Can pain cause high blood pressure? This complex question delves into the intricate relationship between pain and blood pressure, exploring how different types of pain impact our physiological responses. We’ll examine the immediate and long-term effects, considering factors like individual differences and pain management strategies. Understanding this connection is crucial for effectively managing both pain and blood pressure.
The physiological mechanisms linking pain to blood pressure changes are multifaceted. Pain signals trigger a cascade of responses within the nervous system, potentially leading to immediate and sustained increases in blood pressure. We’ll explore how acute and chronic pain conditions differ in their impact, considering examples and potential consequences.
Introduction to Pain and Blood Pressure
Pain is a complex experience that significantly impacts the body’s physiological functions. One such function often affected by pain is blood pressure. Understanding the intricate link between pain and blood pressure is crucial for effective pain management and the overall well-being of patients. This understanding allows healthcare professionals to anticipate potential complications and adjust treatment strategies accordingly.The relationship between pain and blood pressure is multifaceted, involving both immediate and long-term effects.
Physiological mechanisms like the release of stress hormones, activation of the sympathetic nervous system, and inflammatory responses can all contribute to fluctuations in blood pressure in response to pain. The type and duration of pain also play a significant role in the extent of these changes. Knowing how pain can influence blood pressure is vital for diagnosis, treatment planning, and patient education.
While pain itself doesn’t directly cause high blood pressure, it can definitely influence other factors that do. Stress from chronic pain, for example, can significantly impact blood pressure levels. Seeking help with managing these kinds of issues is crucial. Learning more about the challenges people face in accessing HIV care can provide valuable context for understanding how other health concerns might impact overall well-being.
For example, ask expert challenges getting hiv care to see how complex these situations can be. Ultimately, managing pain effectively is key to maintaining healthy blood pressure.
Physiological Mechanisms Linking Pain to Blood Pressure Changes
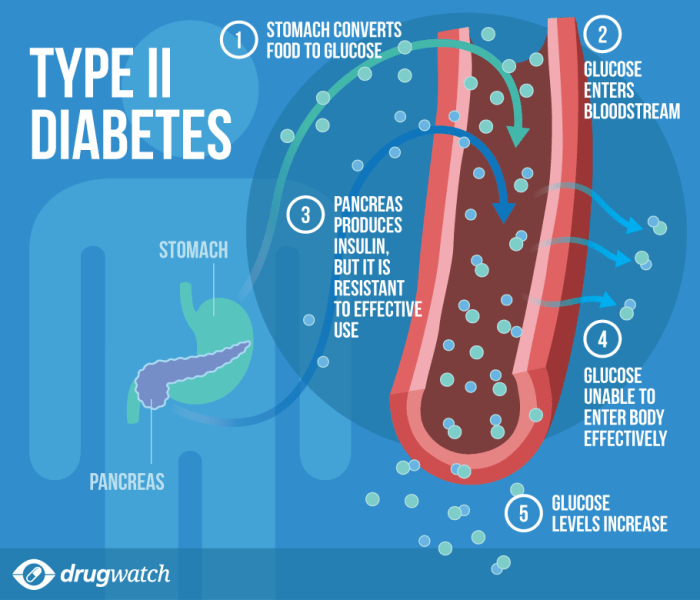
The body’s response to pain involves a complex interplay of neuroendocrine and autonomic nervous system pathways. Activation of the sympathetic nervous system, triggered by pain signals, releases catecholamines like adrenaline and noradrenaline. These hormones increase heart rate and constrict blood vessels, leading to a rise in blood pressure. Furthermore, pain can stimulate the release of other stress hormones, including cortisol, which can also contribute to blood pressure elevation.
Inflammation, often a component of pain, can also impact blood pressure through the release of inflammatory mediators. The extent of blood pressure change depends on the intensity and duration of the pain stimulus.
Types of Pain Affecting Blood Pressure
Different types of pain can trigger varying degrees of blood pressure changes. Acute pain, typically of short duration, often leads to transient elevations, whereas chronic pain, persisting over an extended period, can cause more sustained or even fluctuating blood pressure changes.
Acute and Chronic Pain Conditions and Their Impact on Blood Pressure
Acute pain conditions, such as a sudden injury or a toothache, often result in a temporary but significant rise in blood pressure. This response is a normal physiological reaction to the perceived threat. Chronic pain conditions, such as arthritis, fibromyalgia, or back pain, can lead to more sustained elevations or fluctuations in blood pressure, which can have long-term health consequences.
The impact on blood pressure is influenced by individual factors like pre-existing health conditions, age, and overall physical health.
