Myasthenia gravis vs ALS: This exploration delves into the complexities of two debilitating neurological diseases. We’ll dissect their distinct characteristics, highlighting the fundamental differences in their neurological mechanisms and symptoms. Understanding these nuances is crucial for grasping the unique challenges faced by those affected.
This detailed comparison will cover everything from the initial symptoms and diagnostic procedures to the available treatments and their potential impact on daily life. We will also look at the current research efforts and support systems available to patients and caregivers. The goal is to provide a comprehensive overview for anyone seeking to understand these conditions better.
Understanding Myasthenia Gravis and Amyotrophic Lateral Sclerosis
Myasthenia gravis (MG) and amyotrophic lateral sclerosis (ALS) are both debilitating neurological disorders, impacting the ability to control muscles. While both conditions affect the nervous system, their underlying causes, symptoms, and progression differ significantly. Understanding these differences is crucial for accurate diagnosis and tailored treatment plans.
Fundamental Neurological Mechanisms
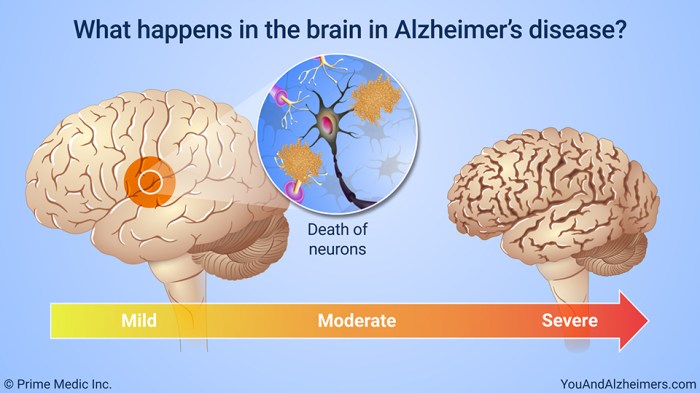
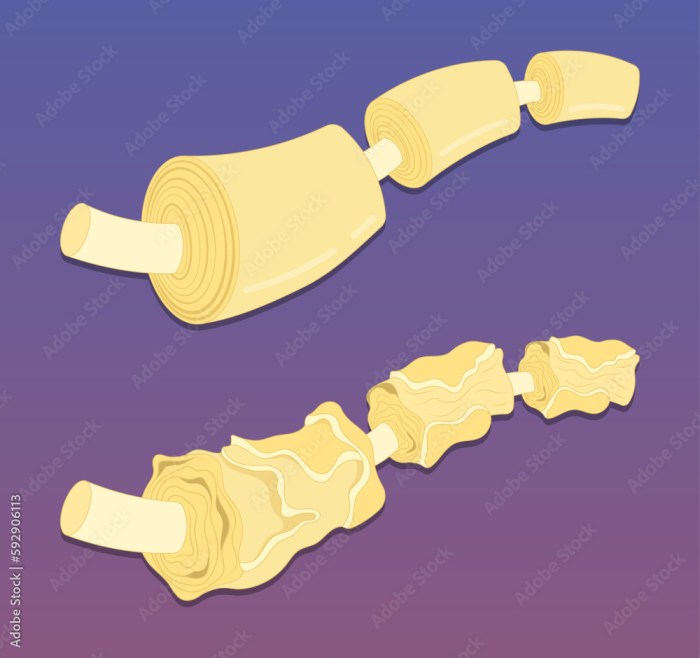
The fundamental difference lies in the mechanisms by which these diseases disrupt nerve-muscle communication. Myasthenia gravis targets the neuromuscular junction, the point where nerves connect to muscles. Autoimmune responses in MG lead to the disruption of acetylcholine receptors, crucial for muscle activation. In contrast, ALS directly affects motor neurons, the nerve cells responsible for controlling voluntary muscle movement.
This damage leads to progressive degeneration and eventual loss of these essential neurons. The resulting muscle weakness and paralysis are vastly different in nature and progression.
