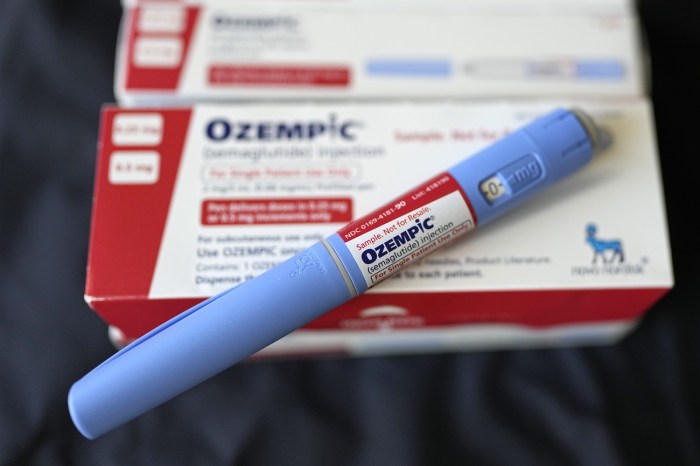
Ozempic impact on kidneys is a crucial area of concern for patients and healthcare professionals alike. This exploration delves into the potential effects of Ozempic on kidney function, examining the science behind its mechanisms, reported cases, and ongoing research. We’ll explore the intricate relationship between Ozempic and kidney health, considering both the potential risks and the importance of careful monitoring.
Understanding the normal functioning of the kidneys is essential to grasping the potential impacts of Ozempic. A detailed look at how kidneys filter blood and remove waste products provides context for potential disruptions. The table comparing typical kidney function with potential Ozempic-related changes will be a key visual tool in this discussion.
Introduction to Ozempic and Kidney Function: Ozempic Impact On Kidneys

Ozempic, a popular medication for weight management, has garnered significant attention for its potential impact on various bodily systems, including the kidneys. Understanding how Ozempic works and the intricate processes of kidney function is crucial for assessing its overall effects. This exploration delves into the mechanism of action of Ozempic, the normal physiology of kidney function, and the existing hypotheses regarding the potential connection between Ozempic and kidney health.Ozempic, a glucagon-like peptide-1 (GLP-1) receptor agonist, works by mimicking the effects of this naturally occurring hormone.
GLP-1 plays a role in regulating blood sugar levels, and Ozempic’s action contributes to lowering blood sugar by stimulating insulin release and suppressing glucagon secretion. This mechanism of action is primarily focused on the pancreas and the endocrine system, but it’s not without potential ripple effects throughout the body.
Ozempic’s Mechanism of Action
Ozempic’s primary action is to regulate blood sugar levels by affecting the pancreas. It does this by binding to GLP-1 receptors on pancreatic beta cells, prompting the release of insulin. This action helps to lower blood glucose levels, which is a core function in managing type 2 diabetes and other metabolic conditions. Additionally, Ozempic slows gastric emptying, which can contribute to feelings of fullness and potentially aid in weight loss.
Normal Physiological Processes Related to Kidney Function
The kidneys are vital organs responsible for filtering waste products from the blood, maintaining electrolyte balance, and regulating blood pressure. They achieve this through a complex filtration process. Blood is filtered through specialized structures called nephrons, which separate waste products and excess water from the blood. The resulting filtrate is then adjusted to maintain optimal fluid and electrolyte balance, and finally, urine is produced and excreted.
This intricate process ensures the body’s internal environment remains stable.
Potential Connection Between Ozempic and Kidney Health
There are emerging hypotheses regarding a potential connection between Ozempic and kidney function. Some studies suggest a possible link between GLP-1 receptor agonists and acute kidney injury, though the precise mechanisms remain under investigation. It’s important to note that further research is needed to fully understand the potential long-term effects of Ozempic on kidney health. The current understanding is that potential effects are primarily short-term and reversible, and further research will clarify the long-term implications.
