Insulin vs blood sugar how to manage type 2 diabetes – Insulin vs blood sugar: how to manage type 2 diabetes. This guide dives deep into the intricate relationship between blood sugar and insulin, specifically focusing on the challenges and solutions for those living with type 2 diabetes. We’ll explore the science behind blood sugar regulation, the underlying mechanisms of insulin resistance, and practical strategies for managing your blood sugar effectively.
From understanding the different types of diabetes to learning about various management methods, including medications, diet, and exercise, this comprehensive guide equips you with the knowledge to take control of your health. We’ll also cover crucial aspects like monitoring blood sugar levels and long-term management strategies.
Understanding Blood Sugar and Insulin
Maintaining healthy blood sugar levels is crucial for overall well-being. A complex interplay of hormones and processes keeps our blood sugar balanced, providing the energy our bodies need. Disruptions in this delicate system can lead to serious health problems, including type 2 diabetes. This section delves into the intricacies of blood sugar regulation, the role of insulin, common imbalances, and different types of diabetes.Blood sugar, also known as glucose, is the primary source of energy for the body’s cells.
Managing blood sugar levels with insulin is key for type 2 diabetes, but sometimes digestive issues like diarrhea can complicate things. Finding the right over-the-counter or prescription medications for diarrhea relief can be a real game-changer for overall health, especially when managing a condition like diabetes. For a comprehensive guide on various options, check out this resource on diarrhea relief otc and prescription medications.
Ultimately, a balanced approach to both managing diarrhea and blood sugar levels is essential for effective type 2 diabetes management.
It circulates in the bloodstream and is vital for various bodily functions. A healthy body meticulously regulates blood sugar levels to ensure optimal cellular function.
How Blood Sugar is Regulated in a Healthy Body
The body maintains blood sugar levels through a tightly controlled feedback loop involving the pancreas, liver, and other organs. The pancreas, a vital gland, plays a pivotal role in this process. It secretes hormones, including insulin, which facilitates the uptake of glucose from the bloodstream into cells. Conversely, the pancreas also produces glucagon, which stimulates the liver to release stored glucose into the bloodstream when blood sugar levels drop.
This balanced system ensures a consistent supply of energy to cells.
The Role of Insulin
Insulin is a hormone produced by the beta cells of the pancreas. Its primary function is to facilitate the transport of glucose from the bloodstream into the cells. When blood sugar rises, typically after a meal, the pancreas releases insulin to enable cells to absorb glucose, lowering blood sugar levels. This process is essential for preventing hyperglycemia (high blood sugar).
Insulin acts like a key, unlocking the doors of cells to allow glucose entry. Without sufficient insulin or when cells become resistant to insulin, glucose remains in the bloodstream, leading to elevated blood sugar levels.
Common Causes of Blood Sugar Imbalances
Numerous factors can disrupt the delicate balance of blood sugar regulation. A sedentary lifestyle, poor dietary choices, and genetics are common culprits. A diet high in refined carbohydrates and sugar can cause rapid spikes in blood sugar, while a lack of physical activity can reduce the body’s ability to utilize glucose effectively. Genetic predisposition also plays a significant role, as certain individuals are more prone to developing blood sugar imbalances.
Underlying health conditions, such as hormonal imbalances or certain medications, can also contribute to blood sugar issues.
Examples of Blood Sugar Imbalances
Blood sugar imbalances manifest in various forms. Hyperglycemia, or high blood sugar, is a common symptom of poorly managed diabetes, characterized by elevated blood glucose levels. Hypoglycemia, or low blood sugar, is another concern, particularly for people with diabetes who take medications to lower their blood sugar. In hypoglycemia, blood glucose levels fall too low, potentially leading to symptoms like dizziness, sweating, and confusion.
These imbalances require prompt medical attention.
Types of Blood Sugar Imbalances (Diabetes)
Diabetes is a chronic metabolic disorder characterized by elevated blood sugar levels. Type 1 diabetes results from the body’s immune system mistakenly attacking and destroying insulin-producing cells in the pancreas. This leads to a complete or near-complete lack of insulin production, requiring lifelong insulin therapy. Type 2 diabetes, on the other hand, arises from insulin resistance, where the body’s cells do not respond effectively to insulin.
