Foods high in omega 3 are essential for a healthy lifestyle. They play a crucial role in maintaining heart health, brain function, and overall well-being. This comprehensive guide explores the different types of omega-3 fatty acids, their sources, benefits, and potential risks. We’ll delve into diverse food sources, from seafood to plant-based options, and examine preparation methods to maximize omega-3 intake.
Understanding the varied types of omega-3s, like EPA, DHA, and ALA, is key to appreciating their unique roles in your body. We’ll uncover the science behind their benefits, from reducing inflammation to boosting cognitive function. This guide provides practical information and insights to help you incorporate omega-3 rich foods into your daily diet, emphasizing the importance of a balanced approach.
Types of Omega-3 Fatty Acids: Foods High In Omega 3
Omega-3 fatty acids are essential polyunsaturated fats that play crucial roles in various bodily functions, including brain health, heart health, and reducing inflammation. Understanding the different types of omega-3s and their unique characteristics is key to maximizing their potential benefits. These fats are not produced by the body and must be obtained through diet.Different types of omega-3s exhibit varying degrees of bioavailability and impact on health.
This section delves into the specific types, their sources, and the nuances of their influence on well-being.
Types of Omega-3 Fatty Acids
Omega-3 fatty acids are categorized into three main types: EPA (eicosapentaenoic acid), DHA (docosahexaenoic acid), and ALA (alpha-linolenic acid). Each type has distinct characteristics and plays a unique role in the body.
EPA (Eicosapentaenoic Acid)
EPA is a longer-chain omega-3 fatty acid that is primarily found in fatty fish. It plays a critical role in reducing inflammation and blood clotting. Its impact on cardiovascular health has been extensively studied. EPA is also believed to support brain function and mental well-being.
- Primary Food Sources: Fatty fish such as salmon, mackerel, tuna, and sardines are excellent sources of EPA.
- Bioavailability and Health Benefits: EPA is more readily absorbed by the body than ALA. Studies suggest that EPA contributes to lowering triglycerides, improving blood pressure, and reducing the risk of heart disease.
- Potential Risks: Consuming excessive amounts of fish, especially those with high mercury content, can pose a risk. Consult with a healthcare professional to determine appropriate intake levels.
DHA (Docosahexaenoic Acid)
DHA is another longer-chain omega-3 fatty acid, primarily found in fatty fish. It’s crucial for brain development and function, particularly during fetal development and childhood. DHA is also essential for eye health and may contribute to cognitive function throughout life.
- Primary Food Sources: Fatty fish, such as salmon, tuna, mackerel, and herring, are excellent sources of DHA. Some algae-based supplements also provide DHA.
- Bioavailability and Health Benefits: Similar to EPA, DHA is readily absorbed and exhibits potent anti-inflammatory properties. Studies indicate that adequate DHA intake may contribute to improved brain function, cognitive performance, and reduced risk of age-related cognitive decline.
- Potential Risks: Excessive intake of certain fish may expose individuals to potentially harmful levels of mercury. Consult a healthcare professional to establish appropriate intake levels.
ALA (Alpha-Linolenic Acid)
ALA is a shorter-chain omega-3 fatty acid found primarily in plant-based foods. While the body can convert ALA into EPA and DHA, this conversion is inefficient.
- Primary Food Sources: Flaxseeds, chia seeds, walnuts, and hemp seeds are rich in ALA.
- Bioavailability and Health Benefits: ALA contributes to reducing inflammation and may offer some cardiovascular benefits. However, its conversion to EPA and DHA is limited, so it does not provide the same level of benefits as EPA and DHA.
- Potential Risks: ALA is generally considered safe, but large quantities may not be effectively converted to EPA and DHA. Focusing on food sources rich in EPA and DHA might be more effective.
