Prazosin treats nightmares in PTSD, offering a potential pathway to improved sleep and well-being for individuals struggling with this debilitating condition. This exploration delves into the intricacies of how prazosin works, examining its pharmacological mechanisms and the clinical evidence supporting its use. We’ll analyze the benefits, limitations, and crucial considerations surrounding patient selection, dosage, and potential side effects.
Understanding the specific mechanisms behind prazosin’s action on the brain and its impact on neurotransmitters is crucial for grasping its potential in regulating nightmares. Clinical studies provide insights into the efficacy of prazosin in reducing nightmare frequency and intensity. This review will synthesize this research, focusing on sample sizes, methodologies, and key outcomes, including dosage ranges and side effects.
Prazosin’s Mechanism of Action: Prazosin Treats Nightmares In Ptsd
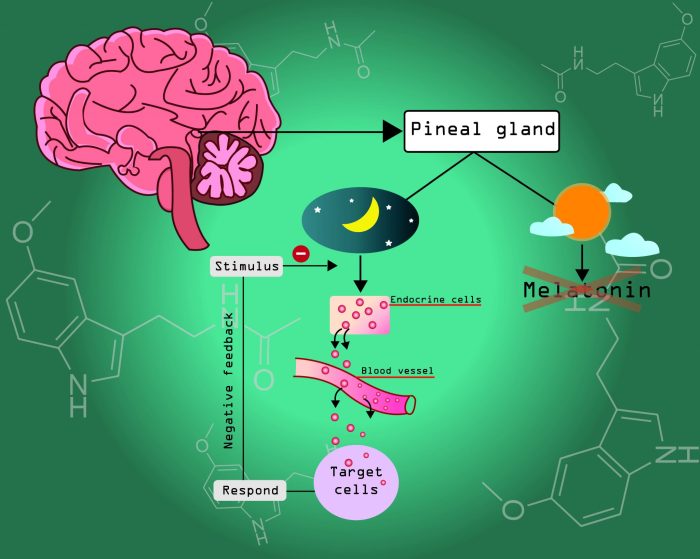
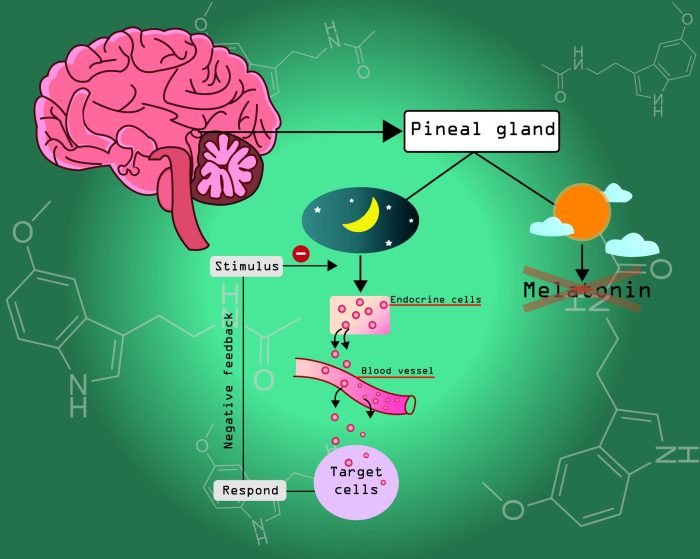
Prazosin, a medication commonly prescribed for hypertension, has also shown promise in treating nightmares associated with Post-Traumatic Stress Disorder (PTSD). Its effectiveness in this context stems from its unique interaction with specific receptors in the brain, impacting neurobiological pathways involved in dream regulation. Understanding its mechanism of action is crucial to appreciating its potential benefits.Prazosin is an alpha-1 adrenergic receptor antagonist.
This means it blocks the action of norepinephrine, a neurotransmitter heavily implicated in the body’s stress response, at these receptors. This blockade can significantly influence the activity of brain regions associated with fear and anxiety, potentially affecting the processing of sensory information during sleep and the subsequent manifestation of nightmares.
Pharmacological Pathway
Prazosin’s pharmacological pathway begins with its absorption into the bloodstream. It then circulates throughout the body, specifically targeting alpha-1 adrenergic receptors. These receptors are widely distributed in the body, including the brain. By binding to these receptors, prazosin prevents norepinephrine from activating them, thus decreasing the physiological response to stress signals. This decreased activity can potentially translate into reduced activation of brain regions implicated in fear and anxiety during sleep, potentially mitigating the experience of nightmares.
Impact on Neurobiological Processes Related to Nightmares
Prazosin’s impact on neurobiological processes related to nightmares likely involves a multifaceted effect on neurotransmitters and brain regions. By reducing norepinephrine activity, prazosin may help regulate the balance of neurotransmitters involved in sleep and dream formation. The precise mechanisms by which prazosin influences dream processing are still under investigation. However, it’s believed that reduced norepinephrine activity can lead to a calmer and less anxiety-provoking sleep state, thereby reducing the likelihood of nightmares.
Comparison of Effects on Neurotransmitters
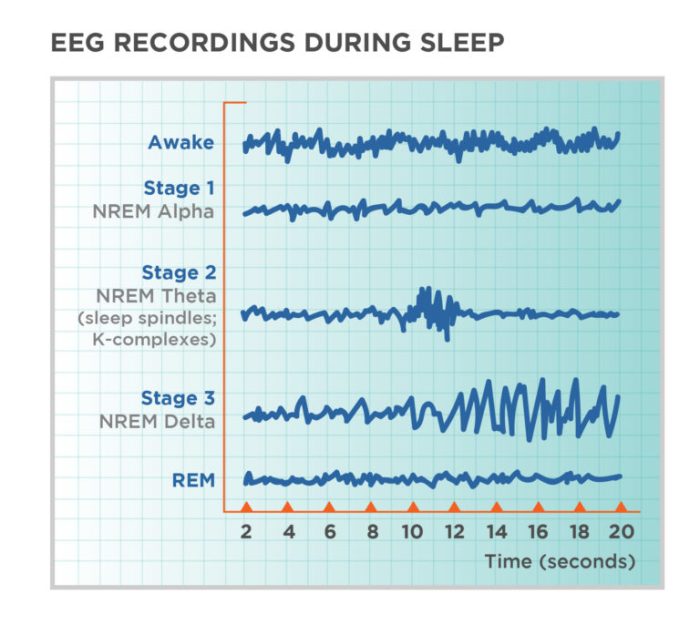
