Signs of dehydration in kids sets the stage for a crucial conversation about recognizing and responding to this potentially serious condition. Knowing the early indicators is key to preventing more severe complications. This guide delves into the various signs, from mild to severe, across different age groups, offering actionable insights into assessing hydration status and initiating appropriate treatment.
From subtle changes in behavior to more noticeable symptoms, understanding the nuances of dehydration in infants, toddlers, and preschoolers is paramount. We’ll explore the causes, the severity levels, and ultimately, how to protect your child from the risks associated with dehydration.
Introduction to Dehydration in Kids
Dehydration in children occurs when the body loses more fluids than it takes in. This loss can be due to various factors, and it’s crucial to understand the signs and severity to ensure prompt treatment. Recognizing the early signs of dehydration is vital to preventing serious complications. Untreated dehydration can lead to significant health issues, ranging from mild discomfort to life-threatening conditions.
Understanding the causes and types of dehydration is essential for parents and caregivers to protect their young children.
Understanding the Importance of Early Recognition
Early recognition of dehydration is key to effective intervention. Delaying treatment can exacerbate the condition, potentially leading to serious health problems. Prompt action based on observable signs can prevent further complications.
Common Causes of Dehydration in Young Children
Young children are particularly susceptible to dehydration due to their smaller body size and higher metabolic rates. Several factors contribute to this vulnerability. Infants and toddlers may not be able to communicate their thirst effectively, making it harder to identify dehydration early. Increased activity levels, especially during hot weather, can lead to significant fluid loss. Certain illnesses, like diarrhea and vomiting, can rapidly deplete fluid reserves.
Other contributing factors include fever, burns, and excessive sweating.
Keeping an eye out for dehydration signs in kids is crucial. Dry mouth and sunken eyes are common indicators, but did you know that some home remedies for kidney stones, like drinking plenty of water, can actually help prevent dehydration? Home remedies for kidney stones often involve increasing fluid intake, which is vital for overall health and preventing dehydration in children.
So, next time you’re concerned about your child’s hydration, remember these simple yet important signs.
Types of Dehydration
Understanding the different levels of dehydration is crucial for appropriate treatment. The severity of dehydration can vary, impacting the child’s overall health.
| Type | Description | Symptoms | Treatment |
|---|---|---|---|
| Mild | Mild dehydration occurs when the body loses a small amount of fluid, typically due to mild to moderate fluid loss through normal activities, or mild diarrhea/vomiting. | Mild symptoms include decreased urination, dry mouth, mild thirst, and a slight decrease in energy levels. | Treatment involves increasing fluid intake, such as offering clear fluids like water, clear broths, or oral rehydration solutions. Monitoring the child’s condition is important. |
