Dysesthesia and multiple sclerosis: a complex interplay of nerve damage and sensory disturbance. This exploration delves into the various forms of dysesthesia, from burning sensations to tingling and prickling, experienced by individuals living with multiple sclerosis (MS). We’ll examine the underlying neurological mechanisms, the impact on daily life, and the current strategies for management, drawing on patient experiences and insights from the research community.
The experience of dysesthesia in MS is multifaceted, impacting not only physical sensations but also emotional well-being and social interactions. This comprehensive look will discuss the diagnostic considerations, highlighting the challenges in differentiating dysesthesia from other neurological conditions. We’ll also consider the effectiveness of different treatment approaches, including medication, physical therapy, and alternative therapies, as well as the perspectives of patients themselves.
Defining Dysesthesia in Multiple Sclerosis
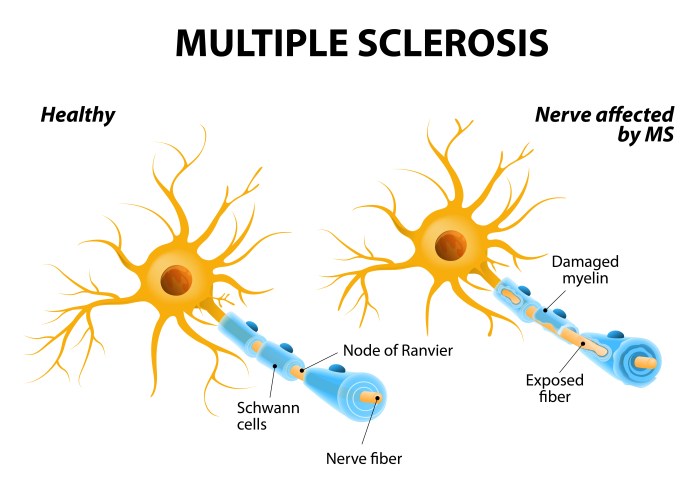
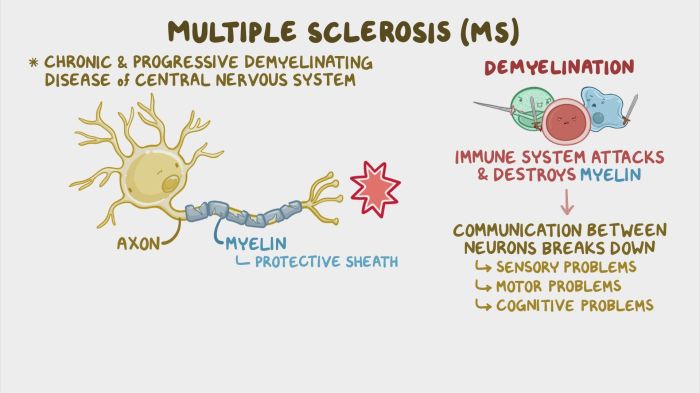
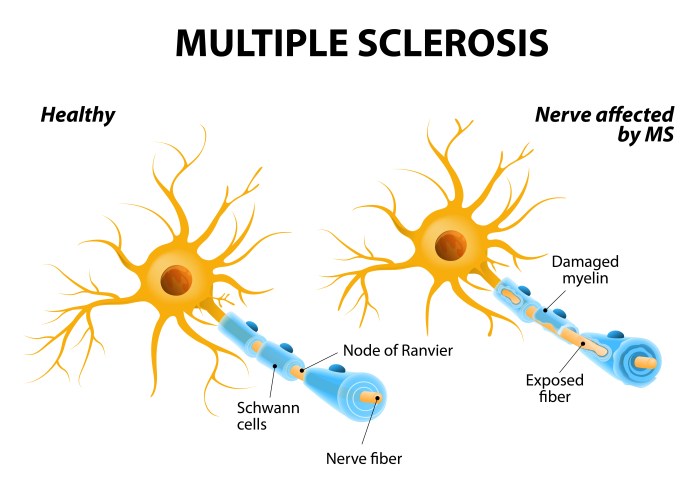
Dysesthesia, a common symptom in multiple sclerosis (MS), encompasses a range of abnormal sensations that are often distressing for individuals living with the condition. These sensations typically involve unusual or unpleasant feelings in the skin and other tissues, and can significantly impact daily life. Understanding the different types of dysesthesia and their underlying mechanisms is crucial for effective management and support.Dysesthesia in MS arises from damage to the myelin sheath, the protective covering of nerve fibers.