Clinical Manifestations: A Comparative Overview
The following table summarizes the key differences in symptoms and affected nerve pathways between MG and ALS:
| Disease Name | Symptoms | Affected Nerve Pathways |
|---|---|---|
| Myasthenia Gravis (MG) | Muscle weakness, typically affecting the eyes, face, neck, and limbs; fluctuating muscle weakness; improvement in muscle strength with rest, worsening with activity; double vision (diplopia), drooping eyelids (ptosis), difficulty swallowing (dysphagia), and difficulty speaking (dysarthria); fatigue. | Neuromuscular junction; the connection between nerves and muscles. The breakdown of acetylcholine receptors, which are critical for signal transmission, leads to weakness. |
| Amyotrophic Lateral Sclerosis (ALS) | Progressive muscle weakness and wasting; difficulty speaking, swallowing, and breathing; spasticity (stiffness) and/or fasciculations (twitching) in muscles; loss of coordination; cognitive decline in some cases. | Motor neurons, which control voluntary muscle movement; damage to these neurons results in the inability to signal muscles properly. The disease progressively destroys these essential neurons. |
Symptom Progression and Impact
The progression of symptoms in MG is often characterized by periods of exacerbation and remission. This fluctuating nature can make diagnosis challenging. In ALS, the progression is typically gradual and relentless, leading to a decline in functional abilities over time. While MG primarily affects muscle strength, ALS can cause significant difficulties with speech, swallowing, and breathing, ultimately impacting the patient’s ability to perform basic daily tasks.
Figuring out Myasthenia Gravis vs ALS can be tricky, but it’s important to understand the differences. While researching similar neurological conditions, I stumbled across an interesting comparison between silver diamine fluoride and sealants for teeth, which highlights the complexity of finding solutions in health care. This comparison to sliver diamine fluoride vs sealants made me realize that even seemingly disparate topics can share underlying themes of finding effective treatments.
Ultimately, the distinctions between Myasthenia Gravis and ALS remain crucial for accurate diagnoses and appropriate care.
Treatment Considerations
Treatment approaches for MG and ALS differ significantly. MG treatment focuses on modulating the autoimmune response, such as with immunosuppressants, to minimize the attack on the neuromuscular junction. In contrast, ALS treatment primarily aims to manage symptoms and slow the disease’s progression, as there is no known cure. Supporting respiratory function and maintaining quality of life are key considerations in the management of ALS.
Similarities and Differences
Understanding the similarities and differences between Myasthenia Gravis (MG) and Amyotrophic Lateral Sclerosis (ALS) is crucial for accurate diagnosis and effective management. While both diseases affect the nervous system, they do so through distinct mechanisms, leading to unique symptom profiles and disease trajectories. Distinguishing these nuances is vital for healthcare professionals and individuals affected by these conditions.
Symptom Overlaps and Variations
MG and ALS, though distinct, can present with some overlapping symptoms. Both can cause muscle weakness, fatigue, and difficulties with movement. However, the specific muscles affected and the nature of the weakness differ significantly. In MG, weakness often improves with rest, while in ALS, weakness tends to progress relentlessly. The presence of specific symptoms like double vision (diplopia) and difficulty swallowing (dysphagia) is more characteristic of MG.
Conversely, ALS typically involves progressive muscle atrophy and spasticity. Careful assessment of the symptom presentation, including the location and pattern of weakness, is critical for differential diagnosis.
Figuring out myasthenia gravis vs. ALS can be tricky, right? It’s important to understand the differences, but honestly, navigating the whole process can be overwhelming. If you’re facing chemo treatments, remember to check out primer tips before your first chemo treatment for some helpful advice. Ultimately, comparing the symptoms and potential treatments for myasthenia gravis and ALS can help you understand your own unique situation better.
