to determine how the frequency of these causes differs across demographics.
Risk Factors for Low CSF Pressure Headaches
Certain factors increase the risk of developing low CSF pressure headaches. These include:
- Previous spinal or head trauma: Individuals with a history of spinal or head injuries are at a higher risk. This is because these injuries can cause damage to the tissues surrounding the spinal cord and brain, which may lead to CSF leaks.
- Recent surgical procedures involving the spine or head: Surgeries on the spine or head, particularly those involving the lumbar region, can sometimes lead to CSF leaks.
- Certain medical conditions: Underlying medical conditions like tumors can increase the likelihood of CSF leaks and headaches.
- Certain medications: Some medications can potentially increase the risk of CSF leaks.
- Dehydration: Dehydration can weaken the tissues surrounding the CSF-filled spaces, increasing the likelihood of a leak.
Summary Table of Causes and Risk Factors
| Cause | Description | Associated Risk Factors |
|---|---|---|
| Spinal Fluid Leaks | Rupture or tear in membranes surrounding the spinal cord or brain, causing CSF to leak. | Trauma, surgery, spontaneous events, prior spinal or head injuries |
| Craniospinal Fluid Fistulas | Abnormal connections between CSF-filled spaces and the outside of the body. | Various factors affecting areas around the nose, sinuses, or spine |
| Meningiomas | Benign tumors that cause pressure changes, potentially leading to CSF leakage. | Slow tumor growth, history of tumor |
| Prior spinal or head trauma | Pre-existing injuries causing persistent CSF leaks. | Previous injuries, potential for ongoing damage |
| Certain Medications | Specific medications affecting blood vessel function. | Medications impacting blood vessels |
| Inadequate Hydration | Dehydration weakening tissues surrounding CSF spaces. | Dehydration, susceptibility to dehydration |
Treatment and Management
Low CSF pressure headaches, while often manageable, require a tailored approach. Effective treatment hinges on understanding the underlying cause and the individual’s response to various interventions. Successful management frequently involves a combination of lifestyle adjustments, medical interventions, and potentially surgical procedures.Addressing low CSF pressure headaches necessitates a proactive and patient-centric strategy. The focus should be on alleviating symptoms, preventing recurrence, and improving the patient’s overall quality of life.
This involves a comprehensive approach encompassing lifestyle modifications, medical treatments, and, in some cases, surgical options.
Treatment Options Overview
Various strategies are employed to manage low CSF pressure headaches, ranging from simple lifestyle changes to more complex medical and surgical interventions. Understanding the diverse treatment options allows patients and healthcare providers to collaborate in developing a personalized plan.
Lifestyle Modifications
Lifestyle modifications play a crucial role in managing low CSF pressure headaches. These modifications often address contributing factors and help prevent further complications.
- Hydration: Maintaining adequate hydration is essential. Drinking plenty of fluids, especially water, helps to replenish the fluid lost from the leak and supports CSF levels. This can significantly reduce headache frequency and intensity.
- Dietary Changes: Certain dietary factors can influence CSF pressure. A balanced diet that provides essential nutrients may aid in managing symptoms. This might include reducing processed foods, increasing intake of fruits and vegetables, and managing any potential allergies or sensitivities that may exacerbate headaches.
- Stress Management: Chronic stress can worsen headaches. Incorporating stress-reducing techniques, such as meditation, yoga, or deep breathing exercises, can help alleviate symptoms and improve overall well-being.
- Sleep Hygiene: Getting sufficient and consistent sleep is critical. Adequate rest allows the body to repair and replenish, potentially reducing headache triggers.
Medical Interventions
Medical interventions often target symptom relief and support CSF pressure normalization.
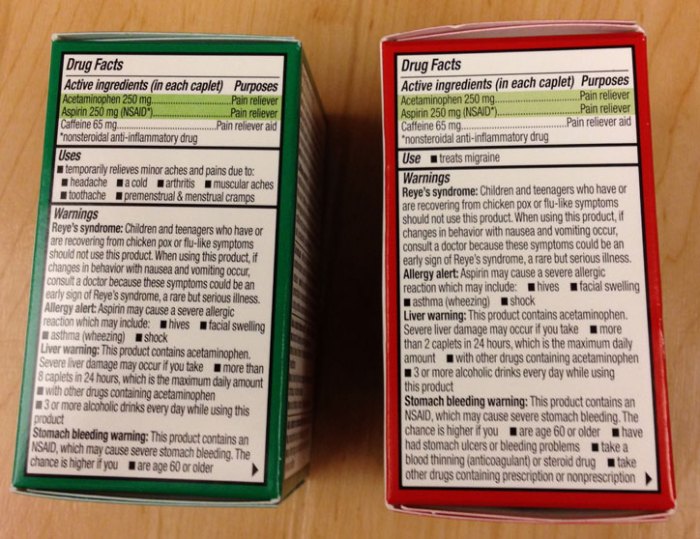
- Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage mild to moderate headaches. Prescription medications, including some muscle relaxants or triptans, might be necessary for severe or persistent symptoms. The choice of medication depends on the severity and frequency of headaches.