Comparison of Kidney Functioning with Potential Ozempic Effects
| Kidney Function | Typical Functioning | Potential Changes with Ozempic |
|---|---|---|
| Filtration | Healthy kidneys efficiently filter waste products and excess water from the blood. | Limited data, but some studies suggest a possible slight decrease in filtration rate. Further research is needed to fully understand this potential effect. |
| Electrolyte Balance | Kidneys maintain precise electrolyte levels (e.g., sodium, potassium, calcium) in the blood. | No significant changes are expected based on current understanding. Further studies are necessary. |
| Blood Pressure Regulation | Kidneys play a critical role in regulating blood pressure by producing hormones and adjusting fluid balance. | Some studies suggest a potential correlation with changes in blood pressure, but this needs further investigation. |
| Waste Removal | Kidneys effectively remove waste products from the blood, ensuring a healthy internal environment. | No significant expected changes based on current knowledge. |
Reported Effects of Ozempic on Kidneys
Ozempic, a popular weight-loss medication, has garnered significant attention for its potential impact on various bodily systems. While generally well-tolerated, there are reported instances of kidney-related issues linked to its use. This section delves into the documented cases, potential adverse effects, and risk factors associated with Ozempic and kidney function.Ozempic’s mechanism of action involves influencing various hormonal pathways, including those related to glucose regulation.
This complex interplay can potentially affect kidney function, though the precise nature of this relationship is still under investigation. The observed effects are not universally consistent and further research is crucial to fully understand the potential risks and protective factors.
Documented Cases of Kidney-Related Issues
While extensive research is ongoing, isolated reports of kidney problems in patients taking Ozempic exist. These cases are often reported through post-marketing surveillance and clinical trials, with detailed analyses still being conducted to establish causal relationships. The nature and severity of these reported issues vary considerably, making it difficult to draw definitive conclusions.
Potential Adverse Effects on Kidney Function
Ozempic, like other medications, may have potential adverse effects on kidney function. These can range from mild to more serious, requiring careful monitoring. Some potential effects include changes in kidney function tests (such as creatinine or blood urea nitrogen levels), and in severe cases, acute kidney injury. It’s essential to note that the reported incidences of these effects remain relatively low, and the exact nature of the connection between Ozempic and kidney problems continues to be explored.
While Ozempic’s impact on kidneys is a hot topic, it’s crucial to understand the connection to other health concerns. For instance, a deeper dive into how high blood pressure is diagnosed could reveal a significant interplay. Understanding all about hypertension diagnosis is vital for fully grasping the complexities of Ozempic’s effect on kidney function. Ultimately, more research is needed to pinpoint the precise mechanisms involved, and we need to keep an eye on this evolving area of medical knowledge.
Potential Kidney-Related Side Effects Table
| Side Effect | Frequency | Severity |
|---|---|---|
| Changes in Kidney Function Tests (e.g., elevated creatinine or blood urea nitrogen) | Potentially rare, but reported | Mild to moderate |
| Acute Kidney Injury | Rare | Moderate to severe; may require hospitalization |
| Chronic Kidney Disease (potential long-term effect) | Uncertain, long-term studies needed | Potential severe |
The table above provides a general overview. Exact frequency and severity data are still being collected and analyzed. Consult with a healthcare professional for personalized risk assessment.
Risk Factors for Kidney Problems in Ozempic Users
Several factors might increase the risk of kidney problems in patients taking Ozempic. These factors include a pre-existing history of kidney disease or conditions that can negatively affect kidney function, such as diabetes or high blood pressure. Patients with a family history of kidney disease or those who have experienced kidney problems in the past should be particularly vigilant and communicate these concerns with their doctors.
Age and overall health also play a role, and individuals with these factors should closely monitor their kidney health.
While the Ozempic impact on kidneys is a growing concern, it’s crucial to remember that maintaining overall health is key. One way to support your well-being, and potentially reduce the risk of fainting spells, is by practicing proper hydration and healthy lifestyle choices. Knowing how to prevent fainting can be a valuable tool in managing potential side effects related to Ozempic.
For a deeper dive into this crucial topic, check out our helpful guide on how to prevent fainting. Ultimately, understanding Ozempic’s potential impact on the kidneys requires a holistic approach to health, and preventative measures are important to consider.