Comparison of Omega-3 Types
| Type | Primary Food Sources | Bioavailability | Potential Health Benefits | Potential Risks |
|---|---|---|---|---|
| EPA | Fatty fish (salmon, mackerel, tuna) | High | Lowering triglycerides, improving blood pressure, reducing heart disease risk | Mercury exposure from fish |
| DHA | Fatty fish (salmon, tuna, mackerel), algae | High | Improved brain function, cognitive performance, eye health | Mercury exposure from fish |
| ALA | Flaxseeds, chia seeds, walnuts, hemp seeds | Low (conversion to EPA/DHA) | Reducing inflammation, some cardiovascular benefits | Limited conversion to EPA/DHA |
Food Sources Rich in Omega-3s
Embarking on a journey to incorporate omega-3 fatty acids into your diet is a fantastic choice for overall health and well-being. These essential fats play a crucial role in various bodily functions, from brain development to heart health. Understanding where to find these vital nutrients is key to optimizing your intake.Knowing which foods are packed with omega-3s allows you to strategically plan your meals and snacks, ensuring you’re getting the necessary dose for optimal health.
This exploration dives into diverse food sources and highlights preparation techniques to maximize omega-3 retention.
Seafood Powerhouses
Seafood is a rich source of omega-3 fatty acids, particularly EPA and DHA. These types are particularly beneficial for heart health and brain function. The specific types of fish and shellfish vary in their omega-3 content. Careful selection and preparation methods can ensure you reap the maximum benefits.
- Fatty fish, like salmon, mackerel, tuna, and sardines, are excellent sources of omega-3s. Their rich, oily texture is a testament to their high content. These fish offer a delightful blend of flavor and nutrition.
- Herring and anchovies are also great choices, providing a substantial dose of omega-3s in a compact package. They are often a part of traditional cuisines and offer a versatile ingredient.
- Shellfish like oysters and shrimp also contain omega-3s, albeit in smaller amounts compared to fatty fish. They contribute to a balanced intake and provide various essential nutrients.
Plant-Based Options
While seafood is a prime source, plant-based foods also contribute to a balanced omega-3 intake. These sources often provide ALA, which the body converts to EPA and DHA, although this conversion is not always efficient.
- Flaxseeds and flaxseed oil are renowned for their high ALA content. They can be incorporated into smoothies, sprinkled on cereals, or used as a topping for yogurt. However, the conversion efficiency of ALA to EPA and DHA is relatively low in the human body.
- Chia seeds are another excellent source of ALA. They are incredibly versatile, adding a delightful texture and nutritional punch to various dishes.
- Walnuts and walnuts oil provide a significant amount of ALA. Their crunchy texture and nutty flavor make them a delicious and nutritious addition to salads, yogurt, or as a snack.
- Hemp seeds are a great source of omega-3s and other essential nutrients, making them a versatile addition to meals.
Preserving Omega-3 Content
Proper preparation methods can significantly impact the omega-3 content of foods. Cooking methods that minimize heat exposure are often preferable.
- Baking, grilling, or steaming are gentler cooking methods that can help retain omega-3s.
- Avoid deep-frying, as high heat can degrade the omega-3s. The high heat exposure can lead to the breakdown of the delicate fatty acid structure.
- When preparing seafood, consider pan-searing or stir-frying at moderate temperatures. These methods balance flavor with preservation of nutrients.
Omega-3 Content Comparison, Foods high in omega 3
| Food Source | Serving Size (approx.) | Approximate Omega-3 Content (mg) |
|---|---|---|
| Salmon (cooked) | 3 oz | 1500-2000 |
| Flaxseeds (1 tbsp) | 1 tbsp | 2500-3000 |
| Chia Seeds (1 tbsp) | 1 tbsp | 2000-2500 |
| Walnuts (1/4 cup) | 1/4 cup | 2500-3000 |
| Tuna (canned in water, 3 oz) | 3 oz | 1000-1500 |
Note: Values are approximate and can vary based on specific preparation and the type of fish or seed.
Eating foods high in omega-3 fatty acids is great for overall health, but did you know some conditions like hand pain can be related to underlying issues? For example, if you’re experiencing persistent hand pain, it’s crucial to understand the potential causes, available treatments, and when seeking medical attention is necessary. Checking out this informative article on hand pain causes treatment and when to see a doctor could provide valuable insight.
Fortunately, incorporating foods rich in omega-3s, like salmon and flaxseeds, can contribute to joint health and overall well-being.