Neurotransmitter and Pathway Involvement, Myasthenia gravis vs als
The fundamental mechanisms driving MG and ALS are different. MG targets the neuromuscular junction, the site where nerves communicate with muscles. Specifically, the immune system attacks acetylcholine receptors, which are essential for muscle contraction. This disruption hinders the transmission of signals, leading to muscle weakness. In contrast, ALS primarily affects motor neurons, the nerve cells responsible for controlling voluntary movements.
The degeneration of these neurons disrupts the communication pathway between the brain and muscles, leading to progressive muscle weakness and atrophy. This fundamental difference in affected pathways explains the distinct symptoms and disease progression.
Disease Progression
The progression of MG and ALS is not uniform. In MG, the disease can fluctuate in severity, with periods of remission and exacerbation. Factors like stress, infection, and medication can influence the disease’s course. The progression is typically more variable than in ALS. ALS, on the other hand, is characterized by a relentless, progressive decline in motor function.
While the rate of decline can vary between individuals, the overall trajectory is towards significant disability and ultimately, fatality. These differences in progression patterns necessitate different management strategies for each condition.
Symptom Severity and Progression Comparison
| Characteristic | Myasthenia Gravis (MG) | Amyotrophic Lateral Sclerosis (ALS) |
|---|---|---|
| Symptom Onset | Variable, often insidious, with gradual progression of symptoms. | Gradual, but often more rapid and significant progression, with noticeable symptoms. |
| Symptom Fluctuation | Symptoms can fluctuate significantly, with periods of remission and exacerbation. | Symptoms progress steadily and relentlessly, with no significant periods of remission. |
| Muscle Weakness | Weakness is often more prominent in specific muscle groups (e.g., ocular muscles, facial muscles). Weakness improves with rest. | Weakness progresses throughout the body, affecting muscles responsible for various movements. Weakness does not improve with rest. |
| Progression Rate | Can be variable, with some individuals experiencing slower progression and others faster. | Typically a more rapid and progressive decline in motor function, although rates can vary between individuals. |
| Life Expectancy | Variable, with many individuals living relatively normal lives with appropriate management. However, the disease can be severe. | ALS significantly shortens life expectancy, with average survival times ranging from 2-5 years from diagnosis. |
The table above provides a general comparison. Individual experiences can vary considerably. The table highlights the key distinctions in symptom presentation, progression rate, and overall impact on life expectancy.
Diagnosis and Treatment
Navigating the complexities of myasthenia gravis (MG) and amyotrophic lateral sclerosis (ALS) often hinges on accurate diagnosis and effective treatment strategies. Both conditions present unique challenges, demanding a multidisciplinary approach to manage symptoms and improve quality of life. Understanding the diagnostic pathways and available interventions is crucial for individuals and caregivers alike.
Diagnostic Procedures for MG and ALS
Diagnosing MG and ALS involves a combination of clinical evaluation, neurological examinations, and specific diagnostic tests. The diagnostic process for MG often starts with a detailed medical history, including symptom onset, progression, and any contributing factors. Physicians will perform a comprehensive neurological examination to assess muscle strength, reflexes, and cranial nerve function. Key diagnostic tests for MG include electromyography (EMG), which evaluates the electrical activity of muscles, and repetitive nerve stimulation, which measures the response of muscles to repeated nerve stimulation.
In ALS, the diagnosis often relies on a thorough neurological evaluation, including assessments of muscle strength, reflexes, and motor function. Furthermore, electromyography (EMG) and nerve conduction studies (NCS) help pinpoint the characteristic pattern of nerve and muscle degeneration. Neuroimaging, like MRI, may be used to rule out other conditions.
Treatment Options for MG
Managing MG involves a multifaceted approach targeting the underlying autoimmune response. Medications, therapies, and supportive care are integral components of the treatment plan. Medications commonly used include acetylcholinesterase inhibitors, which enhance the action of acetylcholine at the neuromuscular junction, and corticosteroids, which suppress the immune response. Plasmapheresis, a procedure that removes antibodies from the blood, is sometimes used to reduce symptoms during acute exacerbations.
