Ask an expert will losing weight lower my heart disease risk? This question delves into the complex relationship between shedding pounds and reducing cardiovascular risk. We’ll explore the science behind weight loss’s impact on heart health, examining the physiological mechanisms, diverse weight loss methods, and crucial lifestyle factors. Understanding the nuances of this connection is key to making informed decisions about your well-being.
The discussion will encompass various aspects, from the fundamental correlation between weight and heart disease to the specific considerations for different demographics. We’ll also cover the importance of consulting healthcare professionals, managing underlying medical conditions, and adopting sustainable weight management strategies for long-term heart health.
Understanding Weight Loss and Heart Disease Risk

Losing weight can significantly reduce your risk of heart disease. This is not just about aesthetics; it’s about improving your overall cardiovascular health and potentially extending your lifespan. A healthy weight contributes to a healthier heart, reducing strain on the entire system. This section delves into the crucial connection between weight loss and heart disease prevention, exploring the mechanisms involved and the various weight loss strategies.Weight loss, when achieved through healthy lifestyle modifications, can positively impact various physiological mechanisms that contribute to a reduced risk of heart disease.
This includes improving blood pressure, cholesterol levels, and blood sugar control. These improvements create a healthier environment for the heart to function effectively, minimizing the risk of developing cardiovascular issues.
Correlation Between Weight Loss and Reduced Heart Disease Risk
Weight loss, particularly when focused on visceral fat (the fat surrounding organs), directly correlates with a reduction in cardiovascular risk factors. Visceral fat is metabolically active and releases substances that can damage blood vessels and promote inflammation, which are key factors in the development of heart disease. Losing weight helps to decrease the production of these harmful substances, resulting in a more favorable cardiovascular environment.
Physiological Mechanisms of Weight Loss Impacting Cardiovascular Health
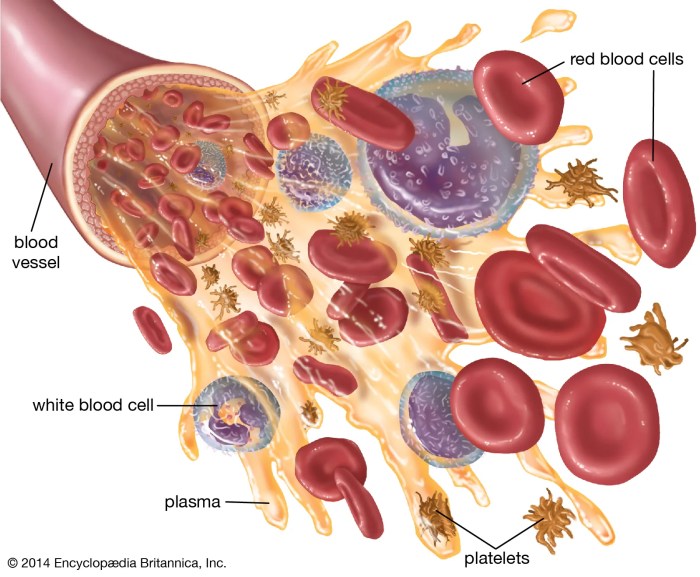
Weight loss improves various physiological parameters vital to cardiovascular health. Reduced weight leads to lower blood pressure, as the heart doesn’t have to work as hard to pump blood throughout the body. Improved insulin sensitivity, often a consequence of weight loss, helps regulate blood sugar levels, further decreasing cardiovascular stress. Simultaneously, weight loss can positively influence cholesterol levels, lowering LDL (“bad”) cholesterol and raising HDL (“good”) cholesterol.
These combined improvements create a protective effect against the development of atherosclerosis (plaque buildup in arteries).
Role of Excess Weight in Increasing Heart Disease Risk
Excess weight, particularly abdominal obesity, increases the risk of heart disease through multiple pathways. The increased strain on the heart to pump blood against higher resistance in the vessels, elevated blood pressure, and the production of inflammatory substances by visceral fat are all contributing factors. Furthermore, excess weight is often associated with other conditions like type 2 diabetes and high cholesterol, all of which are significant risk factors for heart disease.
