How to fall asleep fast is a common concern for many. This guide delves into proven techniques for achieving restful sleep quickly. We’ll explore relaxation strategies, optimize your sleep environment, and discuss sleep hygiene practices to help you drift off easily and wake up feeling refreshed.
From mastering mindfulness to understanding dietary impacts, this comprehensive guide offers practical advice and actionable steps to conquer insomnia and embrace a better night’s sleep.
Relaxation Techniques
Falling asleep quickly often hinges on effectively calming the mind and body. This involves employing various relaxation techniques that can help quiet the internal chatter and promote a state of deep rest. By incorporating these practices into your nightly routine, you can significantly improve your sleep quality and wake up feeling refreshed and rejuvenated.Effective relaxation techniques are crucial for establishing a healthy sleep hygiene routine.
They act as a bridge between your active day and the restorative sleep you need. Consistent practice helps to regulate your body’s natural sleep-wake cycle, making it easier to fall asleep and stay asleep throughout the night.
Ever struggle to fall asleep? Sometimes, seemingly unrelated things can affect your sleep. For example, if you’re noticing pinprick red dots on your skin that aren’t itchy, it could be a sign of something more serious. Check out this helpful resource on pinprick red dots on skin not itchy to understand potential causes. Regardless of the reason, consistent relaxation techniques like deep breathing and meditation can significantly improve your sleep quality and help you drift off to sleep faster.
Relaxation Techniques for Quick Sleep
Relaxation techniques can be powerful tools for sleep induction. They work by lowering your heart rate, reducing muscle tension, and quieting racing thoughts. By consistently employing these techniques, you can establish a regular sleep pattern, leading to improved sleep quality.
- Progressive Muscle Relaxation (PMR): This technique involves systematically tensing and releasing different muscle groups in your body. By consciously contracting and then releasing the tension, you become more aware of the physical sensations associated with relaxation. This awareness can help to quiet the mind and promote a sense of calm.
- Deep Breathing Exercises: Deep, slow breaths can have a profound effect on your body’s physiological response. By focusing on your breath, you can calm your nervous system and lower your heart rate. This can help you to transition into a state of deep relaxation, making it easier to fall asleep.
- Mindfulness Meditation: Mindfulness meditation encourages present moment awareness. By focusing on your breath, bodily sensations, and thoughts without judgment, you can detach from racing thoughts and anxieties. This non-judgmental awareness can promote a sense of calm and reduce stress, leading to improved sleep.
- Guided Imagery: Guided imagery involves creating a mental picture of a peaceful and calming scene. Through detailed descriptions of relaxing settings, you can mentally transport yourself to a serene environment. This can help to reduce stress and anxiety, promoting a state of relaxation conducive to sleep.
- Yoga and Stretching: Yoga and stretching routines can promote physical relaxation and reduce muscle tension. The gentle movements and stretching exercises help to release physical tension, creating a sense of calm and readiness for sleep. This physical relaxation often complements other mental techniques for better sleep induction.
Progressive Muscle Relaxation in Bedtime Routine
Progressive muscle relaxation (PMR) is a valuable technique for incorporating into a bedtime routine. By focusing on physical relaxation, PMR can effectively calm the mind and body, preparing you for sleep.To effectively incorporate PMR into your bedtime routine:
- Choose a quiet and comfortable space: Find a comfortable spot in your bedroom where you can lie down or sit without distractions.
- Begin with a few deep breaths: This will help to calm your nervous system and prepare your body for relaxation.
- Identify a muscle group: Start with your toes and progressively work your way up your body, tensing and releasing each muscle group.
- Hold the tension for a few seconds: Focus on the sensation of the tension in your muscles.
- Release the tension slowly: Notice the difference between the tense and relaxed state of the muscle group.
- Continue through all muscle groups: Repeat the process, gradually working through your entire body, from your toes to your head.
- Maintain a relaxed posture: Continue to breathe deeply and maintain a relaxed posture throughout the process.
- End with a final relaxation: Allow your body to remain completely relaxed, focusing on the sensations of deep rest.
Comparing Mindfulness Practices for Sleep
Mindfulness practices offer various approaches to sleep induction, each with unique strengths and weaknesses.
| Technique Name | Brief Description | Estimated Time Needed |
|---|---|---|
| Mindfulness Meditation | Focuses on present moment awareness without judgment, often using the breath as an anchor. | 10-20 minutes |
| Guided Imagery | Involves creating mental images of peaceful settings to promote relaxation. | 10-15 minutes |
| Progressive Muscle Relaxation | Systematically tenses and releases different muscle groups to reduce physical tension. | 15-20 minutes |
| Deep Breathing Exercises | Focuses on slow, deep breaths to calm the nervous system and reduce anxiety. | 5-10 minutes |
Guided Imagery for Sleep
Guided imagery is a powerful tool for sleep induction. It works by creating a mental escape from worries and anxieties, replacing them with a relaxing and peaceful scene.
- Choose a calming environment: Select a serene and peaceful setting, such as a beach, a forest, or a mountain meadow. Visualize the details of this environment, including sounds, smells, and textures.