- Blood Patch: In cases where a CSF leak is suspected, a blood patch, involving injecting a small amount of the patient’s blood into the area of the leak, can help seal the leak and restore normal CSF pressure. This procedure is generally well-tolerated, with minimal complications.
Surgical Procedures
Surgical interventions are reserved for cases where other treatments are ineffective or when the underlying cause necessitates direct intervention.
Low CSF pressure headaches can be tricky to diagnose, sometimes mimicking other conditions. Understanding cognitive function is key, especially when assessing a patient’s ability to describe symptoms accurately. This is where the Allen Cognitive Level Screen comes in handy, helping healthcare professionals gauge a patient’s level of cognitive function to better understand their overall health status and how they are experiencing the low CSF pressure headache.
Ultimately, a comprehensive approach is needed to diagnose and manage these headaches effectively.
- Repair of CSF Leak: If a CSF leak is identified, surgical repair aims to seal the leak, thereby restoring normal CSF pressure and eliminating the source of headaches. This involves techniques tailored to the specific location and size of the leak. Success rates vary depending on the complexity of the leak.
Treatment Comparison
| Treatment Type | Description | Potential Side Effects |
|---|---|---|
| Lifestyle Modifications | Dietary changes, hydration, stress management, sleep hygiene | Minimal, generally well-tolerated |
| Medications | Over-the-counter and prescription pain relievers, muscle relaxants | Potential for side effects depending on the medication; consult with a physician |
| Blood Patch | Injecting blood into the area of CSF leak | Rare complications, such as infection or bleeding, but generally safe |
| Surgical Repair | Repairing the CSF leak | Potential surgical risks, including infection, bleeding, or nerve damage; recovery time may vary |
Complications and Prognosis: Low Csf Pressure Headache
Low CSF pressure headaches, while often manageable, can sometimes lead to more serious complications if left untreated or if the underlying cause is severe. Understanding these potential complications and the long-term prognosis is crucial for individuals experiencing these headaches and for healthcare providers managing their care. Early diagnosis and appropriate treatment significantly reduce the risk of complications and improve the overall outcome.
Potential Complications
The complications of low CSF pressure headaches vary in severity and depend on the underlying cause and the individual’s response to treatment. Some potential complications include, but are not limited to, worsening headaches, neurological deficits, and spinal fluid leaks.
Low CSF pressure headaches can be a real pain, literally! Understanding the underlying mechanics is key, and sometimes that involves delving into cellular structures. For instance, certain conditions affecting squamous cells can indirectly impact cerebrospinal fluid (CSF) pressure. Learning more about what are squamous cells can help you understand these complex connections. what are squamous cells Ultimately, though, accurate diagnosis and treatment of low CSF pressure headaches require a comprehensive evaluation by a healthcare professional.
- Progressive Neurological Deficits: In some cases, persistent low CSF pressure can lead to progressive neurological deficits, such as vision problems, balance issues, or cognitive impairment. These issues typically manifest as gradual worsening of symptoms over time, and early intervention is key to preventing further deterioration.
- Spinal Fluid Leaks: A significant complication is the development of a spinal fluid leak. This can occur due to the pressure imbalance and may necessitate surgical intervention. Symptoms of a leak can range from worsening headache to visible cerebrospinal fluid leakage from the nose or ears.
- Increased Risk of Secondary Headaches: Chronic low CSF pressure can predispose individuals to developing secondary headaches, which are headaches stemming from an underlying condition. This increased risk highlights the importance of identifying and addressing the root cause of the low CSF pressure.
- Subarachnoid Hemorrhage: While less common, in some cases, low CSF pressure can increase the risk of subarachnoid hemorrhage. This complication arises when blood vessels rupture in the subarachnoid space, a critical area surrounding the brain.