Over time, this can lead to a decrease in insulin production. Gestational diabetes is a temporary form of diabetes that can develop during pregnancy. It usually resolves after childbirth but increases the risk of developing type 2 diabetes later in life.
Normal Blood Sugar Ranges and Ranges for Prediabetes and Diabetes
| Blood Sugar Range | Condition |
|---|---|
| 70-99 mg/dL (fasting) | Normal |
| 100-125 mg/dL (fasting) | Prediabetes |
| 126 mg/dL or higher (fasting) | Diabetes |
Note: Fasting blood sugar levels are measured after an overnight fast.
Type 2 Diabetes

Understanding how your body manages blood sugar is crucial, especially if you have type 2 diabetes. This condition arises when your body becomes resistant to insulin, the hormone responsible for transporting glucose from your blood into your cells. This resistance leads to elevated blood sugar levels, which can have significant health consequences if left unmanaged.
Insulin Resistance: A Deep Dive
Insulin resistance is a key factor in type 2 diabetes. It occurs when cells in the body, particularly muscle, liver, and fat cells, do not respond effectively to insulin. Consequently, the body produces more insulin to compensate, but this increased production often fails to lower blood sugar levels adequately. This creates a vicious cycle, eventually leading to high blood sugar.
Lifestyle Factors Contributing to Insulin Resistance
Several lifestyle choices can increase your risk of developing insulin resistance. A diet high in processed foods, sugary drinks, and unhealthy fats often contributes to insulin resistance. Lack of regular physical activity further exacerbates the issue. Being overweight or obese is another significant factor, as excess fat tissue can impair insulin signaling. Genetic predisposition also plays a role in some cases, highlighting the importance of understanding your family history.
Physiological Mechanisms of Insulin Resistance in Type 2 Diabetes
Insulin resistance stems from several interconnected physiological mechanisms. These include impaired insulin signaling pathways, reduced insulin receptor expression, and altered glucose uptake in cells. These changes disrupt the normal process of glucose metabolism, leading to the buildup of glucose in the bloodstream. The precise interplay of these mechanisms varies between individuals, reflecting the complexity of the disease.
Diet, Exercise, and Insulin Resistance: The Interplay, Insulin vs blood sugar how to manage type 2 diabetes
Diet, exercise, and insulin resistance are intrinsically linked. A balanced diet low in processed foods and refined sugars can significantly improve insulin sensitivity. Regular physical activity, even moderate intensity exercise, enhances insulin action by increasing glucose uptake in muscles. These lifestyle modifications can effectively combat insulin resistance, making it a crucial part of managing type 2 diabetes.
Dietary Strategies for Managing Blood Sugar
Managing blood sugar requires a tailored dietary approach. Different strategies can be employed, and the effectiveness often depends on individual needs and preferences.
| Dietary Strategy | Description |
|---|---|
| Low Glycemic Index Diet | Focuses on foods that cause a slower rise in blood sugar. |
| Mediterranean Diet | Emphasizes fruits, vegetables, whole grains, and healthy fats. |
| Carbohydrate Counting | Involves tracking and managing carbohydrate intake. |
| DASH Diet | Promotes fruits, vegetables, and low-fat dairy, while limiting saturated and trans fats. |
Common Symptoms of Type 2 Diabetes
Type 2 diabetes often manifests with subtle symptoms that may go unnoticed for years. Early detection is crucial for effective management.
- Frequent urination, especially at night.
- Increased thirst.
- Unexplained weight loss.
- Increased hunger.
- Fatigue and tiredness.
- Blurred vision.
- Slow-healing sores.
- Frequent infections.
- Numbness or tingling in the hands or feet.
Managing Blood Sugar in Type 2 Diabetes
Successfully managing blood sugar levels is crucial for preventing long-term complications in type 2 diabetes. This involves a multifaceted approach that goes beyond just medication. A holistic strategy incorporating lifestyle modifications plays a vital role in achieving and maintaining healthy blood sugar control.Effective blood sugar management in type 2 diabetes requires a combination of strategies tailored to individual needs.