This damage, caused by the immune system’s attack in MS, disrupts the transmission of nerve signals. This disruption can lead to a cascade of abnormal sensations, manifesting as various forms of dysesthesia. The precise location and extent of the nerve damage significantly influence the type and intensity of the dysesthetic experience.
Types of Dysesthesia in MS
Dysesthesia in MS presents in diverse forms, each reflecting the specific nerve pathways affected. Common types include burning, tingling, and pricking sensations. These sensations often fluctuate in intensity and location, potentially affecting various parts of the body, from the limbs to the face.
Mechanisms of Dysesthesia in MS
The mechanisms underlying dysesthesia in MS involve the disruption of normal nerve signal transmission. Damaged myelin sheaths impair the efficient propagation of nerve impulses, leading to altered sensory input to the brain. This disruption can result in misinterpretations of sensory information, giving rise to the various dysesthetic sensations experienced by individuals with MS. Furthermore, inflammation and scarring (sclerosis) in the nervous system can also contribute to the development of dysesthesia.
Comparing Dysesthesia in MS with Other Neurological Conditions
| Symptom | Multiple Sclerosis | Peripheral Neuropathy | Diabetic Neuropathy |
|---|---|---|---|
| Burning | Common, often associated with pain and discomfort | Common, often described as “pins and needles” or “electric shock” | Common, often described as “burning” or “shooting” pain |
| Tingling | Frequent, often described as “pins and needles” | Frequent, often described as “pins and needles” or “numbness” | Frequent, often described as “pins and needles” or “numbness” |
| Pricking | Occasional, may be accompanied by other sensations | Occasional, may be accompanied by other sensations | Occasional, may be accompanied by other sensations |
| Location | Variable, can affect any part of the body | Often begins in the extremities (feet, hands) and progresses | Often begins in the extremities (feet, hands) and progresses |
| Intensity | Variable, ranging from mild to severe | Variable, ranging from mild to severe | Variable, ranging from mild to severe |
The table above highlights some common symptoms and locations across different neurological conditions. Note that the symptoms can overlap, and a comprehensive neurological assessment is crucial for accurate diagnosis. Precise symptom description, including the location, duration, and intensity of the sensations, is essential for differentiating between various conditions.
Prevalence and Impact of Dysesthesia
Dysesthesia, a symptom characterized by unusual or unpleasant sensations, is a frequent companion for individuals living with multiple sclerosis (MS). This discomfort can range from mild tingling to severe burning pain, significantly impacting daily life. Understanding its prevalence and the far-reaching effects on quality of life is crucial for developing effective management strategies.The experience of dysesthesia in MS is multifaceted, extending beyond the purely physical.
It often creates a ripple effect, affecting emotional well-being and social interactions. This section will explore the prevalence of dysesthesia in the MS population, its impact on daily activities, and the broader implications for those affected.
Prevalence of Dysesthesia in MS
Studies indicate that dysesthesia is a common symptom among people with MS. Precise prevalence figures can vary depending on the specific study methodology and the definition used for dysesthesia. However, a significant portion of individuals with MS report experiencing some form of dysesthesia at various points in their disease progression. For example, one study might focus on burning pain, while another focuses on tingling.
These variations in the way dysesthesia is measured can affect the final prevalence numbers. Furthermore, the subjective nature of the symptom makes consistent assessment challenging.