Long-Term Prognosis
The long-term prognosis for individuals with low CSF pressure headaches is generally positive with appropriate treatment. The severity of the prognosis depends on factors such as the underlying cause, the promptness of diagnosis and treatment, and the individual’s overall health. For instance, if the cause is a simple, easily treatable condition, the prognosis is likely excellent with a return to normal function.
Conversely, complications, such as a severe spinal fluid leak, can impact the long-term prognosis.
Importance of Early Diagnosis and Treatment
Early diagnosis and timely intervention are crucial in preventing complications and improving the long-term prognosis. Prompt medical attention allows for the identification and treatment of the underlying cause, reducing the risk of long-term complications and ensuring the best possible outcome. This also includes adherence to prescribed treatments and regular follow-up appointments.
Table of Potential Complications
| Potential Complication | Severity | Preventive Measures |
|---|---|---|
| Progressive Neurological Deficits | Moderate to Severe | Early diagnosis, prompt treatment, adherence to prescribed medication, regular follow-up appointments. |
| Spinal Fluid Leaks | High | Prompt diagnosis, appropriate surgical intervention (if necessary), adherence to post-operative instructions, regular follow-up appointments. |
| Increased Risk of Secondary Headaches | Moderate | Identifying and addressing the root cause of low CSF pressure, proper headache management strategies, regular follow-up appointments. |
| Subarachnoid Hemorrhage | Severe | Early diagnosis, prompt treatment of the underlying cause of low CSF pressure, regular follow-up appointments. |
Prevention and Self-Care Strategies
Managing low CSF pressure headaches often involves a multifaceted approach that goes beyond simply treating symptoms. Proactive strategies play a crucial role in preventing recurrences and improving overall well-being. By incorporating healthy habits and lifestyle adjustments, individuals can significantly reduce their risk of experiencing these debilitating headaches.Effective prevention and self-care involve understanding the underlying causes and risk factors.
By implementing the suggested strategies, individuals can better manage their symptoms and lead healthier lives.
Lifestyle Modifications for Headache Prevention
Maintaining a healthy lifestyle is paramount in reducing the risk of low CSF pressure headaches. A balanced approach that addresses physical health, stress management, and sleep patterns can make a significant difference.
- Hydration: Adequate hydration is essential for overall health and can play a crucial role in preventing headaches. Drinking plenty of water throughout the day helps maintain proper fluid balance within the body, which can contribute to overall well-being and reduce the risk of headaches. Aim for 8 glasses of water daily. Carry a water bottle with you throughout the day to remind yourself to stay hydrated.
- Regular Exercise: Engaging in regular physical activity, such as brisk walking, swimming, or cycling, strengthens the body’s overall health and well-being. Physical activity improves circulation and supports overall health, which can contribute to headache prevention. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Proper Posture: Maintaining good posture is crucial for spinal health and can help prevent headaches, especially those related to postural strain. Practicing good posture throughout the day, whether standing, sitting, or sleeping, can reduce the risk of spinal issues and associated headaches.
- Stress Management Techniques: Chronic stress can exacerbate various health issues, including headaches. Implementing stress management techniques, such as meditation, deep breathing exercises, yoga, or spending time in nature, can help reduce stress levels and mitigate the risk of headaches. Regular practice of these techniques can become a valuable self-care tool.
Dietary Considerations for Headache Prevention
Dietary choices can significantly impact overall health and potentially contribute to headache prevention. Maintaining a balanced diet with adequate nutrients can be a key aspect of headache management.
- Balanced Diet: A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients that support overall health. A well-rounded diet can improve overall health and reduce the risk of developing low CSF pressure headaches. Include a variety of colorful fruits and vegetables in your daily meals.
- Nutrient Deficiencies: Identifying and addressing potential nutrient deficiencies is important. If you suspect a nutrient deficiency, consult a healthcare professional to determine the best course of action. This will help ensure you’re receiving the necessary nutrients to support overall health.
Sleep Hygiene and Headache Prevention
Adequate sleep is essential for physical and mental well-being, and disruptions in sleep patterns can contribute to headaches. Establishing a consistent sleep schedule and creating a conducive sleep environment are crucial for headache prevention.
- Consistent Sleep Schedule: Maintaining a regular sleep-wake cycle helps regulate the body’s natural sleep-wake rhythm, which can contribute to reducing headache frequency. Going to bed and waking up around the same time each day, even on weekends, can improve sleep quality.
- Sleep Environment: Creating a dark, quiet, and cool sleep environment can promote relaxation and improve sleep quality. Minimize distractions and create a comfortable space conducive to restful sleep.