| Moderate | Moderate dehydration occurs when the body loses a significant amount of fluid, resulting in more severe symptoms than mild dehydration. This can occur due to prolonged or severe vomiting, diarrhea, or fever. | Symptoms include sunken eyes, decreased skin turgor (skin doesn’t bounce back quickly), rapid pulse, dry mouth, and difficulty urinating. | Treatment requires immediate medical attention. Oral rehydration solutions or intravenous fluids may be necessary to restore fluid balance. |
| Severe | Severe dehydration is a life-threatening condition where the body loses a substantial amount of fluid, often accompanied by severe symptoms. This can result from prolonged or severe vomiting, diarrhea, or fever, or a combination of these factors. | Severe symptoms include sunken eyes, extremely dry mouth, decreased skin turgor (skin doesn’t bounce back), rapid pulse, low blood pressure, difficulty breathing, and altered mental status. | Severe dehydration necessitates immediate medical attention and hospitalization. Intravenous fluids are crucial to rapidly restore fluid and electrolyte balance. |
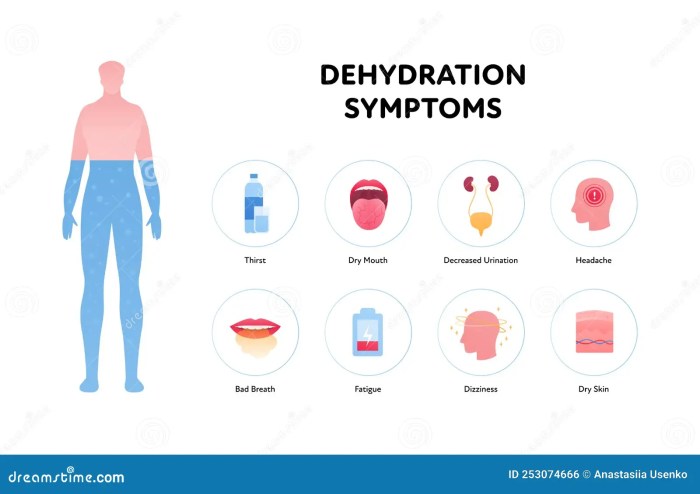
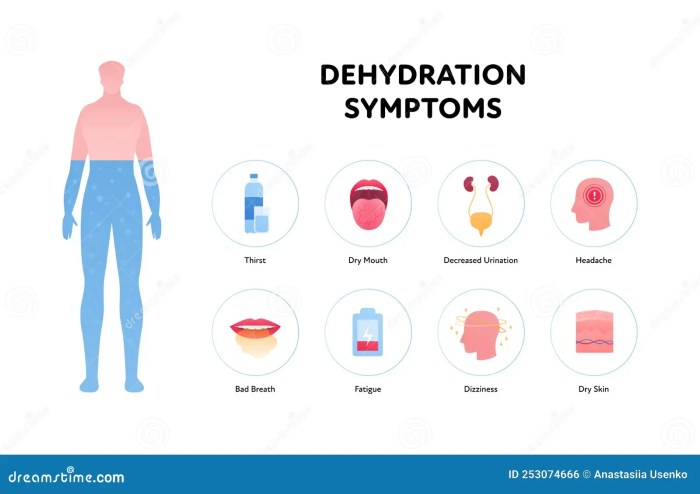
Identifying Early Signs of Dehydration

Recognizing the early signs of dehydration in children is crucial for prompt intervention. Dehydration can quickly progress from mild discomfort to a serious medical concern if not addressed. Understanding the specific signs and symptoms associated with different age groups can significantly improve response time and prevent complications. This knowledge empowers parents and caregivers to take appropriate action when a child shows signs of dehydration.
Identifying Dehydration in Infants
Infants, due to their smaller size and immature kidneys, are particularly vulnerable to dehydration. Early detection is vital. Key indicators include a dry mouth and tongue, a sunken fontanel (the soft spot on the top of the head), fewer wet diapers than usual, and lethargy or irritability. Noticeable changes in their usual activity level can also indicate dehydration.
These changes might include decreased responsiveness to stimuli or a general lack of interest in their surroundings.
Identifying Dehydration in Toddlers
Toddlers, as they become more mobile and explore their environment, may exhibit similar signs to infants. Look for decreased urination, dry mouth, and a general lack of energy. They may also display crankiness or fussiness, which might be mistaken for other issues. A noticeable change in their normal behaviour is a significant indicator. For example, a toddler who is usually very active might become lethargic and less interested in playing.
Identifying Dehydration in Preschool-Aged Children
Preschool-aged children, as they develop more complex communication skills, may exhibit more obvious signs of dehydration. These children can express feelings of thirst or discomfort, and may complain of headaches or dizziness. Along with these verbal cues, observe for dry mouth, decreased urination, and fatigue. A noticeable change in their typical behaviour is an important indicator of dehydration.
For instance, a child who is normally very playful might become withdrawn or irritable.
Differentiating Dehydration from Other Illnesses
Dehydration can mimic other illnesses, making accurate diagnosis challenging. Important factors to consider include the child’s overall health history, recent illnesses, and the presence of any other symptoms. For instance, vomiting and diarrhea, common symptoms of several illnesses, can also be indicators of dehydration. Fever, coughing, or a runny nose might be present alongside dehydration, making the distinction even more difficult.
Careful observation and a detailed history of symptoms are essential for differentiating dehydration from other conditions.