Types of Heart Disease and Their Risk Factors
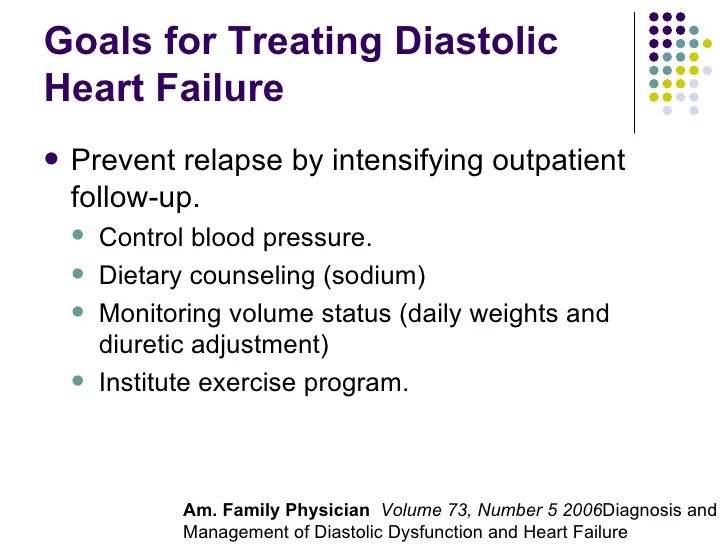
Heart disease encompasses a range of conditions, including coronary artery disease (CAD), heart failure, and arrhythmias. CAD, characterized by the buildup of plaque in the coronary arteries, is a leading cause of heart attacks. Heart failure occurs when the heart cannot pump enough blood to meet the body’s needs. Arrhythmias involve irregular heartbeats, which can lead to various complications.
Common risk factors for these conditions include high blood pressure, high cholesterol, smoking, diabetes, and a sedentary lifestyle. Obesity is a significant risk factor for all types of heart disease.
Weight Loss Methods and Their Potential Impact on Heart Health
Various weight loss methods exist, each with different potential impacts on heart health. A balanced approach, combining dietary changes and regular exercise, is often the most effective strategy for sustainable weight loss and improved cardiovascular health. Diets emphasizing whole foods, fruits, vegetables, and lean protein, along with regular physical activity, promote gradual and healthy weight loss.
Comparison of Weight Loss Strategies
| Weight Loss Method | Potential Impact on Heart Health | Effectiveness Rating |
|---|---|---|
| Balanced Diet and Exercise | Significant improvements in blood pressure, cholesterol, and insulin sensitivity. | High |
| Low-Carb Diets | Potential for improved blood sugar and cholesterol levels, but potential for negative long-term effects if not balanced. | Moderate |
| Very Low-Calorie Diets | Rapid weight loss, but may have adverse effects on metabolism and cardiovascular health if not medically supervised. | Low |
| Surgical Procedures | Significant weight loss, potentially leading to substantial improvements in cardiovascular risk factors. | High (but with risks) |
Factors Influencing Weight Loss and Heart Health Outcomes
Losing weight can significantly reduce your risk of heart disease, but the journey is multifaceted. It’s not just about the number on the scale; it’s about adopting a holistic approach that considers various lifestyle factors. This involves understanding the complex interplay between diet, exercise, stress, sleep, and specific weight loss programs. This exploration will delve into these crucial components.The path to a healthier heart often involves a profound shift in lifestyle choices.
Effective weight management isn’t a quick fix; it’s a continuous process of learning, adapting, and consistently making positive changes. Success hinges on understanding the factors that influence both weight loss and heart health. These factors are interconnected and work together to either support or hinder your progress.