Case Studies and Examples
Understanding low CSF pressure headaches requires looking at real-world cases. These examples demonstrate the spectrum of symptoms, diagnostic challenges, and treatment approaches associated with this condition. Analyzing patient experiences provides valuable insights into managing and preventing these headaches.
A Case Study of a Patient with Low CSF Pressure Headache
A 35-year-old female presented with a progressive headache worsening over several months. Initially, the headaches were mild and intermittent, but gradually increased in frequency and intensity. She described the pain as a dull, throbbing sensation located at the back of her head, often radiating to the neck and shoulders. She also reported experiencing worsening dizziness and balance problems, and visual disturbances.
Neurological examination revealed a positive lumbar puncture result with low CSF pressure. Magnetic Resonance Imaging (MRI) confirmed the diagnosis. The patient responded well to conservative treatment including hydration, bed rest, and pain management with over-the-counter medications.
Progression of Symptoms in a Patient with Low CSF Pressure Headache
The progression of symptoms in a patient with low CSF pressure headache can vary significantly. Some patients experience a gradual onset of symptoms, while others report a sudden and dramatic increase in headache intensity. The headaches may initially be infrequent, mild, and localized, but they can escalate to become severe and debilitating. Associated symptoms like dizziness, balance problems, and visual disturbances often become progressively worse as the condition progresses.
In some cases, the symptoms may remit temporarily before returning with increased severity.
Illustrative Table of Case Study Details
| Case Study Details | Symptoms | Diagnosis | Treatment |
|---|---|---|---|
| Patient: 28-year-old male | Headache worsened over 6 months, worsening dizziness, balance problems. | Lumbar puncture showed low CSF pressure, MRI confirmed. | Conservative treatment including hydration, pain medication, and physical therapy. The patient showed improvement after 3 months of treatment. |
| Patient: 42-year-old female | Sudden onset of severe headache, nausea, vomiting, and visual disturbances. | Lumbar puncture and MRI showed low CSF pressure. | Urgent treatment included hydration, bed rest, and medication for pain and symptoms. Patient required hospitalization and experienced gradual improvement after several days. |
| Patient: 30-year-old female | Gradual onset of mild headache, increased frequency over a year, and neck stiffness. | Lumbar puncture revealed low CSF pressure, confirmed by MRI. | Conservative treatment including hydration, pain management, and avoidance of strenuous activity. The patient experienced minimal symptoms after 4 months. |
Related Conditions and Differentiations
Low CSF pressure headaches can mimic a variety of other headache types, making accurate diagnosis crucial. Differentiating between low CSF pressure headaches and other conditions often requires a thorough evaluation considering symptoms, medical history, and diagnostic tests. Understanding the overlapping symptoms and key differentiating factors is essential for appropriate treatment.
Conditions Mimicking Low CSF Pressure Headaches
Several conditions can present with symptoms similar to low CSF pressure headaches, making accurate diagnosis challenging. These conditions may involve issues with the nervous system, blood vessels, or other body systems. A thorough evaluation by a healthcare professional is essential to rule out these conditions.
- Tension-type headaches: Characterized by a dull, aching pain that can be bilateral (affecting both sides of the head). These headaches often worsen with stress or poor posture, whereas low CSF pressure headaches can be triggered by activities involving the Valsalva maneuver (like straining or coughing).
- Migraines: These often present with throbbing, pulsating pain, typically on one side of the head. They can also be accompanied by nausea, vomiting, and sensitivity to light and sound. Low CSF pressure headaches, while sometimes involving throbbing, are usually not associated with the other migraine symptoms.
- Cluster headaches: These are characterized by severe, stabbing pain, typically around one eye or temple. The pain often occurs in clusters over days or weeks, and is not typically a characteristic of low CSF pressure headaches.
- Post-traumatic headaches: These headaches can arise after a head injury and present with various symptoms, including pain, tenderness, and dizziness. Low CSF pressure headaches, while potentially occurring after head injury, have distinct characteristics.
- Subarachnoid hemorrhage: A condition where blood leaks into the space surrounding the brain. Symptoms can include sudden, severe headaches, stiff neck, and altered mental status. This condition is a serious medical emergency and requires immediate attention.