Immunosuppressants may be prescribed in more severe cases to control the immune response. Physical therapy and occupational therapy are often crucial for maintaining mobility and independence, while speech therapy can aid communication if swallowing or speech is affected.
Treatment Options for ALS
ALS, a progressive neurodegenerative disease, currently lacks a cure. Treatment focuses on managing symptoms and slowing disease progression. Medications like riluzole, which may potentially slow disease progression, are often prescribed. Physical therapy, occupational therapy, and speech therapy play vital roles in maintaining functional abilities as the disease progresses. Supportive care, including nutritional support, respiratory management, and pain management, is crucial for maintaining the patient’s overall well-being.
Innovative therapies, such as gene therapy and stem cell treatments, are under investigation, offering potential avenues for future treatment.
While researching myasthenia gravis versus ALS, I stumbled upon the fascinating world of DMARDs for rheumatoid arthritis. These medications, like DMARDs for rheumatoid arthritis , target the underlying inflammation in the body, a concept that can surprisingly be relevant to understanding the differences in these neurological conditions. Ultimately, the differences between myasthenia gravis and ALS remain quite distinct, highlighting the complexities of neurological diseases.
Comparison of Treatment Efficacy and Side Effects
The efficacy and side effects of treatments vary between MG and ALS. Acetylcholinesterase inhibitors are generally well-tolerated in MG, though some patients experience gastrointestinal side effects. Corticosteroids, while effective in suppressing the immune response, can lead to a range of side effects, including osteoporosis, weight gain, and increased risk of infections. Plasmapheresis, while potentially effective, can be associated with complications like blood clots and infections.
In ALS, riluzole, the most commonly used medication, may slightly slow disease progression but is not a cure. Side effects of riluzole can include gastrointestinal issues, liver problems, and fatigue. Supportive care strategies, while not directly treating the underlying disease, significantly improve quality of life.
Diagnostic Tests, Treatments, and Expected Outcomes
| Disease | Diagnostic Tests | Treatments | Expected Outcomes |
|---|---|---|---|
| Myasthenia Gravis | Medical history, neurological examination, EMG, repetitive nerve stimulation | Acetylcholinesterase inhibitors, corticosteroids, plasmapheresis, immunosuppressants, physical therapy, occupational therapy, speech therapy | Symptom management, improved quality of life, reduced disease flares |
| Amyotrophic Lateral Sclerosis | Medical history, neurological examination, EMG, nerve conduction studies, neuroimaging (if needed) | Riluzole, physical therapy, occupational therapy, speech therapy, supportive care | Slowing disease progression, symptom management, improved quality of life |
Impact on Daily Life
Living with myasthenia gravis (MG) or amyotrophic lateral sclerosis (ALS) significantly alters daily routines and lifestyles. These debilitating neurological conditions impact not only physical abilities but also emotional well-being and social interactions. The unpredictable nature of symptoms, coupled with progressive functional decline, demands a multifaceted approach to support and management.Understanding the challenges faced by individuals with MG and ALS is crucial to developing appropriate support systems and interventions.
This includes recognizing the impact on personal independence, social connections, and emotional resilience. Furthermore, recognizing the variety of assistive technologies available can empower individuals to maintain their quality of life and independence.
Daily Activities and Lifestyle Changes
The progressive nature of both MG and ALS leads to gradual but significant changes in daily activities. Individuals with MG may experience fluctuating muscle weakness, impacting tasks like dressing, eating, and bathing. ALS, characterized by the progressive degeneration of motor neurons, results in the loss of voluntary muscle control. This leads to difficulty with everyday movements, including walking, speaking, and swallowing.
These challenges can impact a person’s ability to work, attend social events, and engage in hobbies.
Social and Emotional Challenges
Living with MG and ALS can be isolating. The unpredictable nature of symptoms and the progressive loss of function can lead to feelings of frustration, anxiety, and depression. Changes in physical appearance and communication abilities can also impact social interactions and relationships. Fear of judgment or misunderstanding from others can contribute to feelings of isolation.