The Role of Diet in Weight Loss and Cardiovascular Health
A balanced diet is fundamental to both weight loss and heart health. Focus on whole, unprocessed foods like fruits, vegetables, lean proteins, and whole grains. These foods are rich in essential nutrients, fiber, and antioxidants, which support overall health and aid in weight management. Limit processed foods, sugary drinks, and excessive saturated and trans fats. These dietary choices can negatively impact both weight and heart health.
A registered dietitian can provide personalized dietary guidance.
Importance of Regular Physical Activity
Regular physical activity is crucial for achieving and maintaining a healthy weight. Physical activity boosts metabolism, burns calories, and strengthens the cardiovascular system. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days a week. Find activities you enjoy to sustain motivation.
Consider incorporating activities like brisk walking, swimming, cycling, or dancing.
Stress and Weight Management
Chronic stress can significantly impact weight management and heart health. Stress hormones can lead to increased appetite and cravings for unhealthy foods, potentially hindering weight loss efforts. Moreover, stress can negatively impact sleep quality, further complicating the equation. Stress management techniques, such as mindfulness, meditation, yoga, or deep breathing exercises, can help mitigate these effects. Seeking professional support for stress management can be beneficial.
Sleep Quality and Duration
Adequate sleep is essential for overall health, including weight management and cardiovascular health. Lack of sleep can disrupt hormones that regulate appetite, leading to increased hunger and cravings for high-calorie foods. Poor sleep quality can also increase inflammation in the body, which is linked to heart disease. Aim for 7-9 hours of quality sleep per night. Establish a regular sleep schedule and create a relaxing bedtime routine.
Effectiveness of Different Weight Loss Programs
Various weight loss programs exist, each with its approach and effectiveness. Some programs emphasize diet, others focus on exercise, and some combine both. The most successful programs often incorporate lifestyle changes and provide ongoing support. Consulting with a healthcare professional or registered dietitian is crucial in selecting a program that aligns with your needs and health status.
So, you’re wondering if shedding those extra pounds will help your heart health? A great question for an expert! While weight loss definitely plays a crucial role in reducing heart disease risk, it’s also important to consider other factors. For example, muscle and joint pain can be a symptom of underlying issues like thyroid disease, which can significantly impact your overall well-being and potentially complicate weight loss efforts.
If you’re experiencing this, be sure to check out this helpful resource on muscle and joint pain with thyroid disease. Ultimately, consulting a healthcare professional is key to understanding the best approach for your individual situation, whether it’s weight loss or managing other health concerns.
Comparison of Weight Loss Programs
| Lifestyle Modification | Potential Benefits for Heart Health | Implementation Tips |
|---|---|---|
| Balanced Diet | Reduced risk of high blood pressure, high cholesterol, and type 2 diabetes. | Focus on fruits, vegetables, lean proteins, and whole grains. Limit processed foods, sugary drinks, and unhealthy fats. |
| Regular Exercise | Improved cardiovascular fitness, reduced blood pressure, and increased HDL (“good”) cholesterol. | Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week. Include muscle-strengthening activities. |
| Stress Management | Reduced stress hormones, improved sleep quality, and potential weight management support. | Practice mindfulness, meditation, yoga, or deep breathing exercises. Seek professional support if needed. |
| Adequate Sleep | Improved hormone regulation, reduced inflammation, and better overall health. | Aim for 7-9 hours of quality sleep per night. Establish a regular sleep schedule and create a relaxing bedtime routine. |
| Support System | Increased motivation, accountability, and sustained lifestyle changes. | Seek support from family, friends, or support groups. Consider professional guidance from a healthcare provider or registered dietitian. |
Specific Populations and Weight Loss
Weight loss for heart health isn’t a one-size-fits-all approach. Different demographics face unique challenges and opportunities when it comes to shedding pounds and improving cardiovascular well-being. Understanding these variations is crucial for developing effective and sustainable strategies that cater to specific needs and circumstances. Personalized plans are vital for achieving positive outcomes.Effective weight management programs for various groups require careful consideration of individual needs and potential obstacles.
