How dangerous is non alcoholic fatty liver disease – How dangerous is non-alcoholic fatty liver disease? This condition, often silently progressing, can lead to serious health complications. Understanding its stages, risk factors, symptoms, and potential treatments is crucial for proactive health management. This comprehensive guide delves into the complexities of NAFLD, exploring its prevalence, potential complications, and strategies for prevention.
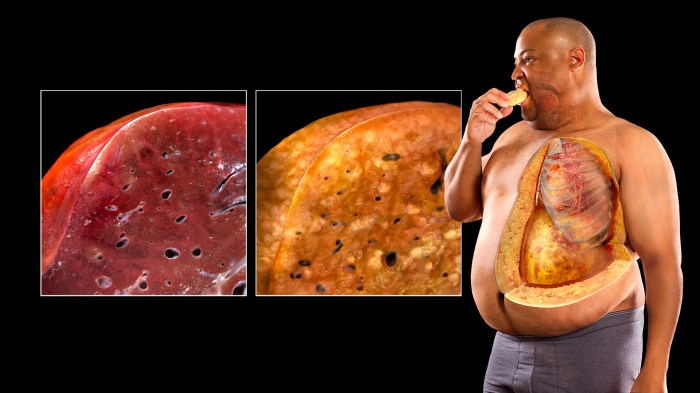
Non-alcoholic fatty liver disease (NAFLD) is a condition characterized by the buildup of fat in the liver. While often asymptomatic, NAFLD can progress to more serious liver conditions like cirrhosis and liver cancer. This detailed exploration examines the factors contributing to NAFLD, including genetics, diet, and lifestyle choices. The information presented aims to empower readers with knowledge to make informed decisions about their health.
Introduction to Non-Alcoholic Fatty Liver Disease (NAFLD)
Non-alcoholic fatty liver disease (NAFLD) is a common condition characterized by the accumulation of excess fat in the liver. This fat buildup isn’t caused by excessive alcohol consumption, a key differentiator from alcoholic fatty liver disease. While seemingly benign in its early stages, NAFLD can progress to more serious liver conditions if left unmanaged. Understanding its various stages and associated risk factors is crucial for preventative measures and timely intervention.NAFLD is a growing global health concern, affecting individuals across diverse demographics and impacting their overall well-being.
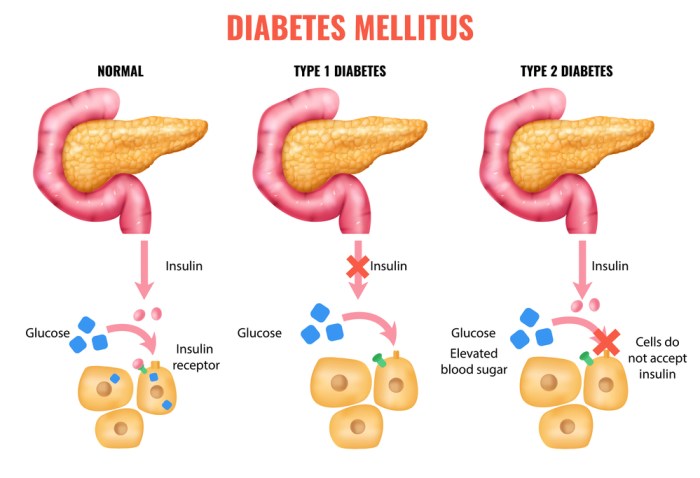
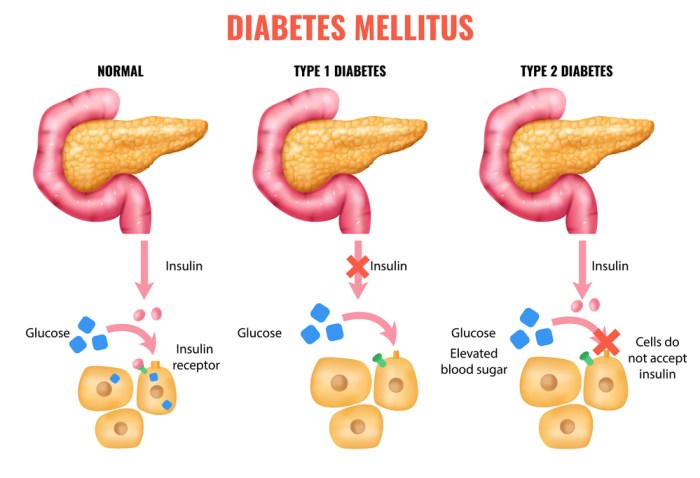
The prevalence of NAFLD is linked to rising rates of obesity, diabetes, and metabolic syndrome, highlighting the importance of lifestyle modifications and early detection in preventing more severe complications.