Assistive Devices and Support Systems
Numerous assistive devices and support systems are available to help individuals with MG and ALS maintain independence and quality of life. These resources are crucial for managing the challenges of daily living. A comprehensive support system involves not only physical aids but also emotional and social support.
Assistive Technologies for Daily Tasks
A structured approach to managing daily tasks is vital. Various assistive technologies are available, ranging from simple tools to complex systems. These technologies help to compensate for lost functions and maintain independence. These technologies range from simple to sophisticated.
| Type of Assistive Technology | Application for Managing Daily Tasks |
|---|---|
| Adaptive eating utensils | Help with eating and drinking when hand dexterity is impaired. Examples include weighted utensils, adaptive cups, and plates. |
| Wheelchairs and mobility aids | Facilitate movement and mobility when walking becomes difficult or impossible. Different types, from basic wheelchairs to power-assisted mobility devices, are available. |
| Communication aids | Assist with communication when speech or writing becomes challenging. This includes speech-generating devices, communication boards, and augmentative and alternative communication (AAC) systems. |
| Adaptive clothing systems | Help with dressing, dressing-assisting devices, dressing systems, and specially designed clothing. |
| Home modifications | Adjusting the home environment to suit the individual’s needs, such as ramps, grab bars, and adapted bathroom fixtures. |
| Assistive technology for personal care | Assist with activities like bathing, showering, and toileting. Examples include grab bars, adaptive shower chairs, and raised toilet seats. |
Research and Future Directions: Myasthenia Gravis Vs Als
Unraveling the mysteries of myasthenia gravis (MG) and amyotrophic lateral sclerosis (ALS) hinges on ongoing research. Scientists are actively pursuing various avenues to enhance our understanding of these debilitating diseases, ultimately aiming to improve diagnostic accuracy and develop more effective treatments. This exploration encompasses a wide range of strategies, from fundamental research into disease mechanisms to clinical trials evaluating novel therapies.
The importance of this ongoing research cannot be overstated; it represents our collective hope for a brighter future for those affected by these conditions.
Current Research Efforts
Research into MG and ALS is multifaceted, spanning basic science investigations to clinical trials. Fundamental research aims to identify the underlying causes and mechanisms driving disease progression. This involves studying the intricate interplay of immune cells, nerve cells, and muscle fibers in MG, and the complex neuronal pathways and protein aggregation in ALS. Clinical trials, on the other hand, focus on evaluating the safety and efficacy of new therapies, ranging from immunomodulatory drugs to novel gene therapies.
Potential Avenues for Future Research
Future research efforts should prioritize strategies that enhance diagnostic accuracy and lead to more effective treatment outcomes. This includes developing more sensitive and specific diagnostic tools, such as blood tests or imaging techniques, that can identify MG and ALS earlier and more accurately. Moreover, exploring novel therapeutic targets, beyond those currently in use, is crucial. This might involve targeting specific immune pathways in MG or identifying and neutralizing key proteins implicated in ALS-related neuronal damage.
The development of personalized medicine approaches tailored to individual patient characteristics, such as genetic profiles and disease severity, could also prove transformative.
Importance of Ongoing Research and Clinical Trials
Ongoing research and clinical trials are vital for advancing our understanding of MG and ALS. Clinical trials are essential for evaluating the safety and efficacy of novel therapies, ensuring that promising treatments are rigorously tested before they are implemented in clinical practice. These trials also provide valuable data on the disease’s progression and response to different treatments, leading to better treatment strategies for individual patients.
Research provides the knowledge base that fuels innovation and drives the development of new and improved treatments, ultimately contributing to a better quality of life for those living with these conditions.