Table of Pain Types and Blood Pressure Effects
| Pain Type | Potential Effect on Blood Pressure | Possible Mechanisms | Example Conditions |
|---|---|---|---|
| Acute Pain | Transient elevation; potentially significant rise | Release of catecholamines, activation of sympathetic nervous system, inflammatory response | Surgical procedures, injuries (fractures, sprains), dental procedures, labor and delivery |
| Chronic Pain | Sustained elevation or fluctuating changes; potentially long-term effects | Sustained release of stress hormones, chronic inflammation, psychological stress | Arthritis, fibromyalgia, back pain, neuropathic pain, cancer pain |
Immediate Effects of Pain on Blood Pressure
Pain, a universal human experience, triggers a cascade of physiological responses. Understanding these immediate effects on blood pressure is crucial for managing pain effectively and preventing potential complications. From the initial signal to the body’s reaction, the pathway is complex, influenced by various factors.The nervous system plays a central role in transmitting pain signals and initiating the body’s response.
These signals, when interpreted as pain, stimulate the autonomic nervous system, leading to a chain of events that can affect blood pressure. The intensity and type of pain significantly impact the magnitude of the response.
Physiological Responses to Pain
The body’s response to pain is multifaceted, involving the interplay of various systems. Pain signals, initiated by nociceptors (sensory nerve endings), are transmitted to the central nervous system. This triggers the release of stress hormones like adrenaline and noradrenaline, which increase heart rate and constrict blood vessels.
Pain Signals and Blood Pressure Increase
Pain signals activate the sympathetic nervous system, leading to a rapid increase in blood pressure. This response is a crucial part of the body’s “fight or flight” mechanism, preparing the individual to react to perceived threat. The body prioritizes blood flow to muscles involved in immediate action.
Short-Term Effects on Blood Pressure in Different Individuals
The immediate effect of pain on blood pressure varies among individuals. Factors such as age, overall health, pre-existing conditions, and the individual’s pain threshold all play a role. Younger, healthier individuals generally exhibit a more transient increase in blood pressure in response to acute pain, whereas those with underlying conditions may experience a more sustained elevation.
Influence of Pain Perception on Blood Pressure Reactions
Pain perception is subjective and can vary significantly between individuals. The perceived intensity of pain can influence the magnitude of the blood pressure response. A person who perceives a painful stimulus as intense will likely experience a greater increase in blood pressure compared to someone who perceives the same stimulus as less intense.
Table: Immediate Blood Pressure Responses to Different Pain Stimuli
| Stimulus Type | Typical Blood Pressure Response | Factors Affecting Response |
|---|---|---|
| Acute, localized pain (e.g., a paper cut) | A moderate, temporary increase in systolic and diastolic blood pressure. | Individual pain tolerance, health status, and pre-existing conditions. |
| Chronic, widespread pain (e.g., arthritis) | A more gradual, sustained increase in blood pressure, potentially leading to chronic hypertension in some cases. | Duration of pain, individual response to chronic stress, co-morbidities. |
| Intense, sudden pain (e.g., a severe burn) | A substantial and rapid increase in blood pressure, potentially reaching a critical level. | Severity of injury, individual’s physiological response to the injury, presence of other stressors. |
Long-Term Effects of Pain on Blood Pressure
Chronic pain isn’t just a temporary discomfort; it can have profound and lasting effects on your overall health, including your blood pressure. Understanding these long-term impacts is crucial for managing chronic pain effectively and preventing potential complications. The consistent stress and altered physiological responses associated with chronic pain can significantly affect blood pressure regulation, potentially leading to hypertension and related health issues.The continuous activation of the body’s stress response systems due to chronic pain plays a significant role in long-term blood pressure elevation.
This sustained activation can lead to a persistent increase in blood pressure, making individuals more susceptible to cardiovascular diseases. Factors like the intensity and duration of pain, individual pain tolerance, and co-occurring health conditions further complicate the picture, contributing to variations in the long-term impact on blood pressure.
Impact on Blood Pressure Regulation
Chronic pain disrupts the delicate balance of the body’s blood pressure regulatory mechanisms. The nervous system, tasked with maintaining homeostasis, is constantly challenged by the persistent pain signal. This ongoing stimulation leads to a heightened state of sympathetic nervous system activity, resulting in a sustained release of stress hormones like adrenaline and cortisol. These hormones cause blood vessels to constrict, increasing blood pressure.
Furthermore, the body’s inflammatory response, often triggered or exacerbated by chronic pain, can also contribute to blood pressure elevation. This complex interplay of factors can lead to a gradual but significant increase in blood pressure over time.