- Create a vivid mental picture: Engage all your senses in creating a detailed and immersive mental image. Imagine the colors, shapes, and textures of the environment.
- Focus on the sensations: Pay attention to the sensations associated with this environment, such as the feeling of warmth, the sound of the waves, or the smell of fresh air.
- Stay present in the imagery: Continue to focus on your chosen imagery, letting your thoughts drift with the experience, letting go of any worries or anxieties.
- Gradually transition into sleep: Allow yourself to drift into a state of deep relaxation, allowing the imagery to guide you into sleep.
Creating a Conducive Sleep Environment
A crucial component of achieving restful sleep is establishing a sleep-conducive environment. Your bedroom should be more than just a place to sleep; it should be a sanctuary designed to promote relaxation and signal to your body that it’s time to unwind. Optimizing your bedroom’s atmosphere can significantly impact your sleep quality and overall well-being.A well-designed sleep environment sets the stage for a smooth transition into slumber.
Elements like lighting, temperature, and noise levels play a significant role in regulating your body’s natural sleep-wake cycle. By creating a calm and comfortable space, you can foster a more positive sleep experience.
Optimizing Bedroom Lighting for Sleep
Dimming the lights in the hours leading up to bedtime sends signals to your brain that it’s time to wind down. Exposure to bright light can suppress the production of melatonin, a hormone crucial for regulating sleep. Gradually reducing light intensity as the evening progresses helps prepare your body for sleep. Using warm-toned lighting, like soft yellow or orange bulbs, further contributes to a calming atmosphere.
Avoid harsh fluorescent lights or blue light-emitting devices (like tablets or smartphones) close to bedtime. The warm tones are more conducive to a relaxing mood and sleep initiation.
Essential Elements for a Sleep-Friendly Bedroom
Creating a truly sleep-friendly bedroom involves more than just darkness and quiet. Consider incorporating elements that promote relaxation and comfort. A comfortable mattress and pillows are essential for supporting your body throughout the night. Consider a breathable, soft bedding set that helps regulate temperature and enhances comfort. A relaxing scent like lavender can create a calming atmosphere.
A comfortable and supportive mattress and pillows are essential for proper spinal alignment and reducing discomfort during sleep. A soothing blanket or a weighted blanket can further enhance relaxation and provide a sense of security.
Creating a Comfortable Sleep Environment
A comfortable sleep environment is essential for promoting relaxation and initiating sleep. The bedroom should be a haven where you can easily unwind and transition into a state of readiness for sleep. Ensure the temperature is cool, the lighting is dim, and the noise levels are minimal. Incorporate elements that promote relaxation and comfort, such as comfortable bedding, soft lighting, and calming scents.
A sleep-friendly environment signals to your body that it’s time to rest, leading to a more positive sleep experience.
Ideal Conditions for a Sleep-Conducive Bedroom
| Factor | Ideal Range | Rationale |
|---|---|---|
| Temperature | 60-67°F (15.5-19.4°C) | A slightly cool room promotes better sleep than a warm room. Lower temperatures encourage the body to cool down, preparing it for sleep. |
| Noise Levels | Below 45 decibels (dB) | Excessive noise can disrupt sleep. Maintaining a quiet environment minimizes distractions and allows for deeper, more restful sleep. A quiet environment reduces stress and anxiety, promoting sleep. |
| Lighting | Dim and Warm-toned | Bright light can interfere with melatonin production, delaying sleep onset. Using warm-toned lighting creates a calming atmosphere, promoting relaxation and sleep initiation. Dim lighting signals to your body that it’s time to rest. |
Sleep Hygiene Practices
Establishing healthy sleep habits, often called sleep hygiene, is crucial for falling asleep quickly and waking up feeling refreshed. Consistent sleep hygiene practices create a predictable sleep-wake cycle, promoting optimal sleep quality. A regular sleep schedule, coupled with mindful choices regarding diet and activity, significantly impacts the ability to fall asleep easily and experience restorative sleep.Sleep hygiene practices encompass a range of behaviors that collectively influence sleep onset and duration.
These practices are not just about the immediate act of falling asleep, but about establishing a foundation for long-term sleep health. By adopting these habits, you can significantly improve your sleep quality and overall well-being.
Consistent Sleep Schedules
A regular sleep schedule, regardless of the day of the week, helps regulate the body’s natural sleep-wake cycle, also known as the circadian rhythm. This consistency signals to the body when it’s time to sleep and wake up, making it easier to fall asleep and wake up feeling rested. For example, a person who consistently goes to bed and wakes up at the same time each day, even on weekends, will often find it easier to fall asleep at night and wake up without an alarm clock.
Caffeine and Alcohol Consumption, How to fall asleep fast
Caffeine and alcohol, while seemingly unrelated, both have significant effects on sleep patterns. Caffeine, a stimulant, can interfere with sleep onset and quality, as its effects can linger for several hours after consumption. Consuming caffeine too close to bedtime can lead to difficulty falling asleep and restless nights. Alcohol, although initially it might seem to promote sleepiness, can disrupt sleep architecture later in the night, resulting in fragmented sleep and a less restorative experience.
