Gen Z weight stigma in medical settings survey aims to explore the unique experiences of young adults navigating healthcare. This survey delves into how weight bias manifests in doctor’s offices, impacting patient trust and potentially affecting health outcomes. We’ll examine the specific pressures Gen Z faces, contrasting these experiences with previous generations. Understanding these dynamics is crucial for creating more inclusive and effective healthcare systems.
The survey will investigate how weight stigma impacts Gen Z’s interactions with medical professionals, potentially leading to delayed or avoided care. We’ll analyze the sources of this stigma, from social media to personal encounters. Ultimately, the survey’s results will offer valuable insights into how healthcare providers can create a more supportive and equitable environment for this generation.
Defining Gen Z Weight Stigma
Gen Z, born between the mid-1990s and the early 2010s, is a generation deeply connected to technology and social media. This constant digital presence, alongside evolving societal norms, shapes their experiences with weight stigma in unique ways. Understanding this stigma requires recognizing the specific pressures and values of this generation.Gen Z, more than previous generations, values authenticity and self-expression.
However, this desire for self-acceptance can be complicated by the pervasive pressure to conform to unrealistic beauty standards. This generation’s emphasis on mental and physical well-being is often intertwined with a desire to present a curated online persona, potentially exacerbating feelings of inadequacy related to weight.
Characteristics of Gen Z and Weight Stigma
Gen Z is a generation that prioritizes mental and physical well-being, yet faces unique pressures related to weight. Their reliance on social media platforms creates a constant stream of images and messages that can influence body image perceptions. The rapid pace of social media interactions can contribute to feelings of pressure and comparison, potentially increasing susceptibility to weight stigma.
This pressure, coupled with a desire for authenticity, can lead to a complex interplay between self-acceptance and external pressures.
Sources of Weight Stigma for Gen Z
Several sources contribute to weight stigma for Gen Z. Media portrayals of idealized body types are ubiquitous, often perpetuating unrealistic expectations. Social norms, both online and offline, can create an environment where individuals feel judged or pressured to conform to specific weight standards. Furthermore, personal experiences, including bullying or teasing, can leave lasting negative impacts on an individual’s self-perception.
Manifestations of Weight Stigma in Medical Settings
Weight stigma in medical settings for Gen Z can manifest in various forms. Healthcare professionals may unconsciously express bias, leading to insensitive or dismissive comments about a patient’s weight. Patients may feel judged or embarrassed, potentially leading to reluctance to seek medical attention or follow treatment plans. This stigma can negatively impact their overall health outcomes and well-being.
For example, a doctor might minimize a patient’s concerns about a health issue due to their weight, leading to delayed or inadequate care.
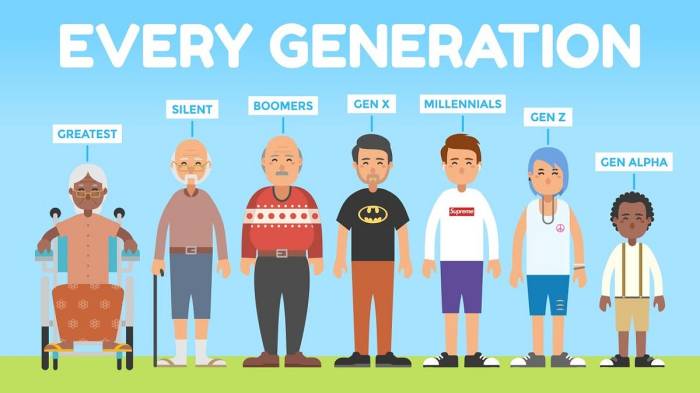
Comparison of Weight Stigma Across Generations
| Generation | Characteristics | Potential Sources of Stigma | Manifestations in Medical Settings |
|---|---|---|---|
| Millennials | Emphasis on health and wellness, but also social media influence. | Media portrayals, social norms, and pressure to conform to appearance standards. | Potential for weight-based bias from healthcare professionals, and reluctance to seek care. |
| Gen X | More emphasis on self-reliance and individuality. | Media portrayals, societal expectations of success. | Potential for judgments based on weight, and less emphasis on mental health aspects of weight. |
| Gen Z | Prioritizes authenticity and self-expression, heavily influenced by social media. | Media portrayals, social norms (especially online), and potential for cyberbullying based on weight. | Increased risk of insensitive comments or dismissive attitudes from healthcare providers, reluctance to disclose weight-related concerns. |
Experiences in Medical Settings
Navigating the healthcare system can be challenging for anyone, but for Gen Z individuals, the experience can be further complicated by the presence of weight stigma. This stigma manifests in various ways during medical consultations, impacting trust and potentially hindering the pursuit of optimal health outcomes. This section will delve into the common experiences of Gen Z patients facing weight bias in medical settings.Medical professionals, despite their best intentions, may unintentionally perpetuate weight stigma through subtle yet impactful behaviors.