Contributing Factors to Hypertension
Several factors can increase the risk of hypertension in individuals experiencing chronic pain. These factors interact and can amplify the impact of pain on blood pressure. A sedentary lifestyle, poor diet, and lack of sleep often accompany chronic pain, further exacerbating the risk of hypertension. Pre-existing health conditions, such as diabetes or kidney disease, can also increase susceptibility.
Additionally, the psychological distress associated with chronic pain, including anxiety and depression, can contribute to heightened blood pressure responses.
Role of Stress Hormones and Nervous System
The sustained release of stress hormones like adrenaline and cortisol in response to chronic pain plays a key role in long-term blood pressure elevation. These hormones trigger vasoconstriction, leading to an increase in blood pressure. The continuous activation of the sympathetic nervous system, the body’s “fight or flight” response, further contributes to this elevation. Chronic pain can lead to a sustained state of sympathetic nervous system activation, leading to higher blood pressure readings over time.
The constant stress response, while crucial for short-term survival, becomes detrimental when prolonged.
Acute vs. Chronic Pain Effects
Acute pain, like a sprained ankle, triggers a temporary increase in blood pressure. This response is a protective mechanism, allowing for quicker blood flow to injured tissues. However, this response is transient, returning to normal levels as the injury heals. In contrast, chronic pain, such as that experienced with arthritis or fibromyalgia, triggers a sustained and elevated blood pressure response.
This persistent elevation can lead to long-term damage to blood vessels and the heart, significantly increasing the risk of hypertension and related cardiovascular issues.
Potential Long-Term Consequences
| Chronic Pain Duration | Potential Blood Pressure Changes | Contributing Factors | Potential Complications |
|---|---|---|---|
| Short-term (weeks) | Temporary increase in blood pressure | Injury, inflammation, acute stress | Generally, no long-term complications if pain resolves |
| Long-term (months to years) | Sustained elevation in blood pressure, potentially leading to hypertension | Chronic inflammation, stress hormones, psychological distress, lifestyle factors | Increased risk of cardiovascular diseases (heart attack, stroke), kidney disease, and other health issues |
Factors Influencing the Pain-Blood Pressure Relationship
Understanding the complex interplay between pain and blood pressure involves more than just the immediate physiological response. Individual characteristics, pain management strategies, and the medications used to alleviate pain all play significant roles in shaping this connection. This section delves into these influencing factors to provide a more complete picture of how pain impacts blood pressure.
Individual Factors
Various individual characteristics can modify the pain-blood pressure response. Age, for instance, plays a role. Older adults may have pre-existing cardiovascular conditions that can amplify the blood pressure rise in response to pain. Gender differences can also be significant. Studies suggest that women may experience a slightly different blood pressure response to pain compared to men, potentially due to hormonal variations.
Pre-existing conditions, such as hypertension or diabetes, significantly influence the blood pressure reaction to pain. These conditions often predispose individuals to more pronounced elevations in blood pressure when experiencing pain. The existing health status of the individual substantially influences the relationship between pain and blood pressure, highlighting the need for personalized approaches to pain management.
Pain Management Strategies
Effective pain management is crucial in regulating blood pressure during and after a painful experience. Non-pharmacological methods, such as relaxation techniques, mindfulness practices, and physical therapy, can significantly reduce pain perception and subsequently mitigate the stress response, which is often a major contributor to blood pressure elevation. These strategies are particularly important for chronic pain conditions, where sustained high blood pressure can lead to long-term health issues.
Proper implementation of pain management strategies can lead to a more controlled and predictable blood pressure response to pain, promoting better overall health.
Medications and Blood Pressure
Pain relievers, while essential for managing pain, can sometimes have a secondary impact on blood pressure. Nonsteroidal anti-inflammatory drugs (NSAIDs), for example, can potentially elevate blood pressure in some individuals, especially those with pre-existing hypertension. Opioid analgesics, often used for severe pain, can also affect blood pressure, sometimes leading to a decrease, but potentially increasing the risk of hypotension in certain cases.
The precise effect of a medication on blood pressure depends on several factors, including the individual’s sensitivity, the dosage, and the presence of other medications. Careful monitoring of blood pressure is crucial when using pain medications, especially in those with pre-existing cardiovascular issues.
Examples of Pain Management Techniques
Numerous pain management techniques can influence blood pressure. Heat therapy, for instance, can help relax muscles and reduce pain signals, leading to a more controlled blood pressure response. Acupuncture, a traditional Chinese medicine practice, has shown promise in reducing pain perception and modulating the body’s stress response, thereby impacting blood pressure levels. Cognitive behavioral therapy (CBT) can help patients manage pain by changing their thoughts and behaviors related to pain, which can be very effective in mitigating the psychological stress associated with pain.