Regular Exercise
Regular physical activity is beneficial for overall health, and it also plays a vital role in sleep quality. Exercise promotes better sleep onset and maintenance. Moderate-intensity exercise, such as brisk walking or cycling, can be particularly effective. However, avoid strenuous exercise too close to bedtime, as it may have the opposite effect, leading to alertness and difficulty falling asleep.
Examples include avoiding a strenuous workout in the hours leading up to sleep.
Pre-Sleep Routines
Establishing a calming pre-sleep routine can signal to the body that it’s time to wind down and prepare for sleep. Activities like taking a warm bath, reading a book, or practicing relaxation techniques can help ease the transition from wakefulness to sleep. These routines create a consistent signal, making it easier to fall asleep each night.
Impact of Pre-Sleep Activities on Sleep Quality
| Activity | Potential Impact | Recommended Time Frame |
|---|---|---|
| Taking a warm bath | Relaxing and promoting sleepiness due to the body temperature drop. | 1-2 hours before bedtime |
| Reading a book | Reduces mental stimulation, promoting relaxation. | 1-2 hours before bedtime |
| Light stretching | Reduces muscle tension, promoting relaxation. | 1-2 hours before bedtime |
| Listening to calming music | Reduces mental stimulation, promoting relaxation. | 1-2 hours before bedtime |
| Meditating | Promotes relaxation and reduces stress. | 1-2 hours before bedtime |
| Using electronic devices (e.g., phone, tablet) | Increased stimulation, potentially delaying sleep onset. | Avoid within 1 hour of bedtime |
| Heavy exercise | Increased alertness, potentially delaying sleep onset. | Avoid within 2-3 hours of bedtime |
Dietary Influences on Sleep

Your diet plays a crucial role in your sleep quality. What you eat and drink, and when you eat, can significantly impact your ability to fall asleep and stay asleep. Understanding these influences allows you to tailor your dietary habits to optimize your sleep.The foods and drinks we consume contain various compounds that can affect our bodies’ natural sleep-wake cycles.
Some promote relaxation and sleepiness, while others can interfere with the process. Understanding the timing of meals, especially the last meal of the day, is equally important for achieving restful sleep.
Impact of Specific Foods and Beverages
Certain foods and beverages can have a stimulating effect, making it harder to fall asleep. Caffeine, found in coffee, tea, and some sodas, is a well-known stimulant. Alcohol, while initially promoting drowsiness, can disrupt sleep later in the night, leading to fragmented sleep and reduced overall sleep quality. Spicy foods can also cause indigestion, which can interfere with sleep.
Sugary foods and drinks, while providing a temporary energy boost, can cause blood sugar fluctuations, impacting sleep quality.
Finding ways to quickly drift off to sleep can be tricky, especially when your mind races. One thing that can sometimes contribute to sleep problems is an underlying health condition like asthma. While some people might wonder if they can outgrow asthma, the answer isn’t always straightforward. For more information on this topic, check out this resource about can you outgrow asthma.
Regardless of whether you can outgrow asthma, practicing relaxation techniques, like deep breathing exercises, can help you fall asleep faster and improve your overall sleep quality.
Meal Timing and Sleep Onset
The timing of your meals, particularly the last meal before bed, significantly impacts your sleep onset. Consuming a large meal close to bedtime can lead to digestive discomfort and keep your body active, making it harder to relax and fall asleep. This is because your body’s digestive system is working hard, diverting energy and resources away from sleep preparation.
A light, easily digestible meal several hours before bed is generally recommended.
Adjusting Your Diet to Promote Sleep
To improve your sleep, focus on incorporating foods and beverages that promote relaxation and a sense of calm. Choose foods rich in tryptophan, an amino acid that helps regulate sleep hormones. Warm milk, for example, is often cited for its calming effects. Avoid or limit the consumption of stimulating substances like caffeine and alcohol close to bedtime.
Also, make sure your last meal of the day is light and easily digestible.
Foods and Beverages to Limit or Avoid
Here are some foods and beverages that can disrupt sleep, along with alternative choices that are sleep-friendly:
- Caffeine-containing beverages: Coffee, tea, sodas. Alternatives: Herbal teas, decaffeinated coffee, water.
- Alcohol: While it might initially induce drowsiness, it disrupts sleep later in the night. Alternatives: Herbal infusions, warm milk.
- Spicy foods: Can lead to indigestion and discomfort. Alternatives: Mildly spiced dishes, easily digestible meals.
- Sugary foods and drinks: Can cause blood sugar fluctuations. Alternatives: Fruits, complex carbohydrates.