Studies and Research on Ozempic and Kidney Impact
Unraveling the connection between Ozempic and kidney health is crucial for informed decision-making. While the drug has shown promise for weight management and other metabolic benefits, understanding its potential impact on kidney function is paramount. This section delves into the types of studies examining this relationship, presents their findings, and highlights the limitations of current research.The research landscape surrounding Ozempic and kidney function is constantly evolving.
Emerging data sheds light on potential risks and benefits, but further investigation is needed to definitively establish the long-term effects.
Types of Studies Investigating Ozempic and Kidney Function
A variety of study designs have been employed to investigate the relationship between Ozempic and kidney function. These include observational studies, which analyze existing patient data, and clinical trials, which involve controlled experiments. The methodologies employed in these studies significantly impact the conclusions that can be drawn.
Methodology and Key Results of Studies
The following table summarizes various studies examining the impact of Ozempic on kidney function, categorized by study type, methodology, and key results. Note that the results are diverse, highlighting the complexity of the relationship.
| Study Type | Methodology | Key Results |
|---|---|---|
| Observational Studies | Analysis of large patient databases, often tracking patients receiving Ozempic over time. Some studies might compare outcomes between those on Ozempic and those not. | Some observational studies suggest a potential association between Ozempic use and a slight increase in certain kidney markers (e.g., creatinine levels). However, these associations do not always translate to clinically significant kidney damage. |
| Clinical Trials | Controlled experiments with a treatment group receiving Ozempic and a control group receiving a placebo or another treatment. These trials often monitor kidney function parameters over a defined period. | Results from clinical trials are less conclusive. Some show no discernible impact on kidney function, while others have noted minor changes in kidney markers, but without evidence of significant harm. The variability in findings may be related to differing trial designs, patient populations, and durations of treatment. |
| Animal Studies | Research conducted on animals to explore the effects of Ozempic on kidney function in a controlled setting. | Some animal studies suggest potential kidney effects, although the extent to which these effects translate to humans is unclear. Animal models may not fully replicate human physiology. |
Comparison of Results Across Different Studies
A key challenge in interpreting the research is the variability in results across different studies. Factors like the study population, the duration of treatment, and the specific methods used for measuring kidney function can influence the observed outcomes. Further, the sample sizes in some studies may be insufficient to draw definitive conclusions. Studies with larger sample sizes and longer follow-up periods are crucial to address these limitations.
Limitations of Existing Research
Existing research on Ozempic and kidney impact faces several limitations. Observational studies, while valuable for identifying potential associations, cannot definitively establish cause-and-effect relationships. Clinical trials, though more rigorous, often have limitations in patient populations and study duration, making it challenging to fully understand the long-term consequences of Ozempic use. Furthermore, the complex interplay of other factors, such as pre-existing medical conditions, can complicate the interpretation of findings.
This highlights the importance of further, well-designed research to address these limitations.
Potential Mechanisms Linking Ozempic and Kidney Issues
Ozempic, a popular medication for weight management and type 2 diabetes, has sparked some concern regarding potential kidney effects. While the overall safety profile remains positive, understanding the potential mechanisms connecting Ozempic to kidney issues is crucial for further research and patient management. Investigating these pathways is vital to differentiate between potential side effects and genuine causal relationships.The exact mechanisms by which Ozempic might impact kidney function are still being explored.
However, several potential pathways have been identified, and ongoing research is aiming to confirm or refute these hypotheses. This exploration is critical to provide a more complete understanding of Ozempic’s potential impact on kidney health and to ensure the responsible use of this medication.
Potential Physiological Pathways
Several physiological pathways could potentially link Ozempic to kidney-related issues. These pathways are complex and interconnected, making it challenging to isolate specific effects. Understanding the nuances of these processes is critical to understanding the potential impact of Ozempic on kidney health.