These techniques, when incorporated into a comprehensive pain management plan, can have a positive impact on blood pressure regulation.
Factors Influencing the Pain-Blood Pressure Relationship
| Factor | Description | Impact on Blood Pressure | Example |
|---|---|---|---|
| Age | Older individuals may have pre-existing cardiovascular conditions. | Increased susceptibility to blood pressure elevation. | A 70-year-old experiencing back pain might see a more pronounced rise in blood pressure than a 30-year-old. |
| Gender | Potential hormonal differences influence the blood pressure response. | May lead to slightly varying responses. | Women might experience a slightly different blood pressure response to pain than men. |
| Pre-existing conditions | Conditions like hypertension or diabetes can amplify the response. | Higher risk of significant blood pressure elevation. | A patient with hypertension experiencing toothache may see a more substantial blood pressure increase. |
| Pain management strategies | Relaxation techniques, mindfulness, and physical therapy can reduce pain perception. | Mitigation of stress response, leading to lower blood pressure. | Employing deep breathing exercises during a migraine can help regulate blood pressure. |
| Medications | NSAIDs and opioids can potentially elevate or lower blood pressure. | Individual sensitivity and dosage are crucial. | A patient taking NSAIDs for arthritis may experience a slight increase in blood pressure. |
Seeking Medical Attention and Management
Chronic pain can significantly impact blood pressure, sometimes leading to hypertension. Ignoring this connection can have serious health consequences. Understanding the interplay between pain and blood pressure, and how to manage both effectively, is crucial for overall well-being.Effective management of pain and blood pressure requires a multi-faceted approach that considers both the acute and chronic aspects of these conditions.
Healthcare professionals play a vital role in guiding patients toward personalized strategies that address the unique needs of each individual.
Wondering if pain can elevate blood pressure? It’s a complex question, and the answer isn’t always straightforward. Chronic conditions like rheumatoid arthritis can significantly impact blood pressure. Fortunately, advancements in treatment like new rheumatoid arthritis treatment are offering promising new ways to manage symptoms and potentially reduce the strain on the cardiovascular system, which can indirectly affect blood pressure levels.
So, while pain itself might not directly cause high blood pressure, the underlying conditions causing the pain often do play a role.
Importance of Professional Guidance
Seeking medical advice is essential when pain consistently affects blood pressure readings. A healthcare professional can accurately assess the relationship between pain and blood pressure changes, identifying underlying causes and developing a tailored management plan. This personalized approach is crucial because the impact of pain on blood pressure can vary significantly depending on factors like the type of pain, its intensity, and the individual’s overall health.
Role of Healthcare Professionals
Healthcare professionals, including doctors, nurses, and pain specialists, are instrumental in managing pain and blood pressure concurrently. They evaluate the patient’s medical history, current medications, and lifestyle factors. This comprehensive assessment allows them to identify potential interactions between pain medications and blood pressure treatments. Crucially, they can also recommend strategies to manage both conditions safely and effectively.
Collaboration between patients and healthcare providers is key to successful management.
Effective Pain Management Strategies for Hypertension, Can pain cause high blood pressure
Several pain management strategies are effective for patients with hypertension. These strategies often incorporate a combination of approaches, aiming to reduce pain and stabilize blood pressure. Pharmacological interventions, such as specific pain relievers and blood pressure medications, may be employed. However, non-pharmacological methods, such as physical therapy, relaxation techniques, and lifestyle modifications, often play a crucial role.
While pain itself might not directly cause high blood pressure, it can definitely trigger a cascade of stress hormones that could elevate blood pressure. Think about the dangers of mixing cleaning chemicals, like the potential for hazardous reactions when mixing bleach and ammonia, a potentially dangerous experiment. Similarly, intense pain can cause similar physiological responses that affect blood pressure.
It’s a complex interplay of factors, so it’s important to understand the overall context for potential health impacts.
- Physical Therapy: Targeted exercises and stretches can alleviate pain and improve mobility, contributing to a healthier lifestyle. This is particularly beneficial for musculoskeletal pain. Examples include exercises for back pain, neck pain, or joint pain, tailored to individual needs.
- Cognitive Behavioral Therapy (CBT): CBT can help patients manage the emotional and psychological aspects of chronic pain. It teaches coping mechanisms and strategies for managing stress and anxiety, which can influence blood pressure levels.