Sleep-Promoting Foods and Beverages
The following table provides a list of sleep-promoting foods and beverages, their potential impact on sleep, and suggested quantities for optimal results.
| Food/Beverage | Potential Impact | Suggested Quantity |
|---|---|---|
| Warm milk | Calming, tryptophan-rich | 1-2 glasses |
| Bananas | Potassium-rich, promoting relaxation | 1-2 bananas |
| Chamomile tea | Calming, promotes relaxation | 1 cup |
| Oatmeal | Complex carbohydrates, promotes steady energy | 1/2 cup |
| Turkey | Tryptophan-rich | 3-4 ounces |
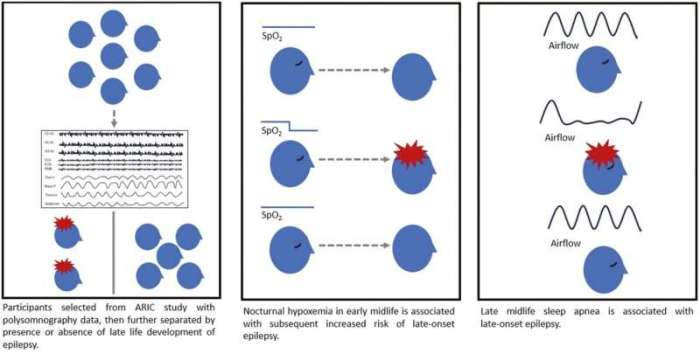
Addressing Underlying Sleep Disorders
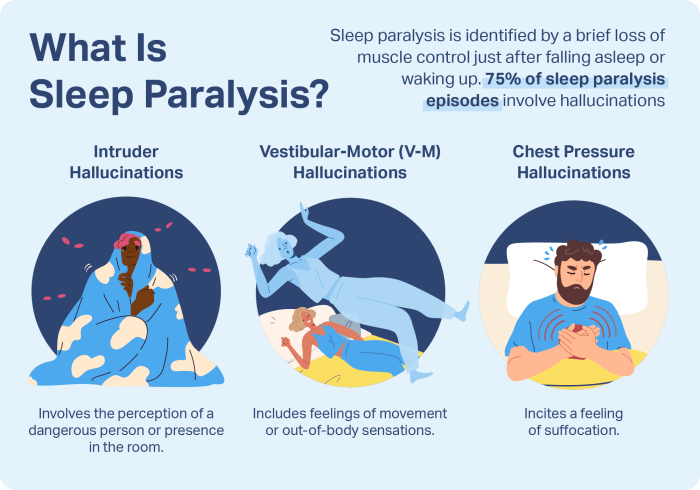
Sometimes, falling asleep quickly isn’t just about creating the right environment or practicing good sleep hygiene. Underlying sleep disorders can significantly impact your ability to nod off and enjoy restorative rest. Recognizing the signs and seeking professional help is crucial for overcoming these challenges and reclaiming your sleep.Understanding the different types of sleep disorders and their symptoms is essential for identifying potential issues.
Identifying a sleep disorder isn’t always straightforward, but a thorough evaluation by a healthcare professional can provide accurate diagnoses and tailored treatment plans. Knowing what to look for can help you determine if it’s time to seek expert advice.
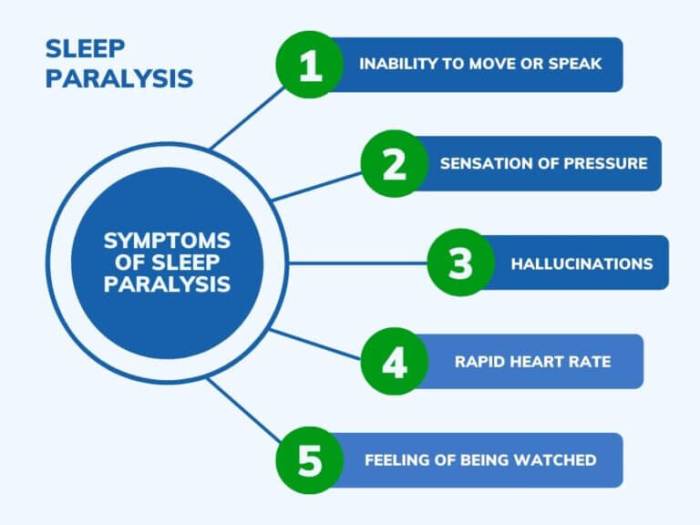
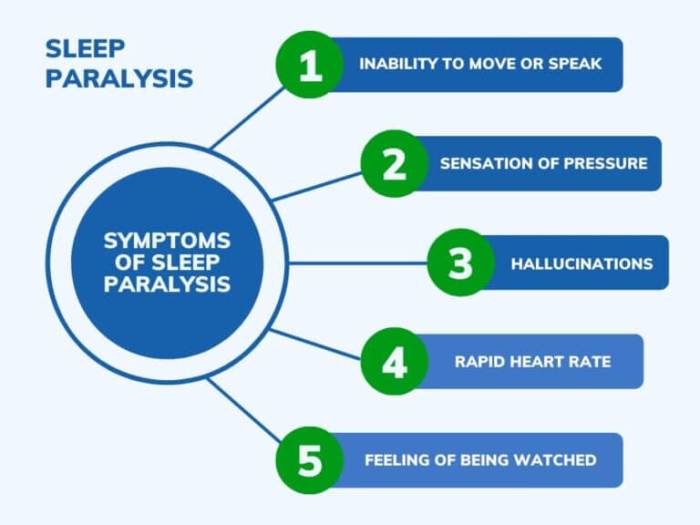
Common Symptoms of Sleep Disorders
Many sleep disorders share similar symptoms, making early identification challenging. It’s important to note that experiencing some of these symptoms doesn’t automatically mean you have a sleep disorder. However, if these issues persist or significantly affect your daily life, consulting a doctor is recommended.