Comparing Signs of Dehydration Across Age Groups
| Age Group | Signs | Severity | Additional Notes |
|---|---|---|---|
| Infants | Sunken eyes, dry mouth, fewer wet diapers, lethargy, irritability, decreased activity, sunken fontanel | Mild to Moderate | Infants may not express thirst verbally. |
| Toddlers | Decreased urination, dry mouth, crankiness, fussiness, lethargy, decreased activity | Mild to Moderate | Toddlers might exhibit irritability or fussiness instead of clear verbal complaints. |
| Preschoolers | Dry mouth, decreased urination, fatigue, verbal complaints (thirst, headache, dizziness), irritability, loss of appetite | Mild to Severe | Preschoolers can communicate their thirst, which provides an important clue. |
Warning Signs Requiring Immediate Medical Attention
A rapid heartbeat, difficulty breathing, confusion, or seizures are critical warning signs that necessitate immediate medical attention. Any child exhibiting these symptoms should be taken to the nearest emergency room. In these situations, speed is critical to preventing serious complications. Rapid treatment is essential to help avoid any lasting health issues.
Assessing Hydration Status
Knowing how to assess a child’s hydration status is crucial for early intervention and preventing serious complications. Accurate assessment allows parents and caregivers to understand the severity of dehydration and take appropriate action, potentially preventing further health deterioration. This involves recognizing the subtle signs and employing practical methods to evaluate a child’s overall hydration level.Proper hydration is vital for a child’s overall health and well-being.
It supports bodily functions, regulates temperature, and plays a key role in nutrient absorption and waste elimination. A comprehensive approach to hydration assessment involves not just observing physical signs but also considering the child’s behavior and medical history.
Methods for Assessing Hydration Level, Signs of dehydration in kids
Several methods are available for assessing a child’s hydration level. These methods range from simple observations to more detailed physical examinations. Understanding these different approaches allows caregivers to choose the most appropriate method based on the specific situation and available resources.
- Observation of Skin Turgor: Assessing skin turgor involves gently pinching the skin on the back of the hand or the forehead. Normal skin will quickly return to its original position. Delayed return or tenting of the skin (the skin remaining pinched) suggests dehydration. This method is a quick and readily available assessment tool.
- Monitoring Urine Output: The volume and color of urine provide valuable clues about hydration. A decrease in urine output or dark-colored urine (concentrated) indicates potential dehydration. Conversely, a large amount of pale yellow urine suggests adequate hydration. The frequency of urination should also be observed, and a reduced frequency may suggest dehydration. It’s essential to remember that urine color and output can vary based on diet and other factors.
- Measuring Weight: Monitoring weight changes over time can be an indicator of hydration status. A significant weight loss, especially in conjunction with other symptoms, can point towards dehydration. However, this method requires consistent weighing to detect subtle changes.
- Evaluation of Blood Electrolytes: Blood tests to assess electrolytes like sodium and potassium are more advanced methods used in healthcare settings. These tests can provide a precise measure of electrolyte imbalances, which are often associated with dehydration. Such tests are important for severe dehydration or when other assessments are inconclusive.
Flowchart for Assessing Dehydration
This flowchart provides a structured approach to assessing dehydration: 
(Note: This is a placeholder for an image. A flowchart illustrating the steps for assessing dehydration would be included here.)
Comparing and Contrasting Methods
Different methods for monitoring hydration have varying levels of invasiveness and accuracy. Skin turgor is a simple, non-invasive method, but its accuracy can be affected by factors like skin elasticity. Urine output is readily available and provides information about the kidneys’ function, but it’s influenced by factors like diet. Weight monitoring is a more objective measure, but it requires consistent tracking.
Blood tests offer the most precise results but are more invasive and require medical intervention.
Keeping an eye out for dehydration signs in kids is crucial. Sunken eyes, dry mouth, and decreased urine output are all telltale indicators. It’s important to remember that certain exercises, like those that could exacerbate sciatica pain, exercises that could worsen sciatica , can also affect hydration levels. So, while keeping an eye out for these classic dehydration symptoms is key, remember that other factors could play a role.
Importance of Observing a Child’s Behavior
A child’s behavior can be a crucial indicator of dehydration. Signs such as excessive sleepiness, irritability, or lethargy can point to a problem. A decrease in activity level and lack of interest in usual activities are also warning signs.
Normal vs. Abnormal Hydration Signs
Normal hydration signs include moist mucous membranes (the linings of the mouth and nose), a normal skin turgor (the skin springs back quickly), and appropriate urine output. Abnormal hydration signs include dry mucous membranes, slow return of skin turgor (skin stays pinched), decreased urine output, and lethargy or irritability.