- GLP-1 Receptor Activation and Renal Hemodynamics: Ozempic’s primary mechanism involves activating the glucagon-like peptide-1 (GLP-1) receptor. This activation can influence renal blood flow and glomerular filtration rate. Increased GLP-1 activity might either enhance or reduce renal blood flow, depending on the specific circumstances and the individual’s baseline kidney function. For example, in some individuals, this could potentially lead to changes in blood pressure and subsequent alterations in kidney filtration processes.
This could be especially relevant for individuals with pre-existing kidney conditions.
- Sodium and Water Balance: GLP-1 can affect the balance of sodium and water within the body. Changes in sodium and water retention could indirectly affect kidney function, potentially contributing to conditions such as acute kidney injury (AKI). For instance, in cases where Ozempic usage is combined with other medications affecting sodium and water balance, this effect could be amplified.
- Glomerular Filtration Rate and Proteinuria: Ozempic’s potential effects on glomerular filtration rate (GFR) and proteinuria warrant careful consideration. A decrease in GFR, or the rate at which blood is filtered by the kidneys, could be a marker of potential kidney damage. Similarly, elevated proteinuria, the presence of proteins in the urine, could indicate kidney dysfunction. This highlights the importance of ongoing monitoring of kidney function during Ozempic therapy.
Alternative Hypotheses
While the mechanisms discussed above are plausible, alternative explanations for potential kidney issues associated with Ozempic use also exist. These alternative factors need careful consideration.
- Pre-existing Conditions: Individuals with pre-existing kidney conditions or other underlying health issues may be more susceptible to adverse kidney effects, regardless of Ozempic use. This highlights the need for careful patient selection and monitoring.
- Co-medications: The concurrent use of Ozempic with other medications, particularly those affecting kidney function, could potentially exacerbate any existing kidney problems or induce new ones. This underscores the importance of thorough medication history assessment.
- Individual Variability: Individual responses to Ozempic therapy can vary significantly. This emphasizes the importance of personalized medicine approaches, tailoring treatment plans to individual patient characteristics and needs.
Illustrative Diagram (Conceptual)
(Note: A diagram cannot be displayed here, but a conceptual diagram would illustrate the interconnected pathways mentioned above. It would show GLP-1 receptor activation leading to changes in renal blood flow, sodium and water balance, and GFR. Arrows would indicate the potential directions of these effects, with feedback loops representing the complex interplay between these factors.)
Clinical Considerations and Recommendations
Ozempic, a popular medication for weight management and type 2 diabetes, has shown promising results in many patients. However, like any medication, it’s crucial to understand potential side effects and take proactive steps to mitigate risks. This section focuses on the clinical considerations and recommendations surrounding Ozempic’s impact on kidney function, emphasizing preventative measures and monitoring guidelines.Careful monitoring of kidney function is essential for patients using Ozempic.
This proactive approach helps identify potential issues early and allows for timely intervention. Early detection and management of kidney problems can significantly improve patient outcomes.
Monitoring Kidney Function
Regular kidney function tests are crucial for patients taking Ozempic. These tests, typically involving blood creatinine and estimated glomerular filtration rate (eGFR) measurements, provide valuable insights into the health of the kidneys. The frequency of these tests should be determined by individual patient risk factors and the overall clinical picture. Patients with pre-existing kidney conditions, or those exhibiting symptoms of kidney problems, may need more frequent monitoring.
Importance of Regular Kidney Function Tests, Ozempic impact on kidneys
Regular kidney function tests allow for early detection of any potential kidney issues related to Ozempic use. Early identification of developing problems enables prompt interventions and mitigates potential long-term complications. This proactive approach helps to maintain overall kidney health and reduces the risk of adverse events. For instance, if a patient experiences a sudden decline in eGFR, prompt intervention could prevent irreversible kidney damage.
Recommended Course of Action if Kidney-Related Issues Arise
If kidney-related issues arise in patients on Ozempic, it’s essential to immediately consult a healthcare provider. The healthcare provider will evaluate the patient’s specific situation, considering factors such as pre-existing conditions and the severity of the issue. This assessment will guide the course of action, which might include adjusting the Ozempic dosage, temporarily suspending the medication, or initiating alternative treatments.