Key Areas of Research and Their Status
| Disease | Research Area | Current Status | Future Directions |
|---|---|---|---|
| Myasthenia Gravis (MG) | Immune system modulation | Significant progress in understanding the role of immune cells in MG. Current therapies focus on suppressing the immune response, but limitations exist. | Developing targeted therapies that modulate specific immune pathways, potentially minimizing side effects and improving efficacy. |
| Genetic factors | Research is uncovering genetic links to susceptibility to MG. Identifying specific genes and their roles will inform personalized medicine strategies. | Developing genetic tests for early detection and risk stratification. Identifying specific gene targets for therapeutic intervention. | |
| Novel diagnostic markers | Researchers are exploring new blood markers to facilitate earlier and more accurate diagnosis. Current tests have limitations. | Development of highly sensitive and specific diagnostic tests for early detection and monitoring of disease progression. | |
| Amyotrophic Lateral Sclerosis (ALS) | Neuroprotective therapies | Research into therapies to protect neurons from damage is ongoing. Current therapies primarily focus on slowing disease progression. | Development of therapies that can halt or reverse neuronal degeneration, rather than just slowing progression. |
| Genetic screening and testing | Genetic testing is becoming increasingly sophisticated, allowing identification of individuals at risk. | Further investigation into the genetic underpinnings of ALS to improve risk prediction and potentially identify targets for therapeutic intervention. | |
| Stem cell therapies | Studies are exploring the potential of stem cell therapies to replace or repair damaged nerve cells. Results are promising in animal models. | Further development and refinement of stem cell-based therapies, including improving efficacy and safety in clinical settings. |
Patient Support and Resources
Navigating the complexities of myasthenia gravis (MG) and amyotrophic lateral sclerosis (ALS) often requires more than medical expertise. Strong support systems are crucial for both patients and caregivers. These systems provide emotional, practical, and informational support, helping individuals cope with the challenges of these debilitating conditions. Finding the right resources can make a significant difference in the quality of life for those affected.Support is multifaceted, encompassing emotional well-being, practical assistance with daily tasks, and access to reliable information.
Effective support networks foster a sense of community and shared experience, allowing individuals to connect with others who understand the specific challenges they face.
Support Groups and Advocacy Organizations
Support groups offer a vital space for individuals with MG and ALS to connect with others experiencing similar challenges. These groups provide emotional support, practical advice, and a sense of belonging. Advocacy organizations play a crucial role in raising awareness, advocating for improved research, and promoting better access to resources. They often lobby for policies that benefit individuals with these conditions, increasing their visibility and influence.
Online and Offline Resources for Patients and Caregivers
Numerous online and offline resources are available to help patients and caregivers cope with MG and ALS. Online platforms, such as forums and support groups, provide accessible and convenient ways to connect with others and share experiences. Offline support groups, meetings, and workshops offer opportunities for in-person interaction and a more personal connection.
Organizations and Websites Offering Resources
- Myasthenia Gravis Foundation of America (MGFA): The MGFA provides comprehensive information on MG, including diagnosis, treatment, and support services. Their website offers educational materials, support groups, and a helpline for patients and caregivers.
- Amyotrophic Lateral Sclerosis Association (ALSA): The ALS Association is a leading resource for ALS information, offering a broad range of services, including research, caregiving support, and access to clinical trials. Their website provides a wealth of information on the disease and support for individuals.
- The Muscular Dystrophy Association (MDA): The MDA, though primarily focused on muscular dystrophy, also offers significant resources for ALS and MG. They often have regional chapters and programs that provide support to those affected.
- Patient advocacy groups on social media platforms: Facebook, Twitter, and other social media platforms often host support groups for MG and ALS patients, connecting individuals with similar experiences.
- Local chapters of support organizations: Many national organizations have local chapters that offer support groups, meetings, and workshops in specific regions.
- Websites of neurologists and healthcare professionals specializing in MG and ALS: These sites may provide valuable information on diagnosis, treatment, and managing symptoms.
Conclusion
In conclusion, while both myasthenia gravis and ALS present significant challenges, they are distinct neurological conditions with varying symptoms, mechanisms, and treatment approaches. Recognizing these differences is paramount for providing effective care and support. This comparison provides a crucial foundation for understanding these diseases and the need for continued research and compassionate care.