Impact on Daily Life Activities
Dysesthesia can significantly interfere with everyday activities. Simple tasks like dressing, eating, or even walking can become challenging and painful. The constant discomfort can lead to fatigue, impacting the ability to engage in hobbies or social activities. This symptom can also impact a person’s work performance, reducing productivity and potentially leading to job loss or career changes.
For instance, a person might experience intense dysesthesia in their hands, making it difficult to type or hold objects. Similarly, someone experiencing pain in their legs might find walking or even standing for extended periods challenging.
Impact on Quality of Life
The presence of dysesthesia can substantially diminish quality of life. The chronic pain and discomfort can lead to anxiety, depression, and feelings of isolation. Individuals might withdraw from social activities, fearing judgment or embarrassment about their symptoms. Furthermore, the unpredictability of dysesthesia episodes can cause stress and disruption in daily routines. This can lead to decreased social interaction and diminished overall well-being.
Impact on Emotional Well-being, Dysesthesia and multiple sclerosis
The emotional toll of living with dysesthesia in MS is substantial. Chronic pain and discomfort can lead to feelings of frustration, anger, and hopelessness. The unpredictable nature of the symptom can cause anxiety and fear about future episodes. The constant awareness of the discomfort can negatively affect mood and self-esteem. The isolation and lack of understanding from others can compound these feelings, potentially leading to depression.
Social and Psychological Implications
The social and psychological implications of dysesthesia in MS are profound. Individuals may feel stigmatized or embarrassed by their symptoms, leading to social isolation. This can negatively impact relationships, employment, and overall well-being. The lack of understanding or empathy from others can exacerbate feelings of isolation and frustration. The impact on self-image and confidence is significant.
For example, a person with dysesthesia might avoid social gatherings, fearing they will be judged or misunderstood.
Frequency of Different Types of Dysesthesia
| Type of Dysesthesia | Frequency (Approximate Percentage) |
|---|---|
| Burning Pain | 35-45% |
| Tingling | 25-35% |
| Numbness | 20-30% |
| Sharp Pain | 10-20% |
| Paresthesia (Combination of above) | 10-15% |
Note: The percentages are approximate and based on a compilation of various studies. The frequency of each type of dysesthesia may vary based on individual factors and disease progression.
Diagnostic Considerations
Pinpointing dysesthesia in multiple sclerosis (MS) can be challenging, requiring a multifaceted approach. Accurate diagnosis hinges on a thorough understanding of the patient’s symptoms, medical history, and neurological examination findings. This process often involves distinguishing dysesthesia from other conditions that may present with similar sensations.
Diagnostic Process for Dysesthesia in MS
The diagnostic journey for dysesthesia in MS starts with a comprehensive history-taking session. This involves meticulous questioning about the onset, duration, location, and characteristics of the sensory symptoms. Patients are asked to describe the type of pain, tingling, or burning they experience. The pattern of symptom progression and any potential triggers are also documented.
Physical Examinations and Neurological Assessments
A crucial aspect of the diagnostic process is the physical examination. Neurologists meticulously evaluate reflexes, muscle strength, coordination, and sensation. Specific tests are performed to pinpoint the affected areas and assess the severity of the sensory disturbance. This includes testing for touch, pain, temperature, and vibration perception in various parts of the body. A detailed neurological examination aids in identifying the presence and extent of neurological deficits, which can correlate with MS-related dysesthesia.
Role of Diagnostic Tools and Procedures
Several diagnostic tools are employed to confirm the suspicion of MS and to determine if dysesthesia is a manifestation of the disease. Magnetic Resonance Imaging (MRI) of the brain and spinal cord is often the cornerstone of the diagnostic process. MRI scans can reveal characteristic lesions indicative of MS, helping to support the diagnosis. Evoked potential studies, particularly somatosensory evoked potentials, may assist in evaluating nerve conduction and sensory processing, offering further insights into the nature of the sensory disturbance.
Other tools like lumbar puncture (spinal tap) can help rule out other conditions. However, there is no single definitive test for MS, making the diagnosis often a process of elimination and integration of multiple findings.