Evaluating Hydration Based on Symptoms
| Symptom | Possible Hydration Level | Next Steps |
|---|---|---|
| Dry mouth, decreased urine output, sunken eyes | Moderate to severe dehydration | Seek immediate medical attention |
| Decreased activity, irritability, lethargy | Mild to moderate dehydration | Increase fluid intake, monitor for worsening symptoms |
| Normal skin turgor, moist mucous membranes, adequate urine output | Adequate hydration | Continue with normal care |
| Sunken fontanelle (soft spot on the head), rapid heartbeat, weak pulse | Severe dehydration | Seek immediate medical attention |
Treating Dehydration
Treating dehydration in children promptly is crucial for restoring their health and preventing complications. Early intervention is key, and understanding the appropriate home care for mild cases is essential. Following these steps can help you effectively manage mild dehydration at home, but remember that medical intervention might be necessary depending on the severity of the symptoms.
Initial Steps for Home Treatment of Mild Dehydration
Addressing mild dehydration at home involves several crucial initial steps. These actions focus on replenishing lost fluids and electrolytes. Immediate action is important to prevent further dehydration and potential complications.
- Encourage frequent small sips of fluids: Instead of forcing large amounts of liquid at once, encourage your child to take small sips of fluids frequently. This approach helps them gradually absorb the necessary fluids and electrolytes without feeling overwhelmed or uncomfortable.
- Choose appropriate fluids: Offer fluids that are readily absorbed and won’t upset the stomach, such as clear broths, diluted fruit juices (1 part juice to 4 parts water), or electrolyte drinks (especially those formulated for children). Avoid sugary drinks or caffeine-containing beverages, which can worsen dehydration.
- Monitor for improvement: Observe your child’s symptoms and note any improvement. Pay attention to the frequency of urination and the overall improvement in their energy levels. If the symptoms worsen or don’t improve within a few hours, seek medical attention.
Importance of Oral Rehydration Solutions
Oral rehydration solutions (ORS) are specially formulated electrolyte solutions designed to effectively replace lost fluids and electrolytes. These solutions are crucial for replenishing essential minerals like sodium, potassium, and chloride, which are lost through dehydration. ORS are often more effective than plain water alone in treating mild dehydration, as they provide the necessary electrolytes in a balanced ratio.
Administering Oral Rehydration Solutions
Administering ORS correctly is essential for effective treatment. Follow these steps to ensure your child receives the necessary fluids and electrolytes:
- Follow package instructions: Carefully follow the instructions on the ORS package for the correct dilution and dosage. These instructions are critical to ensure proper electrolyte balance and to avoid potential complications.
- Start with small amounts: Begin with small sips or small amounts of the ORS solution, gradually increasing the amount as tolerated. This approach is important to avoid upsetting the child’s stomach.
- Give frequently: Offer the ORS solution frequently throughout the day to replace lost fluids and electrolytes effectively. The frequency should be adjusted based on the child’s needs and tolerance.
When Medical Intervention Is Necessary
Medical intervention for dehydration is crucial when the child’s condition worsens or doesn’t improve with home treatment. Seek immediate medical attention if any of the following symptoms appear:
- Severe dehydration symptoms: These include sunken eyes, decreased urine output, rapid heartbeat, and lethargy. These signs indicate a severe level of dehydration requiring immediate medical attention.
- Persistent vomiting or diarrhea: If the vomiting or diarrhea persists despite home treatment, seeking medical care is crucial. This is because these conditions can quickly lead to severe dehydration.
- Signs of shock: These include pale or bluish skin, cold and clammy skin, rapid breathing, and decreased consciousness. These signs signify a severe and potentially life-threatening condition requiring immediate medical intervention.
Safe and Effective Home Remedies for Mild Dehydration
Several safe and effective home remedies can support mild dehydration, but they should not replace oral rehydration solutions. These options can complement ORS in milder cases.
- Clear broths: Clear broths, such as chicken or vegetable broth, can help replace lost fluids and electrolytes. These are generally well-tolerated and readily absorbed by the body.
- Diluted fruit juices: Diluted fruit juices (1 part juice to 4 parts water) can be a good option for children who tolerate them well. The high sugar content in concentrated juices can worsen the dehydration, so dilution is essential.