Benefits of Omega-3 Consumption

Unlocking the power of omega-3 fatty acids offers a wealth of potential health benefits. These essential fats, crucial for various bodily functions, play a vital role in maintaining optimal well-being. From supporting heart health to boosting brain function, omega-3s are increasingly recognized for their diverse contributions to overall health.Consuming foods rich in omega-3 fatty acids is a proactive step towards a healthier lifestyle.
The diverse range of potential benefits extends from reducing inflammation to supporting cognitive function. By incorporating omega-3-rich foods into your diet, you can potentially experience a positive impact on your overall health and well-being.
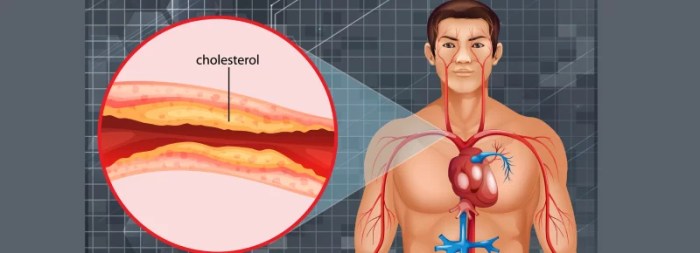
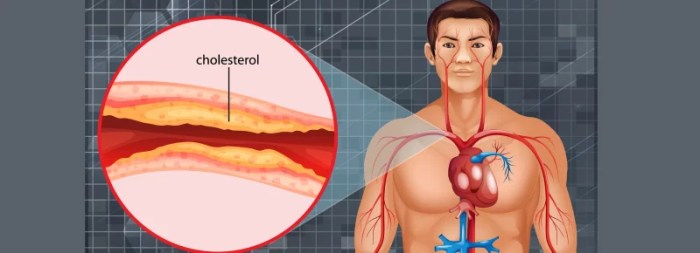
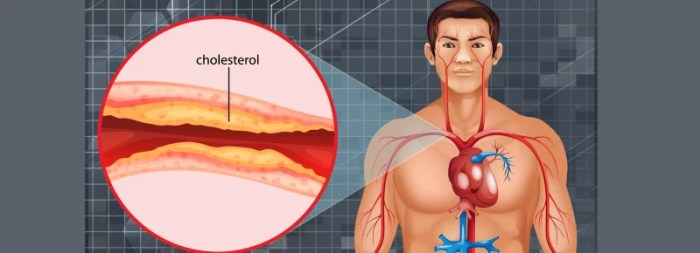
Role in Maintaining Heart Health
Omega-3s contribute significantly to cardiovascular health by reducing triglycerides, lowering blood pressure, and preventing the formation of blood clots. These actions collectively help maintain a healthy heart and reduce the risk of heart-related diseases. Studies have shown a correlation between omega-3 consumption and a decreased risk of coronary heart disease.
Impact on Brain Function and Cognitive Health
Omega-3 fatty acids are essential components of brain cell membranes, playing a vital role in brain structure and function. Adequate intake of omega-3s is linked to improved cognitive function, memory, and mood regulation. They are particularly important for brain development in children and maintaining cognitive health in older adults. This is reflected in various studies that have shown improved cognitive performance in individuals with sufficient omega-3 intake.
Eating foods high in omega-3 fatty acids can be a great way to support overall health, and it might even help with skin health. For example, incorporating foods like salmon, flaxseeds, and chia seeds into your diet can contribute to healthier skin, which in turn can potentially help prevent ingrown hairs, a common skin issue. Learning techniques for how to prevent ingrown hairs can be important too, and focusing on a balanced diet, including plenty of omega-3 rich foods, can contribute to this.
So, next time you’re stocking up on groceries, don’t forget to include some fantastic sources of omega-3s!
Contribution to Reducing Inflammation
Omega-3 fatty acids possess anti-inflammatory properties, helping to regulate the body’s inflammatory response. Chronic inflammation is linked to various health issues, and omega-3s can help mitigate this risk. By reducing inflammation throughout the body, omega-3s may contribute to overall well-being.
Health Conditions Where Omega-3s May Play a Beneficial Role
Omega-3s may offer potential benefits in managing a range of health conditions. This is based on ongoing research and observed correlations. These potential benefits should not be seen as a replacement for conventional medical treatments, but rather as a complementary approach to managing these conditions.