Differentiating Factors
Accurate differentiation between low CSF pressure headaches and other conditions is crucial for appropriate management. A comprehensive evaluation, including detailed patient history, physical examination, and diagnostic tests, is often necessary.
| Feature | Low CSF Pressure Headache | Tension-type Headache | Migraine | Cluster Headache |
|---|---|---|---|---|
| Pain Location | Often diffuse, occipital (back of head), or frontal | Bilateral, often frontal or temporal | Unilateral (one-sided) or bilateral | Unilateral, around the eye or temple |
| Pain Quality | Dull, aching, or throbbing | Dull, aching, pressing | Throbbing, pulsating | Severe, stabbing |
| Associated Symptoms | Visual disturbances, dizziness, neck pain, tinnitus | Muscle tension, fatigue, stress | Nausea, vomiting, photophobia, phonophobia | Lacrimation (tearing), rhinorrhea (runny nose) |
| Triggering Factors | Valsalva maneuver, straining, prolonged standing, rapid position changes | Stress, anxiety, fatigue, caffeine withdrawal | Stress, caffeine, certain foods, hormonal changes | Alcohol, stress, changes in sleep patterns |
| Severity | Can range from mild to severe | Mild to moderate | Moderate to severe | Severe |
Overlapping Symptoms
Some symptoms may overlap between low CSF pressure headaches and other conditions. For example, both low CSF pressure headaches and migraines can present with throbbing pain. However, the accompanying symptoms, triggering factors, and diagnostic findings can help distinguish between these conditions.
Illustrative Images and Diagrams
Understanding low CSF pressure headaches often requires visualizing the affected anatomy and potential imaging findings. Visual aids can significantly enhance comprehension and facilitate better communication between patients and healthcare providers. These tools can help patients grasp the underlying mechanisms of the condition and the rationale behind diagnostic and therapeutic approaches.
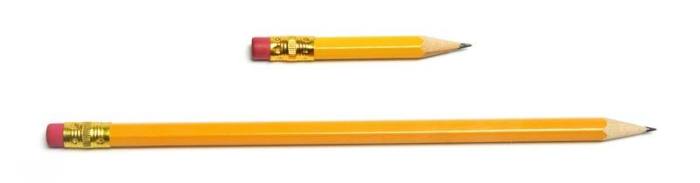
Cerebrospinal Fluid System Anatomy
The cerebrospinal fluid (CSF) system is a complex network within the brain and spinal cord. A diagram illustrating this system would show the ventricles of the brain, the subarachnoid space surrounding the brain and spinal cord, and the pathways for CSF flow. Crucially, the diagram would highlight the location of the subarachnoid space, where CSF pressure is measured.
The diagram would clearly label the different structures involved, including the arachnoid mater, pia mater, and the ventricles. It would also show the connection between the ventricles and the subarachnoid space. The specific area where the pressure is measured would be distinctly marked.
Low CSF Pressure Headache on Imaging Scan
Medical imaging plays a vital role in diagnosing low CSF pressure headaches. A typical imaging scan, like a CT scan or MRI, showing this condition would reveal a flattened appearance of the brain’s base and/or the spinal cord. The subarachnoid space might appear markedly widened, and the brain might appear to be shifted upward or downward relative to its normal position.
The absence of the normal amount of CSF in the subarachnoid space would be a key feature, often accompanied by a loss of the normal CSF cushion. The specific appearance of these findings would vary depending on the severity of the condition.
Treatment Options Visual Representation
Visualizing treatment options for low CSF pressure headaches can be beneficial. A graphic could depict a flowchart outlining the different phases of treatment. This would include options like blood patch procedures, where a small amount of the patient’s own blood is injected into the leak site to seal it. Other possible options include the use of oral medications to help manage symptoms.
The flowchart could also illustrate the importance of monitoring and follow-up care. This approach is designed to give a clear overview of the treatment options available, from initial diagnosis to ongoing management.
Summary Table of Medical Images
This table summarizes the various medical imaging modalities associated with low CSF pressure headaches, highlighting key findings for each.
| Imaging Modality | Key Findings |
|---|---|
| Computed Tomography (CT) Scan | Flattened brain base, widened subarachnoid space, possible displacement of brain structures. |
| Magnetic Resonance Imaging (MRI) | Similar findings to CT scan, often with more detailed visualization of the brain structures and subarachnoid space, providing further details on the condition. |
| Lumbar Puncture (LP) | Low opening pressure in the subarachnoid space is a key diagnostic finding. |
Last Point
In conclusion, low CSF pressure headache, while potentially debilitating, is manageable with appropriate medical attention and lifestyle adjustments. Early diagnosis and treatment are key to preventing complications and improving long-term prognosis. Remember, this information is for educational purposes only and should not be considered medical advice. Consult a healthcare professional for any health concerns.