Fluids to Avoid
Avoid certain fluids that can hinder the rehydration process or worsen the condition.
- Sugary drinks: Sugary drinks like soda, juice (especially concentrated), and sweetened beverages can actually draw fluids from the body’s tissues, hindering the rehydration process.
- Caffeinated drinks: Caffeine is a diuretic, meaning it can increase urination and worsen dehydration. Avoid caffeinated beverages like coffee, tea, and energy drinks.
Preventing Dehydration
Keeping your child hydrated is crucial for their overall health and well-being, especially during hot weather or when they are sick. Proper hydration supports various bodily functions, from regulating temperature to transporting nutrients. Preventing dehydration is much easier than treating it, and proactive measures can significantly reduce the risk of this condition.Preventing dehydration involves understanding the factors that contribute to it and implementing strategies to maintain optimal fluid balance.
This includes recognizing the importance of adequate fluid intake, the role of diet, and monitoring fluid intake during illness. This section will Artikel key strategies to keep your child hydrated and healthy.
Tips for Preventing Dehydration in Children
Understanding the importance of proper hydration is the first step in preventing dehydration. Maintaining adequate fluid intake is essential for a child’s health and well-being. A well-hydrated child is better equipped to handle daily activities and illnesses.
- Offer water frequently throughout the day, especially during hot weather or physical activity. Avoid sugary drinks, which can have a diuretic effect, leading to fluid loss.
- Encourage frequent sips of water, even when not thirsty. This is particularly important for infants and toddlers who may not readily communicate their thirst.
- Incorporate hydrating foods into the diet. Fruits and vegetables with high water content, such as watermelon, cucumbers, and oranges, contribute to overall hydration.
- Provide electrolyte-rich fluids, like diluted fruit juices or sports drinks, during prolonged physical activity or when a child is losing fluids due to illness.
Importance of Maintaining Proper Fluid Intake
Proper fluid intake is essential for maintaining a child’s overall health. Dehydration can negatively impact various bodily functions, leading to fatigue, reduced cognitive performance, and impaired physical activity.
Adequate hydration ensures that the body can effectively regulate temperature, transport nutrients, and eliminate waste products. A well-hydrated child is more likely to thrive and participate in daily activities without experiencing discomfort or reduced performance.
Role of Diet in Preventing Dehydration
Diet plays a significant role in maintaining a child’s hydration levels. Certain foods and drinks can contribute to fluid balance, while others may have a diuretic effect.
- Incorporate hydrating foods into the daily diet. Fruits and vegetables high in water content, such as cucumbers, watermelon, and oranges, are excellent sources of hydration. These foods contribute to overall fluid intake and provide essential vitamins and minerals.
- Limit sugary drinks and juices, as they can have a diuretic effect, leading to increased fluid loss. Opt for water, milk, and diluted fruit juices as better alternatives.
Monitoring Fluid Intake During Illness
Monitoring a child’s fluid intake during illness is crucial to prevent dehydration. Illnesses, such as vomiting and diarrhea, can lead to significant fluid loss, increasing the risk of dehydration.
Keeping an eye out for dehydration signs in kids is crucial. Sunken eyes, dry mouth, and decreased urine output are all telltale indicators. While focusing on hydration is key, did you know that incorporating natural remedies like lemon balm can also contribute to overall well-being? The health benefits of lemon balm might offer a gentle way to support a healthy immune system and potentially aid in digestion, which can indirectly support a child’s hydration.
Ultimately, recognizing and addressing dehydration promptly is essential for maintaining a child’s health and vitality.
Observing the amount of fluids a child consumes and any signs of fluid loss is vital. Adjusting fluid intake based on the child’s specific needs and the severity of the illness is essential for preventing dehydration complications.
Activities Increasing Risk of Dehydration
Certain activities can increase the risk of dehydration in children. Understanding these activities helps in implementing preventive measures.
- Prolonged exposure to hot weather, especially during outdoor activities, can lead to excessive sweating and fluid loss.
- Vigorous physical activity, such as sports or playtime, increases perspiration, increasing the risk of dehydration.
- Certain illnesses, particularly those involving vomiting and diarrhea, can result in significant fluid loss and increase the risk of dehydration.