Prevalence and Demographics
NAFLD is increasingly prevalent worldwide, affecting a substantial portion of the population. Its prevalence is significantly higher in individuals with obesity, type 2 diabetes, and metabolic syndrome. Geographic variations exist, with certain populations demonstrating higher rates than others. The condition is observed across different ethnicities and age groups, making it a significant public health concern.
Non-alcoholic fatty liver disease (NAFLD) isn’t always a walk in the park, and while it can sometimes be mild, it can progress to something more serious. Interestingly, similar symptoms can sometimes arise from dehydration, which can cause stomach pain. For example, if you’re experiencing discomfort, understanding the potential connection between dehydration and your symptoms could be helpful.
Learning more about can dehydration cause stomach pain might shed some light on potential underlying causes. Ultimately, NAFLD’s severity varies, and a doctor’s diagnosis is crucial for proper management.
Stages of NAFLD Progression
NAFLD progresses through different stages, each with varying degrees of severity. Recognizing these stages is crucial for effective management and prevention of further complications. The progression is often insidious, meaning symptoms may not appear until the condition has advanced.
Summary of NAFLD Stages
| Stage | Description | Risk Factors | Potential Complications |
|---|---|---|---|
| Simple Steatosis (Fatty Liver) | Fat accumulation in the liver cells without inflammation or scarring. Often asymptomatic, meaning individuals may not experience any noticeable symptoms. | Obesity, insulin resistance, type 2 diabetes, high blood pressure, high cholesterol, a sedentary lifestyle, unhealthy diet. | If left untreated, can progress to more severe stages. While often asymptomatic, it can be a precursor to more severe liver conditions. |
| Nonalcoholic Steatohepatitis (NASH) | Characterized by inflammation and liver cell damage in addition to fat accumulation. Symptoms may include fatigue, abdominal pain, and discomfort. | Obesity, insulin resistance, type 2 diabetes, metabolic syndrome, high blood pressure, high cholesterol, unhealthy diet, lack of physical activity, genetic predisposition. | Cirrhosis, liver failure, liver cancer. Individuals with NASH are at higher risk of developing more severe liver damage. |
| Fibrosis | Scar tissue formation in the liver, caused by chronic inflammation. Early stages may be asymptomatic, while later stages may present with symptoms like fatigue, abdominal pain, and swelling. | Prolonged inflammation from NASH, unhealthy diet, lack of physical activity, genetic factors, and environmental toxins. | Cirrhosis, liver failure, liver cancer, portal hypertension. Fibrosis can significantly impair liver function. |
| Cirrhosis | Advanced scarring of the liver, significantly impacting its ability to function. Symptoms may include jaundice, ascites (fluid buildup in the abdomen), and encephalopathy (brain dysfunction). | Prolonged NASH and fibrosis, unhealthy diet, genetic factors, and environmental toxins. | Liver failure, liver cancer, increased risk of complications from portal hypertension, such as bleeding esophageal varices. |
Risk Factors for NAFLD
Non-alcoholic fatty liver disease (NAFLD) is a growing concern, affecting a significant portion of the global population. Understanding the factors contributing to its development is crucial for prevention and management. Identifying and analyzing these risk factors allows for targeted interventions and personalized strategies to reduce the likelihood of progression to more serious liver conditions.
Primary Risk Factors
Numerous factors increase the risk of developing NAFLD. These factors often interact and amplify each other, making it crucial to address them comprehensively. The interplay of multiple risk factors significantly increases the probability of NAFLD. For instance, a person with a family history of NAFLD and a sedentary lifestyle combined with a poor diet is at much higher risk than someone with only one of these risk factors.