Getting a good night’s sleep is key for overall well-being, and quick sleep is often a priority. One thing that can affect sleep quality is low blood pressure, which can be a factor in feeling tired. Understanding low blood pressure can help you better address potential sleep disruptions. For a comprehensive overview of low blood pressure, check out this helpful resource: low blood pressure overview.
Ultimately, if you’re struggling to fall asleep, making sure your blood pressure is within a healthy range could be a significant step toward a more restful night’s sleep.
- Difficulty falling asleep (insomnia): This is characterized by persistent trouble initiating sleep, often associated with racing thoughts or anxiety. A consistent pattern of difficulty falling asleep, even when conditions are optimal, may indicate an underlying issue.
- Waking up frequently during the night (insomnia): Frequent awakenings can disrupt sleep cycles, leading to fatigue and difficulty concentrating during the day. Repeated awakenings, even if short, can make it hard to achieve restful sleep.
- Difficulty staying asleep (insomnia): This involves consistently waking up too early or experiencing a reduced duration of sleep. If you consistently find yourself waking up before feeling well-rested, it may signal an underlying problem.
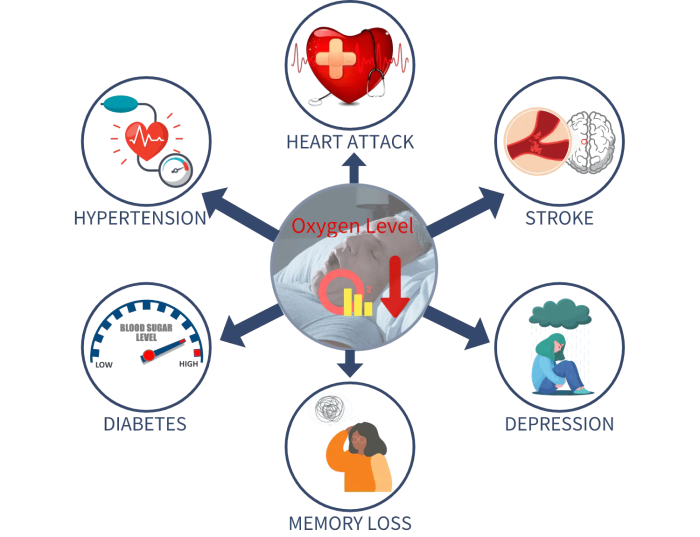
- Excessive daytime sleepiness: Feeling excessively tired and sleepy throughout the day, even after sufficient sleep, can be a sign of sleep apnea or other sleep disorders. Unintended lapses into sleep during the day, especially during mundane activities, could suggest a sleep-related issue.
- Snoring and/or pauses in breathing (sleep apnea): Loud snoring, accompanied by pauses in breathing, is a hallmark symptom of sleep apnea. This condition can lead to daytime sleepiness and various health complications. Loud snoring, coupled with pauses in breathing, can significantly affect sleep quality.
- Restless legs syndrome (RLS): This condition involves an irresistible urge to move the legs, often accompanied by unpleasant sensations. The urge to move the legs, often coupled with uncomfortable sensations, can disrupt sleep cycles and lead to fatigue.
Identifying Possible Sleep Disorders
A thorough sleep history, along with physical examinations and potentially sleep studies, are essential tools for identifying potential sleep disorders. Detailed information about your sleep patterns, lifestyle, and medical history can help a doctor identify potential underlying issues.
- Maintaining a sleep diary: A sleep diary can help track sleep patterns, noting the time you go to bed, wake up, and any difficulties encountered. Detailed records of your sleep patterns, including times of sleep onset, duration, and any disruptions, can provide valuable insights.
- Reporting symptoms to a healthcare professional: Open communication with your doctor about any sleep-related issues is crucial. Sharing detailed information about symptoms, sleep patterns, and any relevant medical history is vital for a proper diagnosis.
- Potential sleep studies: In some cases, a sleep study, also known as a polysomnography, may be recommended to monitor brain waves, breathing, and other physiological functions during sleep. A sleep study can measure various physiological functions during sleep, helping identify any underlying disorders.
Importance of Seeking Professional Help
Addressing sleep disorders with professional guidance is vital for effective treatment and overall well-being. Professional intervention is crucial for managing sleep disorders effectively and avoiding long-term health complications.
- Accurate diagnosis and tailored treatment: A healthcare professional can accurately diagnose the specific sleep disorder and develop a personalized treatment plan. A doctor can provide an accurate diagnosis and a tailored treatment plan specific to your needs.