Close monitoring and adjustments to the treatment plan are crucial to managing the kidney-related issue effectively.
While Ozempic’s impact on the kidneys is a subject of ongoing research, some studies suggest potential links to kidney problems. This is important to consider, especially when you’re looking at the wider picture of potential health issues, like gastroesophageal reflux disease GERD, which can be impacted by various factors, including medications. Ultimately, more research is needed to fully understand the complete effect of Ozempic on kidney function.
Gastroesophageal reflux disease GERD can be tricky to manage, and it’s always best to discuss any concerns with a doctor. Understanding the full scope of the possible side effects of Ozempic on the kidneys is important for informed decision-making.
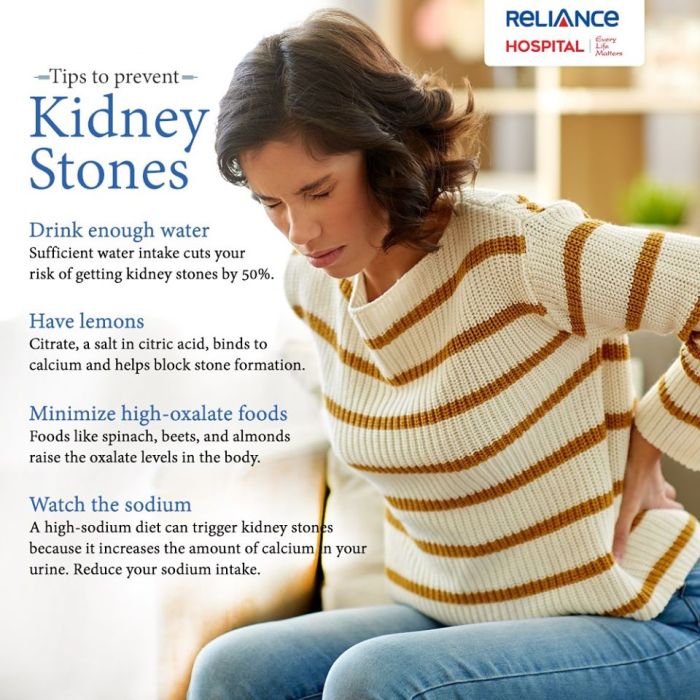
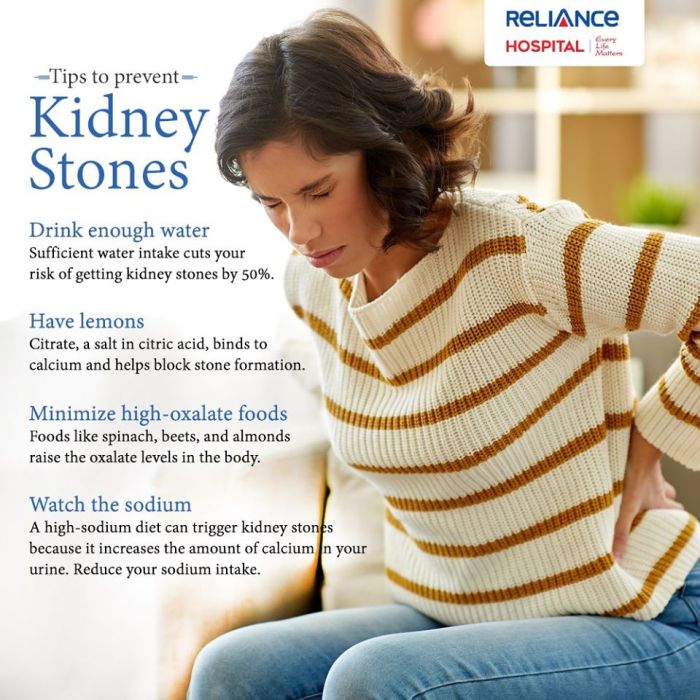
Preventative Measures
Healthcare providers can recommend several preventative measures to patients taking Ozempic. These measures focus on lifestyle modifications and close monitoring to reduce the risk of kidney complications.