This can range from dismissive comments to focusing solely on weight-related concerns, neglecting other important health factors. Such interactions can undermine the patient-physician relationship and negatively affect the overall healthcare experience.
Common Experiences of Weight Stigma
Gen Z individuals frequently report feeling judged or dismissed during medical consultations due to their weight. This can manifest as doctors spending less time discussing concerns, emphasizing weight loss over other health issues, or minimizing the seriousness of conditions related to weight. These experiences often lead to feelings of frustration, anxiety, and distrust. For instance, a Gen Z patient seeking treatment for a recurring headache might feel their concerns brushed aside if the doctor primarily focuses on their weight, potentially missing crucial underlying health issues.
That recent survey on Gen Z weight stigma in medical settings got me thinking. It’s a serious issue, especially when it comes to navigating health conditions like ulcerative colitis. Finding the right diet can be tough, and understanding what to eat if you have ulcerative colitis is crucial for managing symptoms. For detailed advice on this, check out this helpful resource: what to eat if you have ulcerative colitis.
Ultimately, the survey highlights how important it is for medical professionals to approach patients with sensitivity and avoid perpetuating harmful biases based on weight.
Examples of Insensitive or Biased Interactions
Examples of insensitive or biased interactions include a doctor minimizing a patient’s concerns about chronic pain by attributing it to their weight, or a doctor making assumptions about a patient’s lifestyle based solely on their body shape. A patient with high blood pressure might find their doctor focusing on weight loss as the primary solution rather than exploring other contributing factors like genetics or stress.
These interactions can be detrimental, potentially leading to a lack of engagement and delayed or avoided medical care.
Impact on Patient Trust and Engagement
Weight stigma during medical consultations can significantly damage patient trust and engagement with the healthcare system. Feeling judged or misunderstood can lead to a reluctance to discuss health concerns openly and honestly. Gen Z patients may be less likely to seek preventative care or follow-up appointments, potentially exacerbating existing health conditions or hindering the early detection of serious illnesses.
The recent survey on Gen Z weight stigma in medical settings is raising some serious questions. It’s fascinating to consider how this plays out in the context of, say, neuro intensive care units , where patients often face complex medical needs. Ultimately, these findings highlight the crucial need for a more nuanced and understanding approach to healthcare for Gen Z, especially when addressing sensitive issues like weight.
Patients may also feel discouraged from disclosing personal information, further hindering the doctor-patient relationship.
Potential Consequences for Health Outcomes
The consequences of weight stigma for Gen Z patients’ health outcomes can be severe. The emotional distress caused by these experiences can lead to increased stress hormones, impacting the body’s overall functioning. This emotional toll can also hinder the effectiveness of treatments for existing health conditions, or even deter Gen Z patients from seeking care in the first place.
A patient experiencing anxiety about their weight might be less likely to engage in healthy behaviors or seek appropriate medical attention.