Eating foods high in omega-3 fatty acids is great for overall health, but did you know they might also play a role in your body’s response to illness? For example, if you’re experiencing neck pain alongside a cold or the flu, it’s worth checking out if there’s a connection. This article delves deeper into potential causes of neck pain during illness.
Regardless, incorporating foods like salmon, flaxseeds, and walnuts into your diet can provide essential omega-3s and support your immune system.
- Cardiovascular Disease: Omega-3s can help reduce triglycerides, lower blood pressure, and prevent blood clots, thereby potentially lowering the risk of heart disease and stroke.
- Arthritis: Some studies suggest that omega-3s may help reduce inflammation and pain associated with arthritis, potentially improving joint function.
- Depression and Anxiety: Research indicates a possible link between omega-3 intake and improved mood regulation, potentially reducing symptoms of depression and anxiety. The mechanism behind this effect is still being explored.
- ADHD: In some cases, omega-3 supplementation may help manage symptoms of attention deficit hyperactivity disorder (ADHD), particularly in children. More research is needed to fully understand the relationship.
- Pregnancy and Infant Development: Omega-3s are crucial for fetal brain development and may contribute to better cognitive outcomes in infants. Sufficient intake during pregnancy is essential.
Omega-3s and Dietary Considerations
Omega-3 fatty acids are essential for human health, playing a crucial role in various bodily functions. However, incorporating them into a balanced diet requires careful consideration of potential risks and benefits. A well-rounded approach to omega-3 consumption is vital, alongside mindful attention to other dietary aspects.Understanding the potential risks and benefits associated with omega-3 consumption is crucial for creating a healthy and sustainable dietary pattern.
Excessive intake from supplements or certain food sources can lead to potential negative effects, highlighting the importance of a balanced diet incorporating a variety of foods.
Potential Risks of Excessive Omega-3 Intake
High doses of omega-3s, especially from supplements, can potentially increase the risk of bleeding disorders. This is due to their blood-thinning properties. Individuals taking blood-thinning medications should consult their doctor before increasing omega-3 intake. Other potential side effects include nausea, heartburn, and diarrhea, particularly with high doses. It is important to prioritize moderation and consult a healthcare professional before significantly altering one’s omega-3 intake.
Importance of a Balanced Diet
A balanced diet is paramount for optimal health. It encompasses a variety of nutrient-rich foods from different food groups, ensuring adequate intake of essential vitamins, minerals, and fiber. This approach provides the body with the full spectrum of nutrients necessary for proper functioning. Omega-3s are beneficial, but their effectiveness is magnified when combined with a comprehensive dietary approach.
Comparing Dietary Patterns with Omega-3s
Different dietary patterns can effectively incorporate omega-3 rich foods. A Mediterranean diet, for instance, emphasizes fruits, vegetables, whole grains, and healthy fats, including omega-3s from sources like fish and olive oil. This pattern is often associated with numerous health benefits. Vegan or vegetarian diets can also be designed to include omega-3s from plant-based sources such as flaxseeds and chia seeds.
The key is to carefully plan and consider the overall nutrient profile of the diet.
Role of Omega-3s in Weight Management and Well-being
Omega-3s have been linked to various positive effects on weight management and overall well-being. They can contribute to reducing inflammation, which is often associated with weight gain. Studies suggest that omega-3s might help with appetite regulation, although further research is ongoing. Incorporating these healthy fats into a balanced diet, coupled with regular exercise, can be part of a comprehensive weight management strategy.
Potential Interactions with Medications or Supplements
Omega-3s can interact with certain medications, particularly blood thinners. It is essential to discuss any dietary changes, including omega-3 intake, with a doctor or pharmacist. This is particularly important for individuals taking prescription medications or supplements, ensuring that the combination doesn’t pose any health risks.
Examples of Recipes Using Omega-3 Rich Foods
| Recipe | Ingredients (Omega-3 Rich) | Preparation Technique |
|---|---|---|
| Salmon with Roasted Vegetables | Salmon fillets, broccoli, carrots, olive oil | Season salmon with herbs and spices. Roast vegetables with olive oil. Cook salmon alongside vegetables until cooked through. |
| Chia Seed Pudding | Chia seeds, milk (dairy or non-dairy), fruit, honey | Combine chia seeds with milk and let sit for at least 30 minutes to thicken. Top with desired fruit and honey. |
| Tuna Salad Sandwich | Canned tuna, Greek yogurt, celery, onion | Mix canned tuna with Greek yogurt, chopped celery, and onion. Season with salt and pepper. Serve on whole-wheat bread. |
These are just a few examples. Experiment with different flavors and ingredients to create your own delicious and healthy omega-3-rich meals. The preparation techniques highlight simplicity and ease of implementation.