Challenges in Differentiating Dysesthesia in MS
Differentiating dysesthesia in MS from other conditions can be challenging. Symptoms like numbness, tingling, and pain can mimic those of other neurological disorders, vascular issues, or even psychiatric conditions. For instance, diabetic neuropathy can present with similar symptoms, making a precise diagnosis difficult. Thorough investigation, including detailed medical history and relevant laboratory tests, is vital in separating MS-related dysesthesia from alternative diagnoses.
Differential Diagnoses for Dysesthesia in MS
| Condition | Key Features | Distinguishing Factors |
|---|---|---|
| Diabetic Neuropathy | Sensory symptoms often associated with diabetes mellitus, may follow a symmetrical pattern | Presence of diabetes or other metabolic risk factors; often accompanied by other diabetic complications |
| Postherpetic Neuralgia | Chronic pain following a shingles (herpes zoster) infection | History of herpes zoster infection; typically localized to the area affected by the rash |
| Peripheral Neuropathy | Sensory loss or pain affecting peripheral nerves | Presence of risk factors such as alcohol abuse, toxins, or certain medications; often associated with muscle weakness or atrophy |
| Complex Regional Pain Syndrome (CRPS) | Intense, localized pain disproportionate to the initial injury | History of an injury; often involves vasomotor and trophic changes in the affected area |
| Vascular Disorders | Sensory symptoms can be associated with cerebrovascular disease or peripheral artery disease | Presence of risk factors for vascular disease; associated neurological symptoms may be focal or transient |
Management Strategies
Living with dysesthesia in multiple sclerosis (MS) can be challenging, but effective management strategies can significantly improve quality of life. These strategies aim to alleviate symptoms, enhance functional abilities, and promote overall well-being. Understanding the diverse approaches available empowers individuals to actively participate in their care and find what works best for them.
Medication Approaches
Medications play a crucial role in managing MS-related dysesthesia. They can target different aspects of the condition, such as nerve pain, inflammation, or other contributing factors. The selection of medication often depends on the specific symptoms, their severity, and individual patient responses.
- Analgesics (Pain Relievers): Non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen are frequently used for mild to moderate pain. Opioid analgesics may be considered for more severe cases, but their use should be carefully evaluated due to potential side effects like addiction. Individual tolerance to these medications varies.
- Anticonvulsants: Certain anticonvulsant medications, like gabapentin and pregabalin, have demonstrated effectiveness in reducing neuropathic pain, a common component of MS-related dysesthesia. They often work by modulating nerve activity. However, side effects can include drowsiness, dizziness, and weight gain.
- Tricyclic Antidepressants (TCAs): These medications, sometimes used for pain management, can also alleviate dysesthesia. While effective for some, their use is often limited by potential side effects, including dry mouth, constipation, and blurred vision. A careful assessment of risks and benefits is necessary.
- Other Medications: In certain cases, other medications, such as antidepressants, may be used in conjunction with other treatments. The effectiveness and appropriateness of these medications need to be discussed with a neurologist or pain specialist.
Physical Therapy Techniques
Physical therapy interventions can significantly aid in managing dysesthesia by improving sensory function, promoting muscle strength, and enhancing mobility. Specific exercises and techniques can help reduce pain and improve overall functioning.
- Sensory Re-education: Exercises that re-educate the nervous system to process sensory input more effectively can be beneficial. These exercises might involve targeted stimulations or desensitization techniques.
- Strengthening Exercises: Improving muscle strength can help stabilize joints and reduce pain. Specific exercises designed to target muscles involved in maintaining posture or performing daily tasks are crucial.
- Range-of-Motion Exercises: Maintaining flexibility and joint mobility is essential for preventing stiffness and discomfort. Gentle stretches and movements help preserve the range of motion.
- Balance and Coordination Exercises: Improved balance and coordination can minimize falls and injuries, which can be significant in managing MS-related symptoms.