Correlation Between Weight Stigma and Delayed/Avoided Care
| Weight Stigma Experience | Potential Impact on Care | Examples |
|---|---|---|
| Doctor focuses solely on weight loss, dismissing other concerns | Delayed diagnosis or treatment of underlying health conditions | A patient with high blood pressure experiences weight loss being emphasized over addressing underlying conditions, potentially delaying the diagnosis of other contributing factors. |
| Feeling judged or disrespected during consultations | Reduced trust in the healthcare system, reluctance to seek care | A patient feeling judged during a consultation might be less likely to seek preventative care or follow up on crucial health concerns, delaying treatment for an emerging health condition. |
| Doctor makes assumptions about lifestyle based on appearance | Misunderstanding of patient’s needs and health concerns | A patient with a history of dietary restrictions might be misjudged by a doctor who assumes a specific lifestyle without proper inquiry, leading to a misunderstanding of the patient’s individual needs. |
| Doctor’s lack of empathy and understanding | Reduced patient engagement and adherence to treatment plans | A patient experiencing emotional distress from weight-related comments might be less likely to follow medical advice, potentially hindering their recovery process. |
“Weight stigma in healthcare can lead to a vicious cycle where patients avoid care, leading to worse health outcomes, which in turn reinforces the negative perception of weight.”
Survey Design Considerations: Gen Z Weight Stigma In Medical Settings Survey
Crafting a survey on weight stigma in medical settings for Gen Z requires careful consideration to ensure its effectiveness in capturing nuanced experiences and perspectives. This involves understanding the specific challenges and sensitivities this generation faces within healthcare environments. A well-designed survey will offer valuable insights into the prevalence and impact of weight stigma, potentially leading to meaningful changes in healthcare practices.Understanding the intricacies of weight stigma and its impact on Gen Z’s healthcare experiences is crucial for designing a survey that effectively captures their perspectives.
This generation is highly digitally savvy, with strong opinions on societal issues. They are also very aware of the importance of representation and inclusivity. A survey must be sensitive to these aspects while providing a safe and anonymous space for participants to share their experiences.
Necessary Components for a Survey
A comprehensive survey to assess weight stigma in medical settings for Gen Z should include several key components. These components will allow for a thorough understanding of the issue and will also help to generate actionable insights. It’s essential to incorporate elements that address the specific experiences and perspectives of this demographic.
- Clear Definitions of Weight Stigma: A clear definition of weight stigma, as perceived by Gen Z, should be included in the survey. This allows participants to understand the survey’s focus and answer questions accurately and with a shared understanding.
- Specific Gen Z Experiences: The survey must specifically target Gen Z’s experiences with weight stigma within healthcare settings. This involves incorporating questions that probe their perceptions of how weight is addressed by doctors, nurses, and other healthcare professionals.
- Open-Ended Questions: Including open-ended questions allows participants to provide detailed accounts of their experiences. This qualitative data will offer a deeper understanding of the context and nuances of weight stigma.
- Contextual Factors: The survey should also consider factors such as the patient’s gender, ethnicity, and socioeconomic background. Understanding these contexts is important for identifying any potential disparities in the experience of weight stigma.
Examples of Survey Questions
These examples illustrate the types of questions that could be included in the survey to capture Gen Z’s perspectives. The questions are designed to be sensitive and respectful, ensuring a safe space for participants to share their experiences.
- “Have you ever felt that a healthcare professional treated you differently due to your weight?” This is a straightforward question that targets a key aspect of weight stigma. It is followed by multiple choice options allowing for more nuanced answers.
- “How comfortable are you discussing your weight with a healthcare provider?” This question employs a Likert scale to gauge the level of comfort participants feel when discussing their weight with a healthcare professional. Options range from “Very Uncomfortable” to “Very Comfortable.”
- “Describe a specific situation where you felt weight stigma in a medical setting.” This open-ended question allows participants to provide a detailed description of their experience, offering valuable qualitative data.
Question Types, Gen z weight stigma in medical settings survey
Using a variety of question types enhances the survey’s ability to gather comprehensive data.
- Multiple Choice: Provides structured options for participants to select from, facilitating data analysis. These questions can cover specific situations or attitudes.
- Likert Scale: Measures the strength of agreement or disagreement with a statement on a scale. This question type is useful for assessing attitudes and perceptions related to weight stigma.
- Open-Ended Questions: Allows for free-form responses, offering rich qualitative data. These questions encourage participants to elaborate on their experiences.
Ensuring Reliability and Validity
To ensure the survey’s reliability and validity, rigorous steps are essential. A pilot study with a smaller group of Gen Z participants can be used to identify any ambiguities in the questions and improve the survey’s clarity and comprehensiveness.