Metabolic Syndrome Components
Metabolic syndrome is a cluster of conditions that significantly increase the risk of NAFLD. These conditions are often intertwined and contribute to a heightened inflammatory state in the body. These include obesity, insulin resistance, high blood pressure, and abnormal cholesterol levels. These factors disrupt the body’s metabolic balance, leading to excessive fat accumulation in the liver. Obesity, in particular, is a powerful driver, as excess fat is directly deposited into the liver, initiating the inflammatory cascade.
Non-alcoholic fatty liver disease (NAFLD) can be surprisingly serious, impacting overall health. It’s often overlooked, but it’s crucial to understand the potential health risks. Charnette Darrington’s personal experience with asthma, as detailed in her inspiring blog charnette darrington my journey with asthma , highlights the importance of proactive health management. Understanding chronic health conditions like asthma can be a powerful parallel to appreciating the gravity of NAFLD and the need for early detection and proactive care.
Lifestyle Factors
Unhealthy lifestyle choices are strong contributors to NAFLD. These include a diet high in processed foods, saturated fats, and refined sugars, along with a lack of physical activity. A sedentary lifestyle reduces the body’s ability to utilize glucose and process fats efficiently. This, in turn, contributes to the buildup of fat in the liver. A diet rich in unhealthy fats and low in fruits, vegetables, and whole grains can also elevate the risk significantly.
Furthermore, excessive alcohol consumption, while not a direct cause of NAFLD, can exacerbate the condition if present.
Genetic Predisposition
Genetic predisposition plays a substantial role in the development of NAFLD. Certain genetic variations can increase an individual’s susceptibility to developing the disease. Family history of NAFLD is a key indicator of genetic risk. These genetic factors influence how the body metabolizes fats and handles insulin. Individuals with a family history of NAFLD or other metabolic disorders are at a higher risk.
Age and Gender
Age and gender are also linked to the risk of NAFLD. The prevalence of NAFLD increases with age, likely due to the cumulative effects of lifestyle factors and metabolic changes over time. In addition, studies show a difference in the prevalence of NAFLD between men and women. This disparity may stem from hormonal differences and other factors that influence metabolic processes differently.
Table: Comparison of Risk Factors
| Risk Factor | Impact | Prevalence | Mitigation Strategies |
|---|---|---|---|
| Metabolic Syndrome | Disrupts metabolic balance, leading to fat accumulation in the liver. | High, increasing with age and poor lifestyle choices. | Weight management, regular exercise, healthy diet, and management of other metabolic conditions. |
| Lifestyle Factors | Unhealthy diet and lack of physical activity contribute to fat accumulation and insulin resistance. | High, influenced by socioeconomic factors and cultural norms. | Balanced diet rich in fruits, vegetables, and whole grains, regular physical activity, and reducing processed food consumption. |
| Genetic Predisposition | Certain genetic variations increase susceptibility to developing NAFLD. | Variable, influenced by family history and ethnicity. | Maintaining a healthy lifestyle and actively managing metabolic risk factors is crucial. |
| Age and Gender | Prevalence increases with age; differences in prevalence between men and women. | Increasing with age. Prevalence differences exist. | Adopting and maintaining a healthy lifestyle throughout life is essential. |
Symptoms and Diagnosis of NAFLD: How Dangerous Is Non Alcoholic Fatty Liver Disease

Non-alcoholic fatty liver disease (NAFLD) often progresses silently, meaning individuals may not experience any noticeable symptoms in its early stages. This lack of initial symptoms can make early diagnosis challenging. Understanding the potential symptoms and the various diagnostic methods available is crucial for early intervention and management.Early detection and treatment are vital to prevent the progression of NAFLD to more serious conditions like cirrhosis and liver cancer.
The absence of noticeable symptoms in the early stages necessitates reliance on diagnostic tools to identify and monitor the disease’s development.
Common Symptoms of NAFLD, How dangerous is non alcoholic fatty liver disease
Often, NAFLD presents with few or no symptoms. When symptoms do appear, they can be vague and easily mistaken for other conditions. Common symptoms include fatigue, abdominal discomfort, and mild upper right quadrant pain. However, these symptoms are not specific to NAFLD and can occur in other liver conditions or even be attributed to unrelated factors. This makes relying solely on symptoms for diagnosis problematic.