Strategies for Preventing Dehydration in Different Settings
Implementing preventative measures tailored to different settings can significantly reduce the risk of dehydration.
| Setting | Prevention Strategies | Considerations |
|---|---|---|
| At Home | Provide regular access to water. Offer hydrating foods like fruits and vegetables. Monitor fluid intake during illness. | Ensure adequate hydration throughout the day, especially during hot weather. |
| Outdoor Activities | Carry water bottles and encourage frequent drinking. Schedule breaks in shaded areas. Avoid strenuous activity during peak heat hours. | Consider the duration and intensity of the activity. Monitor the child’s hydration status frequently. |
| Illness | Offer clear fluids like water, diluted juice, or electrolyte drinks. Monitor the frequency and amount of fluids consumed. Consult a healthcare professional for guidance on managing fluid intake during illness. | Pay close attention to signs of dehydration, such as decreased urination or dry mouth. Adjust fluid intake based on the child’s specific needs and the severity of the illness. |
When to Seek Immediate Medical Attention: Signs Of Dehydration In Kids
Dehydration, while often manageable at home, can quickly become a serious medical concern if left untreated. Recognizing the signs of severe dehydration is crucial for prompt intervention, potentially saving a child’s life. This section focuses on the critical indicators that necessitate immediate medical attention and why rapid response is essential in such situations.Severe dehydration can lead to life-threatening complications.
The body’s vital functions, including blood pressure regulation and organ perfusion, can be severely compromised. Early intervention minimizes these risks and improves the child’s chances of a full recovery.
Critical Signs Requiring Immediate Medical Attention
Early detection is paramount in managing dehydration effectively. Children exhibiting these severe symptoms require immediate medical attention. Symptoms include: profound lethargy or unresponsiveness, rapid or weak pulse, rapid breathing, sunken eyes, cold or clammy skin, and difficulty breathing or swallowing. Noticeably low blood pressure, indicating circulatory collapse, is also a significant concern.
Why Rapid Response is Crucial
Rapid response is essential in severe dehydration cases because the child’s body is rapidly losing vital fluids and electrolytes. Prolonged delays in treatment can lead to serious complications, including organ damage, seizures, and even death. Time is of the essence when dealing with severe dehydration.
Medical Professionals to Contact
In cases of severe dehydration, immediate contact with appropriate medical professionals is critical. A list of potential contacts follows:
- Emergency medical services (911 or local emergency number)
- A pediatrician or family doctor (if available)
- An urgent care facility
- A hospital emergency room
Promptly contacting the appropriate medical personnel increases the chances of a positive outcome. These resources are readily available to assist in assessing and treating severe dehydration.
Importance of Immediate Medical Intervention
Immediate medical intervention for severe dehydration is critical for preventing further complications. Prompt treatment helps restore fluid and electrolyte balance, stabilizing the child’s vital functions. A delay can lead to a cascade of adverse effects. For instance, a child suffering from severe dehydration might experience seizures due to electrolyte imbalance, which can have severe consequences. Treatment in these cases focuses on restoring fluid balance to ensure the child’s safety and well-being.
Flowchart for Seeking Medical Help
This flowchart illustrates the decision-making process when determining whether a child requires immediate medical attention for dehydration:
| Symptom/Observation | Action |
|---|---|
| Severe lethargy, unresponsiveness, rapid breathing, or weak pulse. | Call 911 or local emergency services immediately. |
| Sunken eyes, cold/clammy skin, difficulty breathing/swallowing, low blood pressure (if measurable). | Seek immediate medical attention from an urgent care facility or hospital emergency room. |
| Moderate dehydration symptoms (reduced urine output, dry mouth, slight lethargy). | Consult a pediatrician or family doctor for appropriate treatment and guidance. |
This structured approach helps parents and caregivers navigate the situation effectively. It highlights the different levels of urgency and the corresponding actions to take.
Concluding Remarks
In conclusion, recognizing the signs of dehydration in kids is vital for their well-being. By understanding the different stages of dehydration, assessing hydration levels, and knowing when to seek medical attention, parents can proactively safeguard their children’s health. Remember, prevention is key, and maintaining proper hydration habits, particularly during illness or intense physical activity, can significantly reduce the risk of dehydration.