Managing type 2 diabetes involves understanding the delicate balance between insulin and blood sugar. It’s crucial to adopt healthy lifestyle choices and, sometimes, medication. While exploring ways to control blood sugar, it’s important to remember that certain factors can increase the risk of contracting other health conditions, such as herpes. Understanding the risk factors for herpes, like those discussed in herpes causes risk factors , can help in making informed decisions about overall health.
Ultimately, a comprehensive approach to managing type 2 diabetes, including regular check-ups and a healthy diet, is key.
This includes understanding the role of medication, the significance of a healthy diet, and the benefits of regular exercise. Consistency in these approaches is key to long-term health.
Managing blood sugar levels in type 2 diabetes is crucial, and understanding insulin’s role is key. One aspect of managing this condition involves lifestyle changes, but did you know that physical therapy techniques like contrast baths can also play a part? A technique like contrast bath in physical therapy can improve circulation and reduce inflammation, potentially aiding in overall health and blood sugar control.
Ultimately, the best approach to managing type 2 diabetes often involves a combination of strategies, including dietary changes and regular exercise.
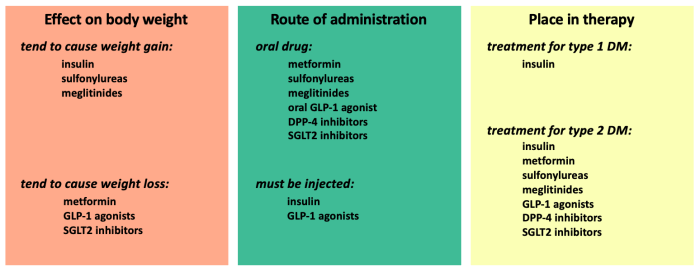
Medication for Blood Sugar Control
Medications are often prescribed to help lower blood sugar levels in individuals with type 2 diabetes. These medications work through various mechanisms, targeting different aspects of glucose metabolism. Understanding how these medications function can empower individuals to actively participate in their treatment plan.
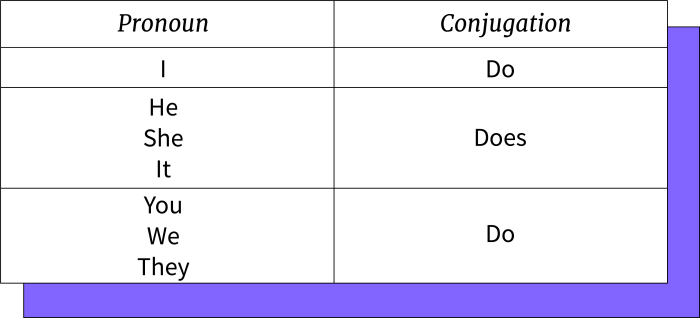
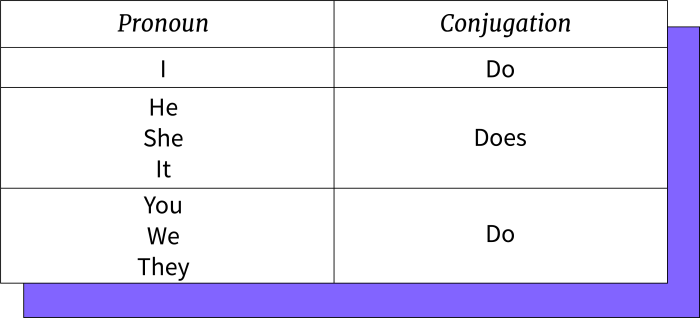
Common Diabetes Medications and Their Mechanisms of Action
Several classes of medications are used to manage blood sugar in type 2 diabetes. Each class has unique mechanisms of action.
- Metformin: This is often the first-line medication prescribed for type 2 diabetes. It works by reducing glucose production in the liver and improving insulin sensitivity in muscle cells. It generally has a low risk of hypoglycemia (low blood sugar). A common example of a metformin dosage is 500 mg twice daily.
- Sulfonylureas: These medications stimulate the pancreas to release more insulin. Examples include glimepiride and glipizide. A possible side effect is hypoglycemia. It’s important to note that dosage and frequency will vary based on individual needs and blood sugar response.