Careful consideration of a patient’s overall health, lifestyle, and other potential risk factors is essential.
Challenges in Diagnosing Early-Stage NAFLD
The lack of specific, noticeable symptoms in early NAFLD poses a significant challenge to early diagnosis. Many individuals with early-stage NAFLD may exhibit no symptoms whatsoever, making it difficult to identify the disease without specialized testing. The initial stages of NAFLD are often characterized by the accumulation of fat in the liver, a process that may not be immediately noticeable or cause discomfort.
This asymptomatic nature of early NAFLD underscores the importance of routine liver function tests and screenings for individuals at risk.
While non-alcoholic fatty liver disease (NAFLD) isn’t always a serious threat, it can certainly progress to more concerning issues. Managing other chronic conditions, like rheumatoid arthritis, requires careful consideration of treatments. For example, some Disease-Modifying Antirheumatic Drugs (DMARDs) for rheumatoid arthritis, like DMARDs for rheumatoid arthritis , can have potential liver side effects. So, while NAFLD might not be a direct result of arthritis treatments, it’s crucial to be aware of the interplay between health conditions when considering long-term treatments.
Diagnostic Methods for NAFLD
Various diagnostic methods are available to detect and assess the severity of NAFLD. These methods range from simple blood tests to more advanced imaging techniques. The choice of diagnostic method often depends on the patient’s specific circumstances, the suspected severity of the condition, and the availability of resources.
Table of Diagnostic Methods for NAFLD
| Diagnostic Method | Accuracy | Cost-Effectiveness | Limitations |
|---|---|---|---|
| Liver Function Tests (LFTs) | Moderate. Can detect abnormalities in liver function but not always specific to NAFLD. | Low cost, readily available. | Can be normal in early NAFLD, and doesn’t definitively diagnose NAFLD. May indicate other liver conditions. |
| Ultrasound | High. Can identify fatty liver and assess liver size. | Moderate cost, widely accessible. | May not detect mild steatosis (fat accumulation) in early stages. Can be influenced by overlying structures. |
| Computed Tomography (CT) Scan | High. Provides detailed images of the liver, allowing for assessment of liver size, structure, and the presence of complications. | Higher cost than ultrasound. | Requires specialized equipment and personnel. Exposure to radiation. |
| Magnetic Resonance Imaging (MRI) | High. Offers detailed images of the liver, potentially better for identifying subtle changes. | Higher cost than ultrasound. | Can be time-consuming. May not be suitable for individuals with certain medical conditions or contraindications. |
| Liver Biopsy | Gold standard for diagnosing NAFLD. Provides a direct examination of liver tissue. | High cost, invasive procedure. | Involves risks such as bleeding, infection, and discomfort. Provides only a snapshot of the liver at a specific location. |
Complications of NAFLD
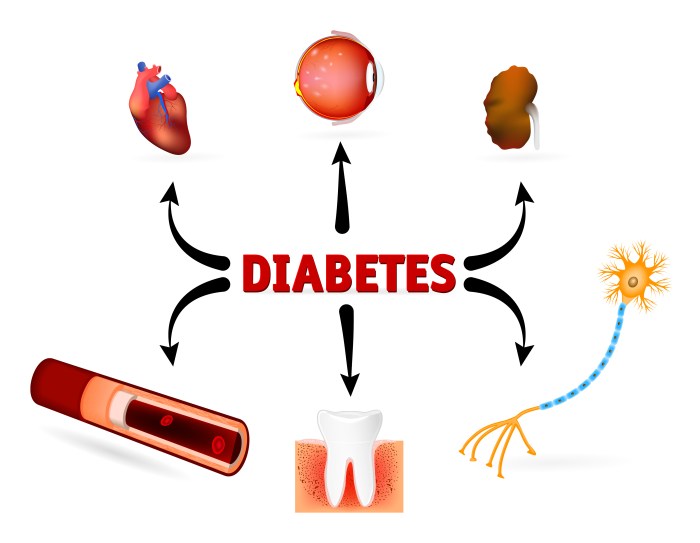
Non-alcoholic fatty liver disease (NAFLD) is a spectrum of liver conditions ranging from simple fat accumulation to more serious conditions like cirrhosis and liver cancer. While many individuals with NAFLD experience no symptoms or only mild discomfort, the potential for complications is significant and warrants careful monitoring. Understanding these complications is crucial for effective management and preventing long-term health consequences.