Omega-3s in Different Cultures
Exploring the diverse ways cultures incorporate omega-3 fatty acids into their diets reveals fascinating insights into traditional food practices and their relationship with health. From the icy plains of the Arctic to the sun-drenched shores of the Mediterranean, the importance of omega-3s has been recognized in countless societies throughout history. Different regions have developed unique approaches to securing these vital nutrients, reflecting their local environments and culinary traditions.Traditional diets often prioritize foods readily available in a particular region, leading to varied omega-3 consumption patterns.
These patterns highlight the adaptability of human societies and their ability to utilize local resources for nutritional needs. Understanding these diverse practices provides a broader perspective on the importance of omega-3s in human health and highlights the rich tapestry of culinary traditions worldwide.
Variations in Omega-3 Consumption Across Cultures
Different cultures have evolved distinct approaches to obtaining omega-3 fatty acids. Factors like geographical location, available food sources, and traditional dietary practices play a significant role in shaping these variations. In some cultures, seafood is a staple, providing a rich source of omega-3s. In others, plant-based foods like flaxseeds or chia seeds contribute substantially to omega-3 intake. These variations highlight the adaptability of human diets and the diverse ways in which cultures meet their nutritional needs.
Traditional Dietary Practices Rich in Omega-3s
Many traditional societies have developed intricate knowledge systems surrounding the selection and preparation of foods rich in omega-3 fatty acids. In the Arctic regions, for instance, the consumption of fatty fish, such as salmon and seals, is deeply ingrained in their culture. These cultures have developed methods of preserving and preparing these foods, maximizing the nutritional value and ensuring year-round availability.
Similarly, in coastal communities around the world, seafood plays a central role in the diet, reflecting the availability of fresh catches. In addition, certain plant-based foods, like certain types of algae and seaweed, are also utilized in some cultures.
Examples of Traditional Dishes Rich in Omega-3s
Traditional dishes from various cultures showcase a wide array of omega-3-rich foods. In the Nordic countries, dishes like gravlax (cured salmon) and various types of seafood stews are common. In the Mediterranean region, dishes often feature fish, like grilled sardines and mackerel, as well as olive oil and nuts. In Asia, certain types of seaweed and algae are part of traditional dishes.
The preparation and ingredients of these dishes reflect the unique characteristics of the respective culinary traditions.
Comparison of Historical Omega-3 Consumption in Various Societies
Historical records and anthropological studies provide insights into the consumption of omega-3s in various societies throughout history. In ancient civilizations that had access to abundant marine resources, fish and seafood were likely a significant part of the diet. Evidence suggests that societies with limited access to these resources relied on plant-based sources of omega-3s, highlighting the adaptability of human diets.
Table of Food Sources and Consumption Patterns of Omega-3s in Various Cultures
| Culture | Primary Food Sources | Consumption Patterns |
|---|---|---|
| Arctic Regions (e.g., Inuit) | Fatty fish (salmon, seals), marine mammals | Regular consumption, integral part of traditional diet |
| Coastal Communities (e.g., Mediterranean) | Fish (sardines, mackerel), shellfish, olive oil, nuts | Frequent inclusion in meals, emphasis on fresh seafood |
| Asian Cultures (e.g., Japanese) | Seaweed, algae, fatty fish, certain types of nuts | Seaweed and algae consumption often part of daily diet |
| Certain African Communities | Plant-based sources (flaxseeds, chia seeds), local fish if available | Consumption patterns vary based on regional availability |
Omega-3 Rich Foods – Visual Representation

Embark on a visual journey into the world of omega-3s! This section delves into the rich tapestry of foods brimming with these essential fatty acids, showcasing their diverse forms and nutritional power. We’ll explore visual representations of omega-3 structures, alongside examples of delicious meals featuring these vital nutrients.This exploration aims to make understanding omega-3s more accessible and engaging, emphasizing the importance of incorporating these beneficial fats into a balanced diet.