Strategies must be tailored to address cultural, socioeconomic, and lifestyle factors. This personalized approach recognizes that genetic predispositions and existing health conditions can influence the effectiveness of certain weight loss methods. Acknowledging these factors ensures programs are supportive and promote long-term success.
Weight Loss in Men
Men often face different physiological and lifestyle factors compared to women when it comes to weight management. Metabolic differences can lead to varying responses to diet and exercise. Addressing these disparities in weight loss programs is essential for achieving optimal outcomes. Male-specific programs often emphasize strength training and targeted exercise regimes.
Weight Loss in Women
Women experience hormonal fluctuations that can impact metabolism and weight regulation. These hormonal changes can make weight loss more challenging and require adjustments in dietary and exercise approaches. Women’s programs often focus on mindful eating and stress management, along with strategies to address potential hormonal imbalances.
Weight Loss in Older Adults
Age-related changes in metabolism and muscle mass can affect weight loss effectiveness. Older adults may also have underlying health conditions that influence dietary choices and exercise capacity. Weight loss programs for this demographic need to prioritize safety, gradual progression, and consideration of any existing health issues. These programs often focus on functional fitness and balanced nutrition.
Weight Loss in Children
Childhood obesity is a growing concern, and weight loss strategies must be approached with extreme caution. Programs should focus on lifestyle changes rather than rapid weight loss. Encouraging healthy habits, such as balanced nutrition and regular physical activity, is paramount in supporting a child’s overall health and development. Parental involvement and support are crucial components of successful childhood weight management.
The Role of Genetics in Weight Loss
Genetic predispositions can influence an individual’s propensity to gain or lose weight. Some people may have a higher predisposition to certain dietary patterns, making it more challenging to lose weight. While genetics play a role, lifestyle factors and environmental influences significantly impact weight loss outcomes. Recognizing genetic predispositions can inform personalized strategies, optimizing the effectiveness of weight loss programs.
So, you’re wondering if losing weight will lower your heart disease risk? A great question! While shedding pounds definitely has numerous health benefits, it’s also important to consider other factors like managing stress and getting regular exercise. Learning how to treat an itchy scalp can also be beneficial for overall well-being. Many people find relief with remedies like using a gentle shampoo and avoiding harsh products.
This article delves into the different approaches to managing an itchy scalp. Ultimately, if you’re concerned about your heart health, consulting a doctor is always the best first step in understanding your individual risk factors and how weight loss can play a role.
Potential Challenges for Weight Loss in Specific Populations
Weight loss challenges vary across demographic groups. For example, socioeconomic factors can limit access to healthy foods and safe exercise environments. Cultural norms and dietary traditions may present additional obstacles. Recognizing and addressing these specific challenges is essential for creating inclusive and effective weight loss programs.
Examples of Successful Weight Loss Programs
Various successful programs cater to diverse populations. Programs like the Mediterranean Diet have proven effective in weight management, particularly for older adults and individuals with heart conditions. Others may use personalized meal plans, exercise programs, and lifestyle coaching tailored to specific needs. Effective programs emphasize sustainability and long-term adherence.
Table of Potential Differences in Weight Loss Responses
| Population Group | Weight Loss Strategies | Potential Challenges |
|---|---|---|
| Men | Strength training, targeted exercise regimes | Metabolic differences, lifestyle factors |
| Women | Mindful eating, stress management, addressing hormonal imbalances | Hormonal fluctuations, lifestyle factors |
| Older Adults | Functional fitness, balanced nutrition, gradual progression | Age-related changes, underlying health conditions |
| Children | Lifestyle changes, balanced nutrition, regular physical activity, parental involvement | Cultural norms, access to healthy foods, safety concerns |
Medical Considerations and Weight Loss: Ask An Expert Will Losing Weight Lower My Heart Disease Risk

Before embarking on any weight loss journey, it’s crucial to understand the potential interplay between your health conditions and your approach. A personalized plan, developed in consultation with a healthcare professional, is essential for a safe and effective weight loss strategy. This is particularly important if you have underlying medical conditions that can affect your metabolism, nutrient absorption, or response to different weight loss methods.