Potential Complications
NAFLD can progress to more severe liver conditions, impacting various organ systems and overall health. The severity and nature of complications depend on the extent of liver damage and the individual’s overall health. Early intervention and lifestyle modifications can often mitigate the progression to more serious complications.
Severity Across Stages
The severity of complications varies significantly across the different stages of NAFLD. Early stages, characterized primarily by fat accumulation in the liver, often have minimal or no complications. However, as the disease progresses, the potential for complications like fibrosis, cirrhosis, and liver failure increases. The progression from simple steatosis (fatty liver) to steatohepatitis (inflammation and damage) and ultimately cirrhosis can take years or even decades, highlighting the importance of proactive management.
The rate of progression varies considerably between individuals. Factors such as obesity, diabetes, and high blood pressure can accelerate the process.
Summary Table of Complications
| Potential Complications | Prevalence (Estimated) | Association with NAFLD Stages | Long-Term Impact |
|---|---|---|---|
| Hepatic Fibrosis | Common, increasing with disease duration | Moderate to severe stages (steatohepatitis and later stages) | Can lead to cirrhosis, potentially impacting liver function and increasing risk of liver cancer. |
| Cirrhosis | More prevalent in severe NAFLD | Advanced stage of NAFLD | Significant impairment of liver function, increasing risk of liver failure, portal hypertension, ascites, and potentially liver cancer. Patients may require liver transplantation. |
| Liver Cancer (Hepatocellular Carcinoma) | Increased risk in those with cirrhosis | Advanced stage of NAFLD, particularly with cirrhosis | Potentially fatal if not detected and treated early. A significant cause of mortality associated with NAFLD. |
| Portal Hypertension | Increased risk with cirrhosis | Advanced stage of NAFLD, particularly with cirrhosis | Elevated blood pressure in the portal vein, potentially causing complications like esophageal varices (bleeding veins), ascites (fluid buildup in the abdomen), and splenomegaly (enlarged spleen). |
| Hepatic Encephalopathy | Occurs in advanced cirrhosis | Advanced stage of NAFLD, particularly with cirrhosis | Impairment of brain function due to the accumulation of toxins normally filtered by the liver. Symptoms range from mild confusion to coma. |
| Ascites | Common in advanced cirrhosis | Advanced stage of NAFLD, particularly with cirrhosis | Accumulation of fluid in the abdomen, causing abdominal swelling and discomfort. Can be a sign of severe liver dysfunction. |
Note: Prevalence estimates are approximate and can vary depending on the specific population studied. The association with NAFLD stages is not absolute, and individual risk factors can influence the development and progression of complications.
Management and Treatment of NAFLD
Non-alcoholic fatty liver disease (NAFLD) is a serious health concern, and its management requires a multifaceted approach. Early intervention and lifestyle modifications play a crucial role in preventing the progression of NAFLD to more severe conditions like cirrhosis and liver cancer. Effective management often involves a combination of lifestyle changes, medical interventions, and close monitoring.
Lifestyle Modifications
Lifestyle modifications are the cornerstone of NAFLD management. These changes are essential for improving overall health and reducing the burden on the liver. A healthy lifestyle, including a balanced diet, regular exercise, and weight management, can significantly improve liver health. These interventions help to reduce hepatic fat content and improve insulin sensitivity, both of which are key factors in NAFLD.
- Balanced Diet: A diet rich in fruits, vegetables, whole grains, and lean protein, while limiting processed foods, sugary drinks, and excessive saturated and trans fats, is vital. This dietary approach helps to control calorie intake and promotes healthy weight management. For example, choosing lean protein sources like fish and poultry over red meat can be beneficial.
- Regular Exercise: Physical activity helps to improve insulin sensitivity, reduce visceral fat (fat stored around the organs), and promote overall health. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities at least twice a week.
- Weight Management: Losing even a small amount of weight can have a positive impact on NAFLD. Weight loss through a combination of diet and exercise is often recommended. A sustainable weight loss strategy, rather than quick fixes, is generally more effective and healthier in the long run.