We’ll visualize the power of omega-3s, connecting the structure of the fatty acids to their nutritional value and practical application in everyday meals.
Omega-3 Fatty Acid Structure
Understanding the structure of omega-3 fatty acids provides a deeper insight into their unique properties and how they differ from other fats. The distinguishing feature is the presence of a specific arrangement of carbon-hydrogen bonds, creating a bent shape. This structural characteristic affects how the body processes and utilizes omega-3s. A detailed illustration of this structure is crucial for appreciating the complexity of these vital nutrients.
A simplified representation of an omega-3 fatty acid chain shows a carbon backbone with alternating single and double bonds, culminating in a bent shape. This unique structure is essential for its biological function.
Visualizing Omega-3 Rich Foods
The following images showcase a variety of omega-3-rich foods in diverse, visually appealing presentations. Each image is accompanied by nutritional information, highlighting the rich sources of omega-3s. This visual approach aims to inspire and educate on the practical ways to incorporate omega-3s into everyday meals.
Image Description: A beautifully plated dish features pan-seared salmon fillets alongside roasted vegetables like broccoli, carrots, and bell peppers. The salmon is rich in omega-3s, while the vegetables contribute essential vitamins and minerals. This meal provides a balanced intake of nutrients.
Nutritional Information: Approx. 2000 mg omega-3 fatty acids per serving (salmon); High in vitamins A & C (vegetables).
Image Description: A vibrant and healthy chia seed pudding, topped with fresh berries and a drizzle of honey. Chia seeds are a fantastic source of omega-3s, fiber, and protein.
Nutritional Information: Approx. 2500 mg omega-3 fatty acids per serving; Excellent source of fiber and protein.
Image Description: A bowl of steamed edamame, a delicious and nutritious snack. Edamame offers a concentrated dose of omega-3s and other essential nutrients.
Nutritional Information: Approx. 500 mg omega-3 fatty acids per serving; Excellent source of protein and fiber.
Nutritional Information Table
| Food | Image | Approximate Omega-3 Content (per serving) | Other Key Nutrients |
|---|---|---|---|
| Salmon | [placeholder-image-1] | 2000 mg | Vitamin D, Protein |
| Chia Seeds | [placeholder-image-2] | 2500 mg | Fiber, Protein |
| Edamame | [placeholder-image-3] | 500 mg | Protein, Fiber |
Concluding Remarks
In conclusion, incorporating foods high in omega-3s into your diet can significantly contribute to your overall health and well-being. This guide has provided a detailed exploration of these essential fatty acids, highlighting their diverse sources, potential benefits, and crucial considerations for a balanced approach. From seafood to plant-based alternatives, we’ve explored a wide range of options to help you make informed choices about your nutrition.
Remember, a balanced diet and mindful consumption are key to reaping the full benefits of omega-3s.



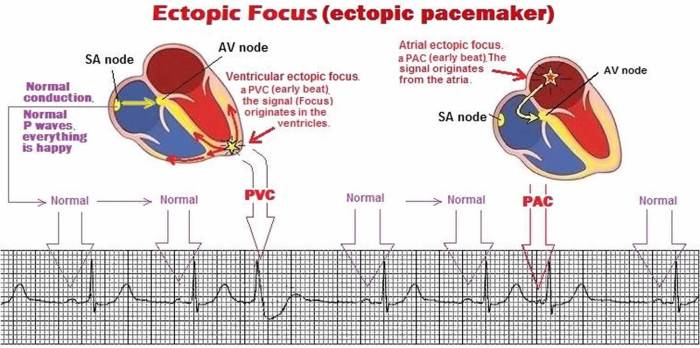
 (Diagram placeholder. A permanent pacemaker is typically implanted under the skin near the collarbone, with thin wires (leads) extending to the heart chambers. The pulse generator is housed within the implanted casing.)
(Diagram placeholder. A permanent pacemaker is typically implanted under the skin near the collarbone, with thin wires (leads) extending to the heart chambers. The pulse generator is housed within the implanted casing.)