- DPP-4 Inhibitors: These medications help to increase the amount of incretin hormones, which stimulate insulin release and decrease glucagon secretion (a hormone that raises blood sugar). Examples include sitagliptin and saxagliptin. Side effects are generally mild and infrequent.
- GLP-1 Receptor Agonists: These medications mimic the action of a naturally occurring hormone that slows gastric emptying, increases insulin release, and decreases glucagon secretion. Examples include liraglutide and exenatide. Potential side effects include nausea and vomiting, particularly in the initial phase of treatment.
Importance of Diet and Exercise
A healthy diet and regular exercise are essential components of managing type 2 diabetes. They work synergistically to improve insulin sensitivity and help regulate blood sugar levels. The positive effects extend beyond just managing blood sugar; they promote overall well-being.
Healthy Meal Plans for Type 2 Diabetes
A healthy meal plan for type 2 diabetes focuses on portion control, balanced macronutrients, and a variety of nutrient-rich foods. It emphasizes whole grains, lean proteins, fruits, vegetables, and healthy fats. The goal is to create sustainable eating habits that support long-term blood sugar control.
- Example Meal Plan 1 (Day): Breakfast: Oatmeal with berries and nuts; Lunch: Salad with grilled chicken or fish; Dinner: Baked salmon with roasted vegetables. This plan emphasizes lean protein, healthy fats, and complex carbohydrates.
- Example Meal Plan 2 (Day): Breakfast: Greek yogurt with fruit and granola; Lunch: Lentil soup with whole-wheat bread; Dinner: Chicken stir-fry with brown rice and plenty of vegetables. This example highlights plant-based protein and whole grains.
Exercise and Insulin Sensitivity
Regular exercise plays a crucial role in improving insulin sensitivity. Physical activity helps muscles absorb glucose more effectively, reducing the strain on the pancreas. This effect can improve blood sugar control over time.
Comparison of Diabetes Medications
| Medication Class | Examples | Mechanism of Action | Potential Side Effects |
|---|---|---|---|
| Metformin | Metformin | Reduces glucose production, improves insulin sensitivity | Gastrointestinal upset (e.g., diarrhea), vitamin B12 deficiency |
| Sulfonylureas | Glimepiride, Glipizide | Stimulates insulin release from the pancreas | Hypoglycemia, weight gain |
| DPP-4 Inhibitors | Sitagliptin, Saxagliptin | Increases incretin hormones, stimulating insulin release and decreasing glucagon secretion | Mild upper respiratory tract infections, headache |
| GLP-1 Receptor Agonists | Liraglutide, Exenatide | Mimics incretin hormones, slows gastric emptying, increases insulin release, decreases glucagon secretion | Nausea, vomiting, diarrhea, potential risk of thyroid tumors (some studies show a possible link) |
Monitoring Blood Sugar Levels: Insulin Vs Blood Sugar How To Manage Type 2 Diabetes
Staying on top of your blood sugar levels is crucial for managing type 2 diabetes effectively. Consistent monitoring provides valuable insights into how your body responds to different foods, activities, and medications. It empowers you to make informed choices that contribute to your overall well-being and help prevent long-term complications.Understanding your blood sugar patterns allows you to anticipate potential issues and adjust your lifestyle accordingly.
This proactive approach minimizes the risk of complications and promotes a healthier, more stable life.
Methods of Monitoring Blood Sugar Levels
Various methods exist for monitoring blood sugar levels. These methods range from traditional finger-prick tests to more advanced continuous glucose monitoring systems. Each approach offers unique advantages and disadvantages.
Importance of Regular Blood Sugar Monitoring
Regular blood sugar monitoring is essential for managing type 2 diabetes effectively. By tracking blood glucose levels, you gain a clearer understanding of how your body responds to different factors, enabling you to adjust your diet, exercise routine, and medication as needed. This proactive approach significantly reduces the risk of developing long-term complications.
Potential Complications of Uncontrolled Blood Sugar Levels
Uncontrolled blood sugar levels can lead to several serious complications. These complications range from nerve damage and kidney problems to cardiovascular issues and eye damage. Consistent monitoring and appropriate management are vital in preventing these potentially life-altering conditions.