Medical Interventions
Medical interventions for NAFLD are often necessary when lifestyle modifications alone are insufficient. These interventions aim to address underlying causes, control symptoms, and prevent complications. The specific interventions will vary depending on the severity of the disease and individual patient factors.
- Pharmacological Treatments: Certain medications, such as those that improve insulin sensitivity or lower blood lipids, may be prescribed to help manage NAFLD. These treatments aim to address the underlying metabolic issues contributing to the condition. Examples of such medications include metformin and statins.
- Bariatric Surgery: In severe cases of NAFLD associated with significant obesity, bariatric surgery may be considered. This surgical procedure aims to induce weight loss and improve liver health. However, bariatric surgery is a significant intervention with potential risks and is generally reserved for patients with severe obesity and significant complications from NAFLD.
Efficacy of Different Treatment Approaches
The efficacy of NAFLD treatments varies depending on the specific treatment and the individual patient. Lifestyle modifications, particularly weight loss, often show significant improvements in liver health and reduced risk of progression to more severe conditions. Pharmacological treatments can also help manage symptoms and slow disease progression. However, the long-term effectiveness of specific treatments needs further investigation.
Treatment Options Summary Table
| Treatment Option | Effectiveness | Potential Side Effects | Cost Considerations |
|---|---|---|---|
| Lifestyle Modifications (Diet & Exercise) | High, particularly for early-stage NAFLD | Generally low, but may include initial discomfort from dietary changes | Low, primarily focusing on lifestyle adjustments |
| Pharmacological Treatments (e.g., Metformin) | Moderate, can improve insulin sensitivity and reduce liver fat | May include gastrointestinal issues, or other side effects related to the medication | Moderate, costs associated with medications |
| Bariatric Surgery | High, can significantly improve liver health in severe cases | Potential for surgical complications, nutritional deficiencies, and long-term follow-up needs | High, costs associated with surgery and post-operative care |
Long-Term Outlook and Prognosis

Non-alcoholic fatty liver disease (NAFLD) is a significant health concern, impacting a substantial portion of the population. Understanding the long-term outlook and prognosis is crucial for individuals affected by NAFLD and their healthcare providers. While NAFLD often begins subtly, its progression can vary considerably. This section explores the potential long-term implications of NAFLD, including the factors influencing its course and the potential for more serious complications.The long-term prognosis for NAFLD is highly variable, depending on several key factors.
Some individuals may experience a benign course, with their liver function remaining stable over time. Others, however, may see their condition gradually worsen, potentially leading to more serious health problems. The factors influencing the prognosis will be explored in the following sections.
Factors Influencing Prognosis
A variety of factors contribute to the long-term outlook for individuals with NAFLD. These factors include the severity of the initial condition, lifestyle choices, and the presence of other underlying health issues.
- Severity of Initial NAFLD: The degree of fat accumulation in the liver at diagnosis plays a significant role. Mild NAFLD often resolves with lifestyle changes, while more severe cases may progress to non-alcoholic steatohepatitis (NASH), a more aggressive form of the disease. NASH is characterized by inflammation and scarring of the liver, which can further increase the risk of long-term complications.
- Metabolic Health: Individuals with associated metabolic conditions, such as type 2 diabetes, obesity, and high blood pressure, often have a higher risk of more severe disease progression. These conditions are often interconnected and influence the severity of NAFLD.
- Lifestyle Factors: Diet, physical activity, and alcohol consumption can significantly impact the course of NAFLD. A healthy lifestyle, including a balanced diet rich in fruits, vegetables, and whole grains, regular exercise, and moderation in alcohol consumption, can help slow the progression and potentially reverse the condition in some cases.
Potential for Disease Progression
NAFLD can progress to more serious liver conditions if left untreated or if the factors mentioned above aren’t addressed. Understanding the potential for progression is vital for early intervention and management.
- Non-Alcoholic Steatohepatitis (NASH): This more severe form of NAFLD involves inflammation and liver cell damage, leading to fibrosis (scarring). If left untreated, NASH can progress to cirrhosis, a serious condition characterized by irreversible scarring of the liver.