Alternative Therapies
While evidence supporting some alternative therapies for dysesthesia in MS is limited, some individuals find relief from complementary approaches. Individual experiences vary.
Experiencing dysesthesia with multiple sclerosis can be challenging, impacting daily life significantly. It’s important to consider the health implications of blood donation when managing conditions like lupus, as some medical guidelines might advise against it. For instance, if you have lupus, understanding the specific requirements around donating blood is crucial, as detailed in this informative resource on donating blood with lupus.
Ultimately, consulting with your doctor remains the best approach to navigate blood donation safely and effectively when dealing with conditions like dysesthesia and multiple sclerosis.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. Some individuals report pain relief, but scientific evidence for its effectiveness in MS-related dysesthesia remains inconclusive.
- Massage Therapy: Therapeutic massage can help relax muscles, reduce tension, and potentially improve circulation. The impact on dysesthesia may be variable.
- Mindfulness and Relaxation Techniques: Practices like meditation and deep breathing can reduce stress and anxiety, which may indirectly alleviate symptoms. They can enhance coping mechanisms.
Comparative Treatment Table
| Treatment Approach | Efficacy | Potential Side Effects | Evidence Base |
|---|---|---|---|
| Analgesics (e.g., NSAIDs) | Mild to moderate pain relief | Gastrointestinal issues, kidney problems | Strong |
| Anticonvulsants (e.g., Gabapentin) | Effective for neuropathic pain | Drowsiness, dizziness, weight gain | Moderate |
| Physical Therapy | Improves function and reduces pain | No significant side effects | Strong |
| Acupuncture | Varied results | Possible bruising, infection | Limited |
Patient Experiences and Perspectives
Living with multiple sclerosis (MS) is a deeply personal journey, and the experience of dysesthesia is no exception. This complex sensory disturbance can profoundly impact daily life, affecting not just physical function but also emotional well-being. Understanding the lived experiences of individuals with MS who experience dysesthesia is crucial for developing effective and patient-centered management strategies. This section will delve into the realities faced by those living with this condition.
Lived Experiences of Dysesthesia in MS
Dysesthesia in MS manifests as a wide range of unusual sensations, from burning and prickling to numbness and pain. These sensations are often unpredictable, fluctuating in intensity and location, and can significantly impact an individual’s quality of life. The chronic nature of MS and the accompanying dysesthesia can lead to significant emotional distress, including anxiety, depression, and frustration.
Experiencing dysesthesia with multiple sclerosis can be tough, impacting daily life in various ways. One aspect often overlooked is the potential for digestive issues, and it’s worth exploring if medications are contributing. For example, some antibiotics can lead to constipation, a condition that could potentially exacerbate the discomfort associated with multiple sclerosis. Further research into this connection is important to consider when managing these conditions.
More information on how antibiotics affect bowel movements can be found here: do antibiotics cause constipation. Ultimately, understanding the interplay between these factors is key to better managing symptoms and overall well-being for those with multiple sclerosis and dysesthesia.
The constant discomfort and unpredictable nature of the symptoms can be deeply isolating, making social interaction challenging and impacting relationships.
Impact on Daily Life
The impact of dysesthesia on daily life varies greatly from person to person, depending on the severity and location of the symptoms. Many individuals report difficulty with simple tasks, such as dressing, eating, or even holding everyday objects. The unpredictable nature of the symptoms can also make it difficult to maintain employment or participate in social activities. Sleep disturbances are also common, further compounding the challenges faced by individuals with MS and dysesthesia.
Patient Testimonials
Direct patient experiences offer invaluable insights into the challenges of managing dysesthesia. One patient might describe the constant burning sensation as an unrelenting torment, while another may focus on the difficulty of maintaining fine motor skills needed for writing or crafting. These varying experiences highlight the profound impact dysesthesia can have on an individual’s life.