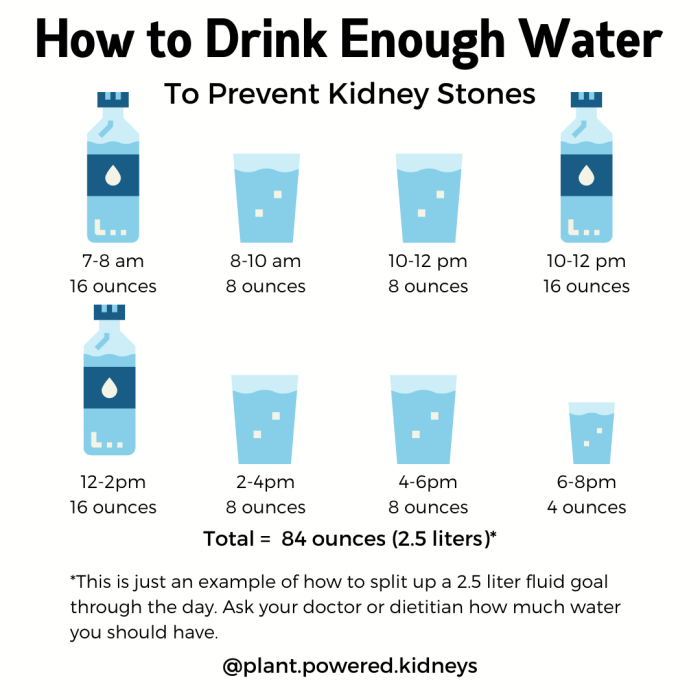
- Maintaining a healthy lifestyle: Encouraging a balanced diet, regular exercise, and adequate hydration are vital preventative steps. These lifestyle modifications contribute to overall health and support kidney function. Patients should be educated on the importance of these practices and receive personalized guidance tailored to their individual needs.
- Regular monitoring of blood pressure and blood sugar: Controlling blood pressure and blood sugar levels is crucial in preventing kidney damage. Consistent monitoring and management of these factors can significantly reduce the risk of complications associated with Ozempic use.
- Prompt reporting of any symptoms: Patients should be encouraged to report any unusual symptoms, such as changes in urine output, swelling, or persistent fatigue, to their healthcare providers immediately. This prompt communication enables early intervention and appropriate management of potential issues.
Patient Perspective on Ozempic and Kidney Health
Ozempic, a popular weight-management medication, has generated significant interest and concern regarding its potential impact on kidney function. Patients understandably want clear, accessible information about this connection. This section delves into common patient concerns, resources for learning more, and how to communicate effectively with healthcare providers.Patients often have legitimate questions and anxieties regarding the potential risks of Ozempic to their kidney health.
This includes a need for reassurance about their personal risk factors and the overall safety of the medication. These concerns are valid and require careful consideration and open dialogue with healthcare professionals.
Common Patient Concerns Regarding Ozempic and Kidney Function
Patients frequently grapple with uncertainties about the potential for kidney problems when using Ozempic. Understanding these concerns is crucial for effective communication and support.
“Is Ozempic safe for my kidneys?” “Will using Ozempic cause kidney damage?” “What are the specific risks for me?”
These concerns stem from the relatively new nature of the medication and the complexities of its effects on the body. Patients want to know the extent of the potential risks and how they personally fit into the picture.
Resources for Patients Seeking Information
Patients seeking reliable information about Ozempic and kidney health have several options. These include reputable medical organizations, scientific journals, and direct communication with their healthcare providers.
- Medical Organizations: Organizations like the National Kidney Foundation (NKF) and the American Diabetes Association (ADA) offer detailed information on kidney health, including potential risks and preventative measures. These resources provide valuable background knowledge and practical guidance.
- Scientific Publications: Medical journals often publish research studies on the effects of Ozempic on various bodily systems, including the kidneys. While these can be more technical, they provide deeper insights into the underlying science.
- Healthcare Providers: Open and honest communication with healthcare providers is crucial. Patients should feel empowered to ask questions, express concerns, and seek clarification regarding their specific situation.