- Pilot Testing: Conducting a pilot study with a representative sample of Gen Z participants can help identify any ambiguities or areas where questions need clarification.
- Peer Review: Seeking feedback from experts in the field of weight stigma and survey design can enhance the survey’s reliability and validity.
- Data Analysis: Statistical methods will be used to analyze the data and identify patterns and trends related to weight stigma. This includes the use of descriptive statistics, correlation analysis, and regression analysis.
Potential Survey Question Categories
This table Artikels potential categories for the survey questions. Each category focuses on different aspects of weight stigma in medical settings.
| Category | Description |
|---|---|
| Experiences with Weight-Based Interactions | Questions related to how participants perceive their treatment in medical settings due to their weight. |
| Perceptions of Healthcare Professionals | Questions about participants’ views on healthcare professionals’ attitudes towards weight. |
| Comfort Levels and Communication | Questions focusing on participants’ comfort discussing weight with healthcare providers. |
| Impact on Health Outcomes | Questions related to how weight stigma affects their health-seeking behaviors and overall well-being. |
Impact and Implications
Weight stigma, unfortunately, isn’t a new problem, but its impact on Gen Z in medical settings deserves specific attention. This generation, digitally connected and often outspoken, is facing a unique set of pressures related to body image and health, and this experience is significantly shaped by their interactions with healthcare professionals. Understanding the potential consequences of this stigma is crucial for improving healthcare accessibility and outcomes for all.The impact of weight stigma on Gen Z’s mental health and overall well-being is significant.
Negative interactions with healthcare providers can lead to feelings of shame, isolation, and reduced trust in the medical system. This, in turn, can discourage individuals from seeking preventative care, delaying diagnosis and treatment of underlying health conditions. A lack of empathy and culturally sensitive care can create barriers to receiving appropriate medical advice, especially concerning weight management or weight-related health issues.
Mental Health and Well-being
Weight stigma often leads to psychological distress in Gen Z. The pressure to conform to societal beauty standards, coupled with negative feedback from healthcare professionals, can negatively impact self-esteem and body image. This can manifest in anxiety, depression, and eating disorders. For instance, studies have shown a correlation between weight-based discrimination and increased rates of depression and anxiety in young adults.
The recent Gen Z weight stigma in medical settings survey highlights some serious concerns about how healthcare professionals approach patient weight. It’s fascinating how this connects to the potential health implications of different elements, like sulfur, for example. Learning more about sulfur’s role in the body might provide some interesting insights into how we can better understand and address these issues.
Sulfur what should I know about it is a good resource for anyone wanting to dive deeper into this. Ultimately, the goal of these studies is to help improve patient care and address bias in medical settings.
This is particularly concerning given the already prevalent mental health challenges among Gen Z. The stress of navigating medical settings with weight bias can exacerbate these existing issues.
Implications for Healthcare Systems and Policies
Weight stigma negatively impacts healthcare systems by hindering effective care. Patients who experience bias may be less likely to adhere to treatment plans, leading to poorer health outcomes and increased healthcare costs in the long run. Moreover, this stigma can lead to underdiagnosis of underlying health conditions, as providers might overlook crucial symptoms due to preconceived notions about patients’ weight.
A focus on providing culturally sensitive care is vital for promoting trust and effective communication between patients and providers.
Impact Across Medical Specialties
The impact of weight stigma varies across different medical specialties. In primary care, it might lead to patients avoiding routine checkups or feeling uncomfortable discussing weight-related concerns. In specialties like cardiology or endocrinology, where weight is a crucial factor in diagnosis and treatment, stigma can hinder accurate assessment and effective management. In obstetrics and gynecology, the impact on a patient’s mental well-being during pregnancy or postpartum care can be detrimental.
Furthermore, weight bias can disproportionately affect marginalized communities, who may already face systemic health disparities.
Role of Cultural Factors
Cultural factors significantly shape weight stigma experiences for Gen Z. Different cultures have varying norms and perceptions of body size and weight, which can influence how patients perceive their weight and how healthcare professionals interact with them. For instance, in some cultures, there might be greater emphasis on maintaining a certain body type, potentially leading to heightened anxiety and pressure related to weight concerns.