Blood Sugar Monitoring Tools and Devices
Numerous blood sugar monitoring tools and devices are available. These include traditional glucometers, which require finger pricks to measure glucose levels, and continuous glucose monitors (CGMs), which provide real-time glucose readings. The choice of device depends on individual needs and preferences.
Steps for Properly Testing Blood Sugar Levels at Home
Proper technique is critical for accurate blood sugar readings. Following these steps ensures reliable results and helps in making informed decisions:
- Wash your hands thoroughly with soap and water, and dry them completely.
- Select a clean lancet and prepare the lancing device.
- Select a fingertip, usually the one on the side of the finger, to prevent repeated pricks in the same spot.
- Gently wipe the selected fingertip with an alcohol swab.
- Insert the lancet into the lancing device and gently press it against the fingertip.
- Collect the blood sample onto the test strip.
- Insert the test strip into the glucometer.
- Follow the instructions on the glucometer to obtain the blood sugar reading.
- Record the reading in a logbook or app.
Summary of Blood Sugar Monitoring Methods
| Method | Pros | Cons |
|---|---|---|
| Finger-prick testing (Glucometer) | Affordable, widely available, easy to use at home. | Requires finger pricks, results are delayed, may not be suitable for frequent monitoring. |
| Continuous Glucose Monitoring (CGM) | Provides real-time glucose readings, allows for better understanding of glucose fluctuations, potentially reduces hypoglycemic events. | More expensive, requires calibration, may cause skin irritation, requires device management. |
| Self-Monitoring of Blood Glucose (SMBG) | Can be done at home, provides a record of blood glucose fluctuations. | Requires a finger prick, not ideal for continuous monitoring, can be prone to errors if not performed correctly. |
Long-Term Management and Prevention
Living with type 2 diabetes requires a commitment to long-term management. This commitment involves ongoing adjustments to lifestyle, medication, and monitoring to maintain good health and prevent complications. A proactive approach to prevention and management can significantly improve quality of life and reduce the risk of serious health issues.Maintaining stable blood sugar levels over the long term is crucial for preventing complications such as heart disease, nerve damage, and kidney problems.
Consistent monitoring and adherence to treatment plans are essential components of this long-term strategy. The proactive approach not only reduces the risk of developing complications but also significantly enhances overall well-being.
Importance of Long-Term Management
Long-term management of type 2 diabetes is essential for preventing or delaying the onset of serious complications. By consistently managing blood sugar levels, blood pressure, and cholesterol, individuals can significantly reduce the risk of cardiovascular disease, nerve damage (neuropathy), kidney disease (nephropathy), and eye problems (retinopathy). These complications can lead to significant disability and reduced quality of life.
Strategies for Preventing Type 2 Diabetes
Prevention of type 2 diabetes is achievable through lifestyle modifications. Adopting healthy habits early in life can substantially reduce the risk of developing the condition. Individuals can actively contribute to their health outcomes by prioritizing a healthy lifestyle.
Role of Lifestyle Choices
Lifestyle choices play a pivotal role in both preventing and managing type 2 diabetes. Dietary habits and regular physical activity are critical components of a healthy lifestyle. Maintaining a healthy weight, consuming a balanced diet rich in fruits, vegetables, and whole grains, and engaging in regular physical activity can significantly lower the risk of developing type 2 diabetes.
Furthermore, regular exercise improves insulin sensitivity, which helps regulate blood sugar levels.
Examples of Support Groups and Resources
Numerous support groups and resources are available to individuals with type 2 diabetes. These resources provide valuable information, emotional support, and practical guidance. Local diabetes support groups, online forums, and healthcare professionals can offer guidance and encouragement. Diabetes education programs can empower individuals with the knowledge and tools necessary to effectively manage their condition.