- Mindfulness and Relaxation Techniques: Practices like meditation and deep breathing exercises can reduce stress and anxiety, leading to better blood pressure control. These techniques can also help manage the pain experience itself.
Holistic Approach to Pain Management
A holistic approach to pain management recognizes the interconnectedness of physical, emotional, and social factors. Lifestyle changes, such as regular exercise, a balanced diet, and sufficient sleep, are integral components of this approach. These lifestyle modifications not only help manage pain but also contribute to overall cardiovascular health, reducing the risk of hypertension complications. A combination of medication, therapy, and lifestyle adjustments can significantly improve both pain and blood pressure management.
Managing Pain and Blood Pressure Concurrently
| Approach | Description | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Pharmacological Intervention | Using prescribed medications for pain relief and blood pressure control. | Rapid pain relief and blood pressure stabilization. | Potential for side effects, drug interactions, and dependence. |
| Non-Pharmacological Therapies | Techniques like physical therapy, relaxation exercises, and CBT. | Improved pain management, reduced reliance on medication, and enhanced well-being. | May take longer to show results, requiring patience and adherence to the prescribed regimen. |
| Lifestyle Modifications | Changes in diet, exercise, sleep, and stress management. | Improved overall health, reduced risk of cardiovascular complications, and long-term pain relief. | Requires commitment and consistent effort, potentially leading to initial discomfort or challenges. |
Illustrative Case Studies (Hypothetical)

Understanding the intricate link between pain and blood pressure requires examining diverse patient responses. Hypothetical case studies offer a glimpse into this complex relationship, highlighting the variability in symptoms, diagnoses, and management strategies. These scenarios emphasize the importance of personalized approaches to managing both pain and hypertension.
Case Study 1: Chronic Back Pain
Chronic back pain, often stemming from conditions like osteoarthritis or herniated discs, can significantly impact blood pressure. This case study involves a 55-year-old woman experiencing persistent back pain for over a year. Initial blood pressure readings were consistently elevated, reaching 140/90 mmHg. Diagnosis included a thorough assessment of her medical history and physical examination, coupled with imaging tests to identify the source of the pain.
The management strategy involved a multifaceted approach, encompassing physical therapy, pain medications like NSAIDs, and stress reduction techniques. Careful monitoring of blood pressure throughout the treatment was crucial. The long-term outcome involved sustained pain management, blood pressure control, and improved quality of life.
Case Study 2: Post-Surgical Pain
Post-operative pain, a common experience following major surgeries, can induce a temporary increase in blood pressure. Consider a 62-year-old man undergoing a major abdominal surgery. He experienced significant pain post-operatively, accompanied by elevated blood pressure readings. The management plan included administering appropriate pain medication, adjusting the medication dosage to manage both pain and blood pressure, and close monitoring in the hospital.
A focus on proper hydration and medication adherence significantly influenced the outcome, leading to successful blood pressure control and prompt recovery.
Case Study 3: Fibromyalgia
Fibromyalgia, a chronic pain condition characterized by widespread pain, fatigue, and tenderness, often presents with hypertension. This case study centers on a 40-year-old woman diagnosed with fibromyalgia. She presented with fluctuating blood pressure readings, often spiking during periods of increased pain. Treatment involved a combination of pain management strategies such as medication, physical therapy, and lifestyle adjustments, like stress management techniques.
Maintaining a consistent pain management plan, regular exercise, and dietary changes were vital to long-term blood pressure control and overall well-being.
Case Study Summary
| Case Study | Pain Type | Blood Pressure Profile | Treatment Approach | Outcomes |
|---|---|---|---|---|
| Chronic Back Pain | Musculoskeletal | Elevated, consistent | Multimodal: Physical therapy, pain meds, stress reduction | Sustained pain management, blood pressure control, improved quality of life |
| Post-Surgical Pain | Acute, post-operative | Elevated, temporary | Pain medication, close monitoring, hydration | Successful blood pressure control, prompt recovery |
| Fibromyalgia | Widespread, chronic | Fluctuating, pain-related spikes | Combination therapy: Medication, physical therapy, lifestyle changes | Long-term blood pressure control, improved well-being |
Last Recap: Can Pain Cause High Blood Pressure
In conclusion, the connection between pain and high blood pressure is multifaceted and influenced by various factors. While acute pain may cause temporary increases, chronic pain can have more significant and lasting effects on blood pressure regulation. Understanding these complexities is key to developing effective pain management strategies that consider blood pressure implications. Ultimately, consulting with healthcare professionals is essential for personalized care and effective management of both pain and blood pressure.