Discussing Kidney Health Concerns with Healthcare Providers
Effective communication with healthcare providers is vital for addressing concerns about Ozempic and kidney health. Patients should be proactive in discussing their anxieties and risk factors.
- Prepare Questions in Advance: Listing questions beforehand can help patients feel more prepared and confident during their consultations. This includes asking about their individual risk factors and specific concerns.
- Maintain an Open Dialogue: Encourage open and honest conversations with healthcare providers. This includes asking for clarification on any points that are unclear.
- Document Conversations: Patients should keep records of their conversations, including dates, topics discussed, and any recommendations made. This provides valuable reference material and aids in tracking progress.
Illustrative Examples of Kidney Function
Healthy kidneys are vital for overall well-being, acting as sophisticated filters for the blood. They remove waste products and excess fluids, maintaining a balanced internal environment. Understanding their function is crucial to appreciating the potential impact of medications like Ozempic on kidney health.
A Healthy Kidney: A Functional Filter
The kidneys, bean-shaped organs located on either side of the spine, receive a constant supply of blood. This blood is filtered through specialized structures called nephrons. Each nephron contains a glomerulus, a network of capillaries where blood pressure forces water and waste products into a filtering space called Bowman’s capsule. This filtrate is then further refined as it passes through intricate tubules within the nephron.
Nutrients are reabsorbed into the bloodstream, while waste products and excess water are collected and expelled as urine. This process maintains the delicate balance of electrolytes and fluids in the body.
A Potential Scenario of Impaired Kidney Function
A potential scenario of impaired kidney function, potentially linked to Ozempic use, could involve damage to the glomeruli. The glomeruli are the initial filtration units in the nephrons. In some cases, Ozempic might contribute to inflammation or reduced blood flow within these capillaries, impacting the glomeruli’s ability to effectively filter waste products. This could lead to a buildup of waste products in the blood, putting a strain on other organs and potentially causing various complications.
- Reduced glomerular filtration rate (GFR): A key indicator of kidney function, GFR measures how much blood the kidneys filter per minute. A decline in GFR indicates reduced filtration capacity, a potential early sign of kidney impairment.
- Proteinuria: This refers to the presence of excessive protein in the urine. Healthy kidneys normally prevent protein from being excreted. Proteinuria can be a sign of damage to the glomeruli, indicating impaired filtration function.
- Inflammation in kidney tissues: Inflammation, potentially triggered by Ozempic, can affect the delicate structures of the nephrons, interfering with their ability to perform their filtering function. This inflammation could manifest as swelling and pain in the kidneys.
How a Healthy Kidney Processes Blood
A healthy kidney meticulously processes blood, acting as a complex filter system. The process begins with blood entering the glomerulus, a network of capillaries within each nephron. High blood pressure forces water, electrolytes, and waste products from the blood into Bowman’s capsule, forming filtrate. The filtrate then travels through a series of tubules where crucial substances like glucose, amino acids, and essential electrolytes are reabsorbed into the bloodstream, maintaining homeostasis.
Waste products and excess water are collected and concentrated to form urine, which is then expelled from the body. This intricate process ensures the removal of harmful substances and maintains the body’s delicate chemical balance.
A Depiction of Potential Impact on Kidney Structures
Imagine a sieve with very fine holes. This sieve represents a healthy glomerulus. Tiny particles, representing waste products, easily pass through the holes. Now, imagine the sieve becoming slightly clogged or the holes getting smaller. This represents a potential impact of Ozempic on the glomeruli, hindering the efficient filtration of waste products.
The clogging or narrowing of the sieve reduces the ability to filter waste, leading to a buildup of these substances in the bloodstream. This reduced filtering capacity can eventually lead to kidney damage.
Conclusion
In conclusion, the relationship between Ozempic and kidney health requires careful consideration. While the potential for adverse kidney effects is a subject of ongoing research, understanding the mechanisms, reported cases, and clinical guidelines is critical. Patients and healthcare providers must work together to ensure proper monitoring and preventative measures. The exploration of patient perspectives and the importance of open communication will be crucial in navigating this complex area.