- Cirrhosis: Cirrhosis is a late-stage liver disease that results from chronic liver damage. This damage can cause the liver to lose its ability to function properly. Symptoms of cirrhosis can range from fatigue and abdominal swelling to jaundice and bleeding disorders. In advanced stages, cirrhosis can lead to liver failure, requiring liver transplantation.
- Liver Cancer: Cirrhosis significantly increases the risk of developing hepatocellular carcinoma (HCC), the most common type of liver cancer. The presence of cirrhosis, along with other risk factors like chronic inflammation and genetic predisposition, significantly increases the likelihood of developing liver cancer.
Impact on Overall Health
NAFLD’s impact extends beyond the liver, affecting various aspects of an individual’s overall health.
- Cardiovascular Disease: NAFLD is often associated with an increased risk of cardiovascular disease, including heart attacks and strokes. This is likely due to shared risk factors, such as obesity and insulin resistance.
- Metabolic Syndrome: NAFLD is frequently linked to metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. This highlights the interconnectedness of these health issues.
Prevention Strategies
Taking proactive steps to prevent non-alcoholic fatty liver disease (NAFLD) is crucial for maintaining long-term health. Early intervention and lifestyle modifications are key to mitigating the risk factors and potentially halting the progression of the disease. By focusing on modifiable lifestyle choices, individuals can significantly reduce their chances of developing NAFLD and its associated complications.
Lifestyle Interventions
Lifestyle modifications play a pivotal role in preventing NAFLD. A comprehensive approach that targets dietary habits, physical activity, and stress management is essential for reducing the risk. Consistent adherence to these changes is critical for long-term success.
- Maintaining a Healthy Weight: Obesity is a major risk factor for NAFLD. Achieving and maintaining a healthy weight through a balanced diet and regular exercise is paramount. Weight loss, even modest amounts, can significantly improve liver health and reduce the burden on the organ. For example, studies show that losing even 5-7% of body weight can improve liver fat content and reduce inflammation.
- Adopting a Balanced Diet: A diet rich in fruits, vegetables, whole grains, and lean protein sources, while limiting processed foods, sugary drinks, and excessive saturated and unhealthy fats, is fundamental in preventing NAFLD. Focusing on nutrient-dense foods and mindful portion control can create a positive impact on liver health. For instance, a diet rich in antioxidants found in fruits and vegetables can help neutralize free radicals that can contribute to liver damage.
- Regular Physical Activity: Engaging in regular physical activity is crucial for overall health and reducing the risk of NAFLD. Aiming for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, combined with muscle-strengthening activities, can significantly contribute to weight management and improved insulin sensitivity, both of which are important in preventing NAFLD.
- Managing Stress: Chronic stress can negatively impact liver health. Incorporating stress-reducing techniques like meditation, yoga, or spending time in nature can help maintain overall well-being and reduce the risk of NAFLD.
Early Detection and Management
Early detection and proactive management are essential for preventing the progression of NAFLD. Regular check-ups and monitoring of liver function are important tools for identifying potential issues early.
- Regular Liver Function Tests: Routine liver function tests can help detect early signs of liver damage. These tests can identify elevated liver enzymes, which can be an indicator of developing NAFLD. Regular monitoring allows for timely intervention and management.
- Consultation with Healthcare Professionals: Regular consultations with healthcare professionals, including a primary care physician or gastroenterologist, can help monitor and manage risk factors for NAFLD. Professional guidance on lifestyle modifications, dietary recommendations, and potential treatment options can greatly improve the chances of preventing disease progression.
Preventative Measures
Implementing preventative measures is vital in the fight against NAFLD. A holistic approach that integrates lifestyle changes and regular monitoring is critical for success.
- Avoiding Excessive Alcohol Consumption: Alcohol consumption is a significant risk factor for NAFLD. Limiting or abstaining from alcohol can significantly reduce the risk of liver damage. This includes avoiding excessive alcohol consumption, which can contribute to fatty liver.
Wrap-Up
In conclusion, non-alcoholic fatty liver disease (NAFLD) is a serious health concern that requires careful attention. Understanding the risk factors, stages, symptoms, and treatment options is vital for early detection and effective management. Adopting a healthy lifestyle, including a balanced diet and regular exercise, can significantly reduce the risk of developing NAFLD. By taking proactive steps towards prevention and early intervention, individuals can improve their long-term health outcomes.