I’ve been getting a lot of questions lately about whether losing weight will lower your heart disease risk. It’s a complex issue, and while shedding pounds definitely has a positive impact on overall health, the specifics depend on individual circumstances. For example, if you have a tooth cracked in half but aren’t experiencing pain, it’s crucial to see a dentist immediately as a cracked tooth can lead to serious issues.
This can sometimes be overlooked. Still, asking an expert about the specific impact of weight loss on heart disease risk is always a good idea. The link tooth cracked in half no pain is a good starting point for further research, and remember, a healthy lifestyle is key for a healthy heart!
Importance of Professional Consultation
Consulting a healthcare professional, such as a doctor or registered dietitian, is paramount before starting any weight loss program. They can assess your overall health, identify any underlying medical conditions, and tailor a plan that aligns with your individual needs and health goals. This personalized approach minimizes potential risks and maximizes the chances of success.
Medical Conditions and Weight Management
Certain medical conditions can significantly impact weight management and heart health. For example, diabetes, hypothyroidism, and other hormonal imbalances can affect metabolism and make weight loss more challenging. A healthcare professional can identify these conditions and develop strategies to manage them alongside your weight loss goals.
Medications and Weight Loss
Some medications can influence weight. Certain medications for conditions like depression, anxiety, or high blood pressure might have side effects that include changes in appetite or metabolism. A healthcare provider can evaluate the potential impact of any medications you are taking on your weight loss journey and help you adjust your strategy as needed. They can also recommend alternative medications or adjustments to your dosage if necessary.
Risks of Rapid Weight Loss
Rapid weight loss can be detrimental to your health. It can lead to nutrient deficiencies, muscle loss, and even electrolyte imbalances. A gradual and sustainable approach, guided by a healthcare professional, is crucial to prevent these potential complications. It’s important to prioritize a balanced approach over quick fixes. For example, extremely restrictive diets can lead to nutrient deficiencies and can be harmful.
Tailoring Weight Loss Strategies to Individual Needs
Weight loss strategies should be tailored to individual medical needs. A person with diabetes, for instance, may need a different approach compared to someone with no underlying health conditions. A healthcare professional can determine the most suitable dietary plan, exercise regimen, and overall lifestyle adjustments to meet specific medical needs.
Potential Medication-Weight Loss Interactions
| Medication | Potential Impact on Weight Loss | Considerations |
|---|---|---|
| Antidepressants (some types) | May increase appetite or affect metabolism | Consult your doctor about potential alternatives or adjustments to your dosage. |
| Steroids | Often lead to weight gain | Discuss with your doctor strategies to mitigate weight gain while managing your condition. |
| Diabetes medications | May affect appetite and metabolism | Your doctor can adjust your medication or recommend additional lifestyle changes. |
| Thyroid medications | May influence metabolism and appetite | Adjusting medication doses or dietary changes may be necessary. |
| Blood pressure medications | Some may lead to fluid retention or appetite changes | Consult your doctor for alternative options if necessary. |
Long-Term Maintenance and Weight Management
Staying at a healthy weight isn’t a sprint; it’s a marathon. Successfully shedding pounds is a significant achievement, but the real challenge lies in maintaining those results for the long haul. This requires a shift in mindset, from a temporary diet to a lifelong commitment to healthy habits. This section will explore the crucial elements of long-term weight management, empowering you to make sustainable choices for your heart health.
Sustainable Weight Loss Strategies for Long-Term Heart Health, Ask an expert will losing weight lower my heart disease risk
Maintaining a healthy weight is not about restricting yourself but about making conscious, sustainable lifestyle changes. These changes are more likely to be successful and lead to long-term heart health when approached as an integrated lifestyle rather than a temporary diet. This encompasses a balanced approach that incorporates all facets of your life, from food choices to physical activity and stress management.