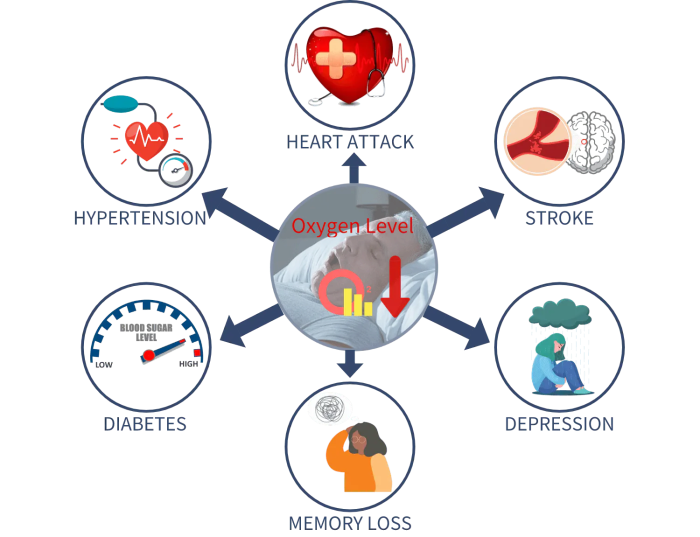
- Management of related health concerns: Some sleep disorders can contribute to other health problems, such as cardiovascular disease or diabetes. Addressing sleep disorders can help prevent or manage these related health issues.
- Improved quality of life: Effective treatment for sleep disorders can significantly improve your overall quality of life by promoting better physical and mental health. Addressing sleep disorders can lead to better overall physical and mental well-being.
Common Sleep Disorders
Several sleep disorders can significantly impact sleep onset and overall sleep quality. Recognizing these conditions is the first step toward seeking appropriate treatment.
- Insomnia
- Sleep apnea
- Restless legs syndrome (RLS)
- Narcolepsy
- Periodic limb movement disorder
Comparison of Sleep Disorders
| Disorder | Common Symptoms | Potential Treatments |
|---|---|---|
| Insomnia | Difficulty falling asleep, staying asleep, or waking up too early; fatigue, irritability, difficulty concentrating. | Cognitive behavioral therapy for insomnia (CBT-I), medication (in some cases), lifestyle changes. |
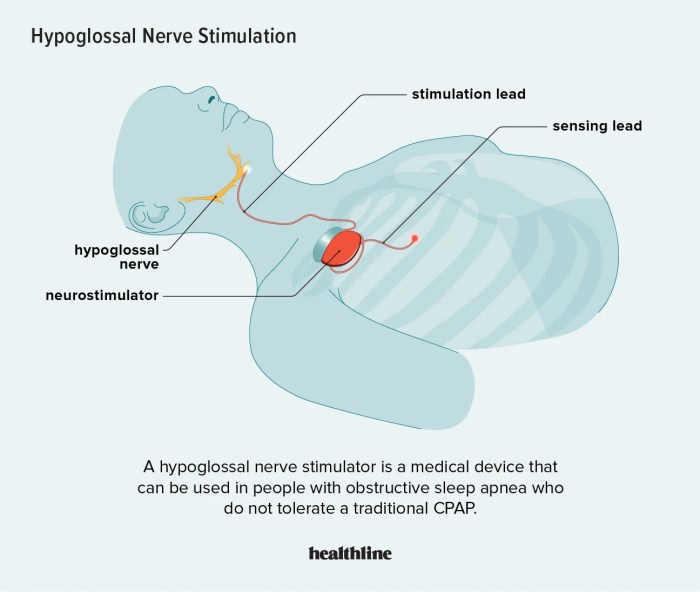
| Sleep Apnea | Loud snoring, pauses in breathing, gasping or choking during sleep; daytime sleepiness, morning headaches, irritability. | Continuous positive airway pressure (CPAP) therapy, lifestyle changes, surgery (in some cases). |
| Restless Legs Syndrome (RLS) | Irresistible urge to move legs, uncomfortable sensations in legs; difficulty falling asleep, frequent awakenings. | Medication, lifestyle changes, relaxation techniques. |
Cognitive Strategies for Sleep
Our thoughts can significantly impact our ability to fall asleep. Unresolved problems, worries, and racing thoughts often keep us tossing and turning, making it challenging to quiet the mind and drift off. Effective cognitive strategies can help manage these mental distractions and promote a more peaceful sleep experience.Cognitive strategies for sleep involve actively addressing and restructuring negative thought patterns that interfere with sleep.
By understanding how your thoughts affect your body’s natural sleep-wake cycle, you can develop techniques to regain control and improve sleep quality.
Managing Racing Thoughts
Racing thoughts, a common sleep disruptor, involve a rapid stream of thoughts that make it difficult to focus on anything else. Techniques to manage racing thoughts include mindfulness exercises and cognitive restructuring. Mindfulness involves focusing on the present moment without judgment, redirecting your attention away from the anxious thoughts. Cognitive restructuring involves identifying and challenging negative thought patterns. Replace anxious or worrisome thoughts with more balanced and realistic ones.
For example, instead of thinking “I’ll never get this presentation right,” try “I’ve prepared well, and I’m confident in my abilities.”