Dealing with dysesthesia in multiple sclerosis can be tough, and finding relief is often a journey. Managing symptoms like this often involves exploring various options, including prescription and OTC drugs. Knowing the difference between these options can be crucial when trying to manage symptoms effectively, which is why I highly recommend checking out this guide on prescription and OTC drugs.
Ultimately, understanding the different approaches to managing dysesthesia and MS is key to finding what works best for you.
Importance of Patient-Centered Care
Effective management of dysesthesia in MS requires a patient-centered approach. Healthcare providers must actively listen to patient concerns, understand their individual experiences, and tailor treatment strategies to their specific needs. Open communication, empathy, and shared decision-making are essential for fostering a supportive environment where patients feel empowered to actively participate in their care. This collaborative approach leads to better symptom control and improved overall well-being.
Challenges and Frustrations
Patients with MS and dysesthesia often face a range of challenges and frustrations. These include the unpredictable nature of the symptoms, the lack of readily available and effective treatments, and the difficulty in communicating their experiences to healthcare professionals. The need for ongoing adjustments to daily routines and the potential for social isolation can be especially disheartening.
Patient Feedback on Dysesthesia Management
“The unpredictability of the burning sensation is the worst. One minute I’m fine, the next I’m struggling to even hold a cup of coffee. Finding relief is like searching for a needle in a haystack.”
Patient testimonial regarding dysesthesia management.
Research and Future Directions
Unraveling the complexities of dysesthesia in multiple sclerosis (MS) requires a multifaceted approach. Current research provides valuable insights, but significant gaps remain in our understanding of its underlying mechanisms and effective management strategies. Future research must address these gaps to improve the quality of life for individuals living with this debilitating symptom.The current body of research highlights the multifaceted nature of dysesthesia in MS, suggesting that it’s not merely a simple sensory disturbance.
Understanding the intricate interplay of neurobiological factors, psychological influences, and environmental triggers is crucial for developing effective therapeutic interventions. A deeper dive into these areas will pave the way for more personalized and targeted treatments.
Gaps in Current Research
Current research often lacks longitudinal studies that track the progression of dysesthesia in MS over extended periods. This lack of longitudinal data hinders the ability to identify predictors of symptom severity and responsiveness to different treatments. Furthermore, studies often lack diverse representation, potentially leading to biased results. This is critical, as the experience of dysesthesia can vary significantly across individuals with different MS subtypes and disease severities.
Potential Areas for Future Research
A critical area for future research is developing novel biomarkers for dysesthesia in MS. These biomarkers could aid in early detection, monitoring disease progression, and evaluating treatment efficacy. Neuroimaging techniques, such as functional MRI, could reveal neural correlates of dysesthesia, offering insights into the underlying mechanisms. Furthermore, exploring the impact of environmental factors, such as stress and sleep disturbances, on dysesthesia could lead to the development of preventative strategies.
Emerging Therapies and Treatments
Emerging therapies, such as non-pharmacological interventions like transcranial magnetic stimulation (TMS) and virtual reality (VR) therapies, show promise in managing neuropathic pain, including dysesthesia. These approaches offer a potential pathway to reduce reliance on pharmacological interventions with their associated side effects. Preliminary research suggests that these therapies can modulate neural activity and improve sensory processing, potentially leading to symptom reduction.
Promising Research Methodologies
Multidisciplinary research teams incorporating neurologists, psychologists, and physical therapists are essential for advancing the understanding of dysesthesia. Utilizing advanced statistical modeling techniques, such as machine learning algorithms, to analyze complex data sets can identify patterns and predictors of symptom progression. Developing robust, standardized assessment tools for dysesthesia in MS is also crucial to ensure consistent and comparable results across different studies.
Importance of Ongoing Research
Ongoing research is vital for improving the lives of individuals with MS experiencing dysesthesia. By addressing the knowledge gaps and exploring innovative approaches, we can develop more effective treatments and ultimately enhance the quality of life for those affected. The potential for personalized treatments and targeted interventions is substantial, promising a future where dysesthesia in MS is better managed and understood.