Developing Healthy Habits for Weight Maintenance
Developing sustainable habits is crucial for weight maintenance. It’s not about perfection, but about consistency. Focus on these key areas:
- Balanced Diet: Prioritize whole, unprocessed foods like fruits, vegetables, lean proteins, and whole grains. Limit processed foods, sugary drinks, and excessive saturated and unhealthy fats. Pay attention to portion sizes to avoid overeating, even with healthy foods. A registered dietitian can offer personalized dietary guidance.
- Regular Physical Activity: Incorporate physical activity into your daily routine. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities twice a week. Find activities you enjoy, whether it’s dancing, hiking, swimming, or team sports. Consistency is key, not just intensity.
- Stress Management Techniques: Chronic stress can lead to unhealthy coping mechanisms, such as emotional eating. Incorporate stress-reducing activities such as meditation, yoga, deep breathing exercises, or spending time in nature. Stress management is crucial for maintaining a healthy weight and overall well-being.
The Role of Support Systems in Weight Management
Weight management is often more successful when you have a supportive network. This could include family members, friends, support groups, or healthcare professionals.
- Accountability Partners: Sharing your goals with a friend or family member can provide accountability and motivation. Regular check-ins and shared celebrations of progress can significantly boost your commitment.
- Support Groups: Connecting with others facing similar challenges can offer encouragement, shared experiences, and coping strategies. Online or in-person support groups can provide a valuable network of peers.
- Healthcare Professionals: Consult your doctor or a registered dietitian for personalized advice and support. They can assess your individual needs and provide tailored recommendations for sustainable weight management.
Preventing Weight Regain After Achieving Goals
Maintaining weight loss requires ongoing effort. Strategies to prevent regain include:
- Consistency: Don’t fall into the trap of “all or nothing.” Consistency in your healthy habits is more effective than occasional extreme measures. Maintain a consistent approach to eating and exercise, adjusting as needed.
- Addressing Plateaus: Weight loss plateaus are common. Consult your doctor or a registered dietitian to identify potential underlying causes and adjust your plan. Review your current habits and see where adjustments are needed.
- Long-Term Mindset Shift: Focus on adopting a healthy lifestyle rather than a temporary diet. Weight management is a journey, not a destination. Focus on adopting long-term, sustainable habits.
Potential Challenges and Solutions for Long-Term Weight Management
Maintaining a healthy weight is a lifelong commitment, not a quick fix. Some common challenges include:
- Social Gatherings and Temptations: Learn strategies for managing social situations and temptation. Prepare healthy options in advance or choose smaller portions of tempting foods. Focus on moderation rather than deprivation.
- Lifestyle Changes and Time Constraints: Make small, manageable changes to fit your lifestyle. Prioritize your well-being by incorporating healthy choices into your daily routine. Be realistic about your time and resources.
- Emotional Eating: Develop coping mechanisms for emotional eating. Engage in stress-reducing activities or talk to a therapist to address underlying issues.
Tools and Resources for Weight Management Support
Numerous tools and resources are available to support your weight management journey.
- Apps: Many apps offer personalized meal planning, exercise tracking, and support communities.
- Online Communities: Online forums and social media groups can provide support and motivation from like-minded individuals.
- Registered Dietitians: Registered dietitians can provide personalized nutrition plans and support.
Final Wrap-Up
Ultimately, the answer to “ask an expert will losing weight lower my heart disease risk” is a resounding yes, but not without careful consideration. Weight loss, when approached responsibly and sustainably, can significantly reduce heart disease risk. However, it’s vital to tailor your approach to individual needs, seek professional guidance, and prioritize long-term lifestyle changes for optimal results.
By understanding the complexities of weight loss and heart health, you can empower yourself to make informed choices and take proactive steps toward a healthier future.