Challenging Negative Thoughts About Sleep
Negative thoughts about sleep can create a self-fulfilling prophecy, leading to increased anxiety and further sleep problems. Identifying these negative thoughts and actively challenging them is crucial. For instance, if you’re worried about not getting enough sleep, challenge that thought by acknowledging past instances where you slept well despite perceived challenges. Consider the possibility that your sleep might be better than you anticipate.
Recognizing and challenging negative thoughts helps to foster a more positive and realistic outlook regarding sleep.
The Importance of Positive Self-Talk
Positive self-talk plays a critical role in managing anxiety and promoting relaxation before bed. By replacing negative self-criticism with supportive and encouraging affirmations, you can create a more conducive mental state for sleep. For example, instead of saying “I’m so tired and I’ll never fall asleep,” try “I’m allowing myself to relax and my body is ready for sleep.” These affirmations create a sense of calm and control, encouraging a more positive approach to sleep.
Reducing Anxiety Before Bed
Anxiety before bed can be a major obstacle to sleep. Techniques for reducing anxiety include progressive muscle relaxation, deep breathing exercises, and creating a relaxing bedtime routine. Progressive muscle relaxation involves systematically tensing and releasing different muscle groups in the body, promoting physical relaxation. Deep breathing exercises can calm the nervous system, reducing feelings of stress and anxiety.
A relaxing bedtime routine, such as taking a warm bath or reading a calming book, can help signal to your body that it’s time to wind down.
Sample Script for Positive Self-Talk Exercise
“I am allowing my body to relax. My muscles are releasing tension. My breath is calm and steady. I am safe and secure. I am comfortable and peaceful.
I am letting go of any worries. I am ready for sleep. I am drifting off into a restful sleep. I am now falling asleep.”
Practical Applications and Examples: How To Fall Asleep Fast
Turning knowledge into action is key to achieving better sleep. This section dives into practical ways to integrate the discussed techniques into your daily life, creating a personalized sleep routine, and emphasizing the importance of consistency. Understanding these applications will empower you to take control of your sleep and experience the benefits of a well-rested life.
Creating a Personalized Sleep Routine
A personalized sleep routine is crucial for optimizing sleep. It’s a tailored plan that aligns with your individual needs and preferences. This isn’t a one-size-fits-all approach. Instead, it’s about creating a schedule that promotes relaxation and signals to your body that it’s time for sleep. This involves understanding your natural sleep-wake cycle and adjusting your routine accordingly.
For instance, if you naturally wake up early, adjust your bedtime accordingly. Consistency is vital in establishing a personalized sleep routine.
Importance of Consistency in Sleep Routines
Consistency is paramount in establishing a healthy sleep pattern. Your body thrives on routine. A regular sleep schedule, including both bedtime and wake-up time, helps regulate your circadian rhythm. This internal clock governs your sleep-wake cycle, and consistency reinforces its natural patterns. Irregular sleep schedules disrupt the circadian rhythm, leading to difficulty falling asleep and staying asleep.
Maintaining a consistent sleep routine, even on weekends, minimizes these disruptions.
Examples of Personalized Bedtime Routines
Creating a calming bedtime routine signals to your body that it’s time to wind down. This routine can include activities such as taking a warm bath, reading a book, listening to relaxing music, or practicing mindfulness. A consistent bedtime routine can help you relax and prepare your mind and body for sleep. Here are a few examples:
- Relaxing Bath Routine: A warm bath with Epsom salts, followed by gentle stretching, can promote relaxation and muscle recovery, setting the stage for a restful night’s sleep. The warmth helps soothe the muscles and the Epsom salts can aid in relaxation.
- Mindfulness and Meditation: Engaging in a few minutes of mindfulness or meditation can help clear your mind of racing thoughts, reducing anxiety and promoting a sense of calm before sleep. Focusing on your breath and releasing tension can lead to improved sleep quality.
- Quiet Reading Time: Choosing a light, non-stimulating book can help transition your mind from the day’s activities to a state of relaxation. The act of reading, combined with the calming atmosphere, promotes sleep.
Practical Tips for Each Category
| Category | Tip | Explanation |
|---|---|---|
| Relaxation Techniques | Practice deep breathing exercises before bed. | Deep breathing calms the nervous system, reducing stress and promoting relaxation. |
| Creating a Conducive Sleep Environment | Ensure your bedroom is dark, quiet, and cool. | A dark, quiet, and cool environment promotes better sleep by minimizing distractions and maintaining a comfortable temperature. |
| Sleep Hygiene Practices | Establish a consistent sleep schedule, even on weekends. | Consistency in sleep schedule regulates your body’s natural sleep-wake cycle, improving sleep quality. |
| Dietary Influences on Sleep | Avoid large meals and caffeine close to bedtime. | Large meals and caffeine can disrupt sleep patterns by stimulating the body and increasing alertness. |
| Addressing Underlying Sleep Disorders | Consult a healthcare professional if you suspect a sleep disorder. | Professional evaluation can identify and address potential sleep disorders, leading to improved sleep. |
| Cognitive Strategies for Sleep | Challenge negative thoughts about sleep. | Negative thoughts about sleep can exacerbate insomnia. Replacing these thoughts with positive affirmations and realistic expectations can be beneficial. |
Sleep-Promoting Supplements and Considerations

Taking supplements to improve sleep can be tempting, but it’s crucial to approach them with caution and understanding. While some supplements may help, they aren’t a magic bullet for sleep problems. It’s essential to explore the potential benefits and risks, understand how to determine if they’re right for you, and prioritize consulting a healthcare professional before starting any new supplement regimen.Many people turn to supplements hoping for a quick fix for sleep issues.