Illustrative Case Studies
Unveiling the complexities of diagnosing and managing dysesthesia in multiple sclerosis (MS) requires a deep understanding of individual experiences. These case studies, while fictional, aim to highlight the challenges faced by patients, the diagnostic nuances, and the range of treatment options considered. They serve as illustrative examples, emphasizing the need for a holistic approach to care.
Case Study 1: Progressive Sensory Disturbances
This case revolves around a 35-year-old woman, Sarah, diagnosed with relapsing-remitting MS three years prior. Over the past six months, Sarah has experienced progressive dysesthesia, characterized by burning and prickling sensations in her left arm and leg. The sensations are more pronounced at night, interfering with sleep. Initially, the symptoms were attributed to nerve compression, but they have persisted despite conservative measures.
The patient also reports some mild cognitive changes.The diagnostic process involved a comprehensive neurological examination, including sensory testing and nerve conduction studies. Magnetic resonance imaging (MRI) scans confirmed the presence of MS lesions, though the correlation between the lesions and the specific dysesthetic symptoms remained uncertain. Treatment options explored included various medications to manage MS symptoms, such as corticosteroids for inflammation, and physical therapy for pain management.
Additional investigations for other potential causes, such as vitamin deficiencies or peripheral neuropathy, were also considered. Due to the progressive nature of the dysesthesia and lack of clear correlation to MS lesions, a trial of gabapentin was initiated to manage the neuropathic pain.
Case Study 2: Episodic Dysesthesia and Cognitive Impairment
Consider a 48-year-old man, David, with a history of secondary progressive MS. He has experienced episodic bouts of severe dysesthesia, primarily affecting his face and hands, accompanied by fluctuating cognitive impairment. These episodes typically last for a few days and are often triggered by stress or fatigue. The episodic nature of the dysesthesia and its association with cognitive fluctuations posed diagnostic challenges.The diagnostic process included a detailed medical history, focusing on the episodic nature of the symptoms.
Neuropsychological testing was employed to assess the cognitive fluctuations. MRI scans revealed active MS lesions, particularly in areas associated with sensory processing and cognition. Treatment options considered included medications to manage MS symptoms, such as disease-modifying therapies (DMTs) and symptomatic treatments for the dysesthesia. The patient was also encouraged to adopt stress-reducing techniques to minimize the frequency of episodes.
Case Study 3: Dysesthesia and Autonomic Dysfunction
A 62-year-old woman, Emily, with a history of primary progressive MS, has experienced progressive dysesthesia, characterized by a combination of burning, tingling, and numbness in her lower extremities. The dysesthesia is accompanied by autonomic symptoms, such as bladder dysfunction and postural hypotension. These symptoms have gradually worsened over the past year.The diagnostic process focused on identifying the underlying cause of the dysesthesia and autonomic dysfunction.
The patient underwent a thorough neurological evaluation, including autonomic function tests, and blood tests to rule out other potential medical conditions. MRI scans revealed progressive MS lesions affecting both the sensory and autonomic pathways. Treatment options focused on managing both the MS and the accompanying symptoms. This included medications to address the autonomic dysfunction, such as bladder retraining exercises and blood pressure medications, along with medications to address the dysesthesia.