Cultural sensitivity in healthcare is paramount to understanding these diverse experiences and providing equitable care.
Potential Solutions to Mitigate Weight Stigma
| Solution | Description |
|---|---|
| Training for Healthcare Professionals | Comprehensive training programs focusing on cultural competency, implicit bias awareness, and effective communication techniques can equip healthcare providers with the tools to address weight-related concerns in a sensitive and non-judgmental manner. |
| Patient-Centered Care | Promoting a patient-centered approach emphasizes active listening, open communication, and shared decision-making between patients and providers. This can foster trust and encourage patients to openly discuss their concerns. |
| Addressing Implicit Bias | Implementing strategies to address implicit bias within healthcare systems can significantly improve the quality of care provided to individuals with weight concerns. This can involve creating standardized guidelines for evaluating patient needs, regardless of weight. |
| Promoting Body Positivity | Encouraging body positivity and acceptance in media and within healthcare settings can contribute to a more supportive environment for individuals of all weights. |
| Policy Changes | Policy changes aimed at reducing weight bias in healthcare can be implemented at both local and national levels. Examples could include mandates for weight-neutral language in medical records or protocols. |
Survey Data Analysis
Unraveling the complexities of weight stigma requires a meticulous approach to analyzing survey data. This process involves more than just counting responses; it necessitates a strategic application of statistical methods to identify patterns, trends, and correlations. Careful interpretation of these findings is crucial to understand the experiences of Gen Z in medical settings and inform interventions aimed at reducing weight bias.A well-structured analysis provides insights into the nuanced ways weight stigma manifests in medical encounters, offering a roadmap for targeted interventions.
This involves not only quantifying the prevalence of stigma but also exploring the relationships between various factors, such as the perceived severity of weight stigma, patient demographics, and the types of medical interactions.
Statistical Methods for Analysis
Understanding the nuances of weight stigma requires a multifaceted approach to data analysis. Various statistical methods can be employed to discern patterns and trends.
- Descriptive statistics, such as frequencies and percentages, provide a foundational understanding of the distribution of responses to survey questions. This allows for a quick overview of the prevalence of specific experiences, enabling a preliminary assessment of weight stigma.
- Inferential statistics, including t-tests and ANOVA, allow for comparisons between groups (e.g., patients who report high levels of weight stigma versus those who report low levels). This enables the exploration of potential relationships between demographic characteristics and experiences of weight stigma.
- Correlation analysis can help reveal the strength and direction of relationships between different variables. For instance, it can determine if there’s a correlation between the perceived severity of weight stigma and the patient’s satisfaction with their medical care.
- Regression analysis delves deeper by identifying the predictive factors of weight stigma. For example, it can help determine whether specific patient characteristics (e.g., gender, race, or socioeconomic status) are associated with greater or lesser experiences of weight stigma.
Interpreting Survey Results in the Context of Weight Stigma
Interpreting survey results requires a contextual understanding of weight stigma. The analysis must consider the social, cultural, and medical contexts surrounding weight-related interactions.
- Survey results should be triangulated with existing research on weight stigma, healthcare disparities, and patient experiences. This validation process strengthens the conclusions and adds depth to the analysis.
- Qualitative data, such as open-ended questions, should be incorporated into the analysis to provide richer insights into the lived experiences of Gen Z. This allows for a deeper understanding of the complexities of weight stigma beyond quantitative data.
- The interpretation should avoid generalizations and acknowledge the diversity of experiences within the sample population. Understanding the specific ways different groups within Gen Z are affected by weight stigma is vital.
Significance of Survey Results for Interventions
The findings from a well-executed survey can be instrumental in developing targeted interventions to reduce weight stigma in medical settings.
- Identifying specific areas of concern, such as particular medical professionals or types of interactions that perpetuate weight stigma, allows for the development of focused strategies to address these issues.
- Understanding the prevalence of specific experiences enables the development of effective educational programs for medical professionals and patients. For instance, identifying that patients feel judged or dismissed in relation to their weight can help develop training programs on appropriate communication and patient-centered care.
- The results can inform policy changes and guidelines for healthcare providers, aiming to promote a more equitable and respectful environment for all patients.