Common Long-Term Complications of Diabetes
| Complication | Description |
|---|---|
| Cardiovascular Disease | Increased risk of heart attack, stroke, and peripheral artery disease. |
| Neuropathy | Damage to nerves, leading to pain, numbness, and tingling, often in the hands and feet. |
| Nephropathy | Damage to the kidneys, potentially leading to kidney failure. |
| Retinopathy | Damage to the blood vessels in the retina, increasing the risk of vision loss. |
| Foot Problems | Increased risk of infections and ulcers due to nerve damage and poor blood flow to the feet. |
Preventative Measures for Type 2 Diabetes
Dietary habits and regular exercise are crucial preventative measures. A diet rich in fruits, vegetables, whole grains, and lean protein, along with limiting processed foods, sugary drinks, and unhealthy fats, is essential for managing weight and blood sugar levels. Regular physical activity, such as brisk walking, swimming, or cycling, helps improve insulin sensitivity and maintain a healthy weight.
Illustrative Cases

Diabetes management is a journey, not a destination. Success stories highlight the power of personalized approaches, emphasizing the importance of lifestyle modifications and consistent medical care. These narratives showcase the potential for positive outcomes and inspire individuals facing similar challenges. Learning from real-life examples can be incredibly motivating and practical for understanding the multifaceted nature of managing type 2 diabetes.Individuals with type 2 diabetes can experience significant improvements in their health and well-being through dedication and commitment.
Success often involves a combination of factors, including dietary changes, regular exercise, stress management techniques, and consistent medication adherence. These examples demonstrate the positive impact that these factors can have on blood sugar control and overall health.
Successful Management Through Lifestyle Changes
Understanding the impact of lifestyle choices is crucial for effective diabetes management. Individuals who successfully manage their condition often experience dramatic improvements in their health through a holistic approach that considers diet, exercise, and stress reduction. For instance, a person might switch to a low-glycemic index diet rich in fruits, vegetables, and whole grains, while also incorporating regular walks or cycling into their routine.
This could be combined with stress-reducing activities like meditation or yoga.
Hypothetical Case Study: Preventing Long-Term Complications
A hypothetical case study can illustrate the importance of blood sugar control in preventing long-term complications. Consider a 50-year-old woman diagnosed with type 2 diabetes. Initially, her blood sugar levels were poorly controlled, leading to elevated HbA1c levels. Over time, she made significant lifestyle changes, including a balanced diet, regular exercise, and stress management. She also worked closely with her healthcare team to adjust her medication regimen.
Subsequently, her blood sugar levels stabilized, and her HbA1c levels significantly improved. This proactive approach helped her avoid potential complications such as nerve damage, kidney disease, and cardiovascular issues. This illustrates how consistent effort in managing blood sugar can prevent long-term health risks.
Table Summarizing Success Stories
| Individual | Key Lifestyle Changes | Outcomes |
|---|---|---|
| Sarah | Low-carb diet, increased physical activity (walking 30 minutes daily), stress-reducing techniques (yoga). | Improved HbA1c levels, reduced blood pressure, increased energy levels. |
| David | Portion control, mindful eating, incorporating more fruits and vegetables, regular strength training sessions. | Stable blood sugar levels, weight loss, reduced risk of cardiovascular disease. |
| Maria | Cooking healthy meals at home, avoiding sugary drinks, regular check-ups with her doctor, medication adherence. | Significant improvement in blood sugar control, improved overall health, reduced medication needs. |
This table highlights different strategies employed by individuals to manage their type 2 diabetes successfully. These examples demonstrate that a combination of approaches can lead to positive outcomes.
Comparing Management Strategies
Comparing different management strategies reveals the importance of tailoring interventions to individual needs. A study could compare the outcomes of a lifestyle-modification-only approach to a strategy combining lifestyle changes with medication. The lifestyle-modification group might experience a significant improvement in blood sugar control, but some individuals might require medication to achieve optimal levels. This demonstrates that a personalized approach that considers individual circumstances is crucial for effective management.
Different approaches might lead to varying outcomes, depending on individual responses to interventions.
Ultimate Conclusion
In conclusion, managing type 2 diabetes involves a multifaceted approach that goes beyond simply understanding insulin and blood sugar. By adopting a holistic lifestyle encompassing diet, exercise, and medication, individuals can effectively manage their condition and prevent long-term complications. This guide has provided a comprehensive overview, from the basics of blood sugar regulation to advanced strategies for long-term management.
Remember, consistent monitoring and proactive lifestyle choices are key to maintaining optimal health.