Summary of Case Studies
| Case Study | Key Features | Diagnostic Process | Treatment Options |
|---|---|---|---|
| Case 1: Progressive Sensory Disturbances | Progressive dysesthesia in left arm/leg, night-time exacerbation, mild cognitive changes | Comprehensive neurological exam, sensory testing, nerve conduction studies, MRI scans | MS symptom management (corticosteroids), physical therapy, investigation for other causes, gabapentin trial |
| Case 2: Episodic Dysesthesia and Cognitive Impairment | Episodic dysesthesia (face/hands), fluctuating cognitive impairment, stress/fatigue triggers | Detailed medical history, neuropsychological testing, MRI scans | MS symptom management (DMTs), symptomatic treatments for dysesthesia, stress-reducing techniques |
| Case 3: Dysesthesia and Autonomic Dysfunction | Progressive dysesthesia (lower extremities), autonomic symptoms (bladder dysfunction, hypotension) | Thorough neurological evaluation, autonomic function tests, blood tests, MRI scans | MS symptom management, medications for autonomic dysfunction (bladder retraining, blood pressure meds), medications for dysesthesia |
Illustrative Visualizations
Unveiling the intricate tapestry of dysesthesia in multiple sclerosis requires more than just words. Visual representations can illuminate the underlying mechanisms, the body’s response, and the impact of this neurological disorder. These visualizations offer a window into the complex interplay of nerve damage, sensory pathways, and the resulting symptoms, ultimately facilitating a deeper understanding of the condition.Visualizations provide a powerful tool for clinicians, researchers, and patients alike.
They help to illustrate the complex neurological pathways affected by dysesthesia, facilitating communication and understanding of the condition. They can also demonstrate the diverse range of symptoms and their potential impact on daily life. This section delves into various visual representations that can enhance our grasp of dysesthesia in MS.
Mechanisms of Nerve Damage
Understanding how nerve damage leads to dysesthesia is crucial. Visualizations can depict the demyelination process in the peripheral and central nervous system. A diagram could show a healthy nerve fiber, encased in a protective myelin sheath, juxtaposed with a damaged nerve fiber where the myelin is disrupted. This would highlight how the disruption of this sheath interferes with the efficient transmission of nerve impulses, leading to altered sensations.
Further, the visualization could depict how inflammation and scarring can occur around the nerve fibers. These inflammatory processes can cause additional damage to the nerve, resulting in persistent sensory issues.
Distribution of Dysesthesia
Dysesthesia in MS is not uniform. A visual representation, such as a body map, can show the common patterns of dysesthesia distribution. Different shades of color or intensity of markings on the map could illustrate the severity and extent of sensory abnormalities across various parts of the body. For instance, a darker shade of color could signify more intense or frequent dysesthetic sensations in a particular limb or region.
This representation could aid in the clinical assessment of the patient and assist in identifying potential areas of nerve involvement.
Neurological Pathways Affected
Visualizing the neurological pathways affected by dysesthesia provides a comprehensive understanding of the condition’s impact. A diagram could trace the sensory pathways from the periphery of the body to the brain. Areas of the central nervous system, such as the thalamus and the somatosensory cortex, where these pathways converge, could be highlighted. The diagram could also show how demyelination and inflammation along these pathways disrupt the normal flow of sensory information, leading to the various types of dysesthesia.
This visual representation allows clinicians to identify potential areas of dysfunction within the sensory system.
Scans and Imaging Techniques
Various scans and imaging techniques provide invaluable insights into the structural and functional changes associated with MS and dysesthesia. Magnetic Resonance Imaging (MRI) scans are frequently used to visualize the brain and spinal cord. These scans can identify areas of demyelination, lesions, and inflammation. A sample MRI image could depict hyperintense lesions characteristic of MS. Additionally, Functional MRI (fMRI) scans can be used to examine the brain activity related to sensory processing, offering insights into the functional consequences of dysesthesia.
A visual comparison of fMRI scans from a healthy individual and one with MS could highlight the differences in brain activity during sensory tasks. Similarly, evoked potential studies, which measure the electrical activity in response to sensory stimuli, could be visualized in a graph format, displaying the differences in latency and amplitude compared to healthy individuals.
Last Word: Dysesthesia And Multiple Sclerosis
In conclusion, dysesthesia in multiple sclerosis is a significant challenge, impacting quality of life in profound ways. While current management strategies offer some relief, the complexities of diagnosis and the ongoing need for personalized care remain key areas of focus. Further research and improved understanding of the mechanisms driving dysesthesia are crucial to advancing effective treatments and improving the lives of individuals living with MS.
The shared experiences and perspectives presented throughout this exploration underscore the need for a holistic and patient-centered approach to care.