Potential Statistical Results
The following table presents hypothetical results illustrating how statistical analysis might reveal patterns related to weight stigma. These are examples and not actual data.
| Survey Question | Potential Statistical Result | Interpretation |
|---|---|---|
| “How often do you feel judged by healthcare professionals about your weight?” | 75% of respondents reported feeling judged “sometimes” or “often.” | Weight stigma is prevalent among respondents, suggesting a need for training healthcare professionals on appropriate communication regarding weight. |
| “Did you feel your weight affected your treatment recommendations?” | 40% of respondents answered yes. | A significant portion of respondents perceived their weight as influencing their treatment plan, which can point to a need for policy changes that promote equitable care. |
| “How satisfied were you with the doctor’s communication about weight?” | Mean score of 2.5 out of 5. | A low satisfaction score indicates that communication regarding weight could be improved, potentially through training and guidelines on the topic. |
Illustrative Case Studies

Navigating the healthcare system can be challenging enough without the added layer of weight bias. Gen Z individuals, particularly those navigating medical settings, often experience implicit and explicit weight-based discrimination, which can significantly impact their health outcomes and well-being. This section will delve into illustrative case studies, highlighting the experiences of Gen Z patients and the potential biases they encounter.
Understanding these scenarios is crucial for creating more equitable and supportive medical environments.This exploration of real-life and hypothetical situations aims to shed light on the pervasive nature of weight stigma in medical settings. We will focus on how weight stigma can influence communication, potentially leading to misdiagnosis, inadequate treatment plans, and decreased patient trust.
Real-Life Scenarios of Weight Stigma
Weight bias in healthcare isn’t always overt; sometimes, it manifests in subtle, yet damaging, ways. Patients might feel dismissed or unheard, leading to a lack of open communication and potentially hindering effective treatment. For instance, a Gen Z patient seeking advice on a healthy lifestyle might feel their concerns are trivialized or their questions dismissed. A medical professional might focus more on weight management than on the patient’s primary concerns, potentially leading to a breakdown in trust and a lack of adequate care.
Hypothetical Encounters with Medical Professionals
Imagine a 20-year-old Gen Z patient, Sarah, who visits her doctor complaining of persistent back pain. Sarah, who is concerned about her weight, anticipates judgment from her doctor. During the appointment, the doctor might ask about Sarah’s diet and exercise habits, placing emphasis on weight loss rather than exploring the root causes of her back pain. This focus on weight could inadvertently shift the conversation away from the core issue, potentially delaying diagnosis or leading to a less comprehensive treatment plan.
Impact on Patient-Physician Communication
Weight stigma can severely hinder effective communication between patients and physicians. When patients feel judged or dismissed due to their weight, they might be less likely to disclose important information or ask clarifying questions. This can lead to inaccurate diagnoses, delayed treatments, and a decrease in patient satisfaction. Conversely, physicians might be inadvertently influenced by their own biases, leading to a less thorough evaluation of the patient’s condition.
Table Summarizing Case Studies
| Case Study | Patient Profile (Gen Z) | Medical Concern | Potential Weight Stigma | Impact on Communication |
|---|---|---|---|---|
| Sarah | 20-year-old female, concerned about weight | Back pain | Doctor focused on weight loss rather than root cause | Limited exploration of back pain, reduced trust |
| David | 19-year-old male, struggling with anxiety | Anxiety attacks | Doctor minimized anxiety symptoms due to perceived lifestyle factors | Dismissed concerns, decreased engagement in therapy |
| Emily | 22-year-old female, seeking advice on healthy eating | Dietary concerns | Doctor focusing on weight loss rather than nutritional guidance | Lack of support, feeling unheard, potential for poor dietary advice |
Outcome Summary
This survey on Gen Z weight stigma in medical settings will provide critical data to help address the significant issue of weight bias within healthcare. By understanding the experiences of this generation, we can work towards creating a more supportive and effective healthcare system for everyone. The findings will illuminate the need for improved training and awareness for medical professionals to reduce weight stigma and improve patient care.
Ultimately, this survey can serve as a catalyst for positive change in the way healthcare providers approach weight-related issues.