However, a holistic approach that combines lifestyle changes with professional guidance is often more effective in the long run. Before jumping to supplements, ensure you’ve exhausted other avenues, like establishing a consistent sleep schedule, optimizing your sleep environment, and managing stress.
Potential Sleep-Promoting Supplements
Various supplements claim to promote sleep, but their effectiveness and safety vary. Some common ones include melatonin, valerian root, chamomile, and magnesium. Understanding their potential effects can help you make informed decisions.
- Melatonin: This hormone naturally regulates sleep-wake cycles. Supplementing with melatonin may help regulate circadian rhythms, particularly in individuals with irregular sleep schedules or jet lag. It can also assist in falling asleep faster. However, prolonged use can sometimes disrupt the body’s natural melatonin production.
- Valerian Root: This herb is known for its calming properties. Some studies suggest that it may help reduce anxiety and promote relaxation, potentially improving sleep quality. However, it can sometimes cause mild side effects like headaches or stomach upset.
- Chamomile: This herbal tea is traditionally used for its calming effects. Chamomile’s potential to reduce anxiety and promote relaxation may contribute to better sleep. However, its effectiveness for sleep improvement is less robust compared to other supplements.
- Magnesium: Magnesium plays a role in various bodily functions, including relaxation. Some studies indicate that magnesium supplementation may help improve sleep quality and reduce muscle tension, potentially contributing to a more restful sleep. However, high doses can cause gastrointestinal discomfort.
Potential Risks and Benefits of Sleep Aids
Sleep aids, including supplements, can be helpful, but it’s crucial to weigh the potential risks and benefits. While they can sometimes improve sleep, they can also have unwanted side effects or interact negatively with other medications. It’s important to consult with a healthcare professional to discuss potential risks and to determine if supplements are appropriate for you.
- Potential Benefits: Supplements can be a useful tool for short-term sleep improvement, helping individuals overcome temporary sleep difficulties. Some supplements may enhance relaxation and reduce anxiety, promoting a more restful sleep. For individuals with specific sleep disorders, supplements may offer a targeted approach, but these should be considered part of a larger treatment plan.
- Potential Risks: Using supplements improperly or without professional guidance can lead to side effects. Interacting with other medications is a significant concern, as is the potential for long-term effects on the body’s natural sleep regulation mechanisms. Furthermore, some supplements may not be effective for everyone.
Determining Supplement Appropriateness
Deciding if supplements are suitable for you involves several factors. Consider your current health status, other medications you’re taking, and the severity of your sleep difficulties. It’s essential to carefully weigh the potential benefits against potential risks.
- Individual Needs: Assess your current sleep habits and underlying causes of sleep issues. A comprehensive evaluation can determine whether supplements are necessary and appropriate for your specific needs. It’s crucial to consider the severity and duration of your sleep difficulties before relying on supplements.
- Severity of Sleep Issues: If your sleep problems are mild and temporary, lifestyle changes and other non-pharmacological interventions might be sufficient. For chronic or severe sleep disorders, supplements could be part of a broader treatment plan, but only under the guidance of a healthcare professional.
Importance of Professional Consultation
Before using any sleep-promoting supplement, it’s critical to consult with a healthcare professional. They can assess your specific needs, rule out any underlying medical conditions, and advise you on appropriate dosages and potential interactions with other medications. This crucial step ensures your safety and effectiveness of the supplement regimen.
| Supplement | Potential Effects | Warnings |
|---|---|---|
| Melatonin | May regulate circadian rhythm, help fall asleep faster | May disrupt natural melatonin production with prolonged use, interactions with certain medications possible |
| Valerian Root | May reduce anxiety, promote relaxation | Can cause mild side effects like headaches or stomach upset, interactions with other medications are possible |
| Chamomile | May reduce anxiety, promote relaxation | Effectiveness for sleep improvement is less robust than other supplements |
| Magnesium | May improve sleep quality, reduce muscle tension | High doses can cause gastrointestinal discomfort, interactions with certain medications are possible |
End of Discussion
In conclusion, achieving a fast and restful sleep is a journey that requires a multifaceted approach. By combining relaxation techniques, optimizing your sleep environment, prioritizing sleep hygiene, and understanding dietary influences, you can pave the way for a consistently rejuvenating night’s sleep. Remember that consistency is key, and tailoring these strategies to your individual needs will yield the best results.
Ultimately, a personalized sleep routine will lead to a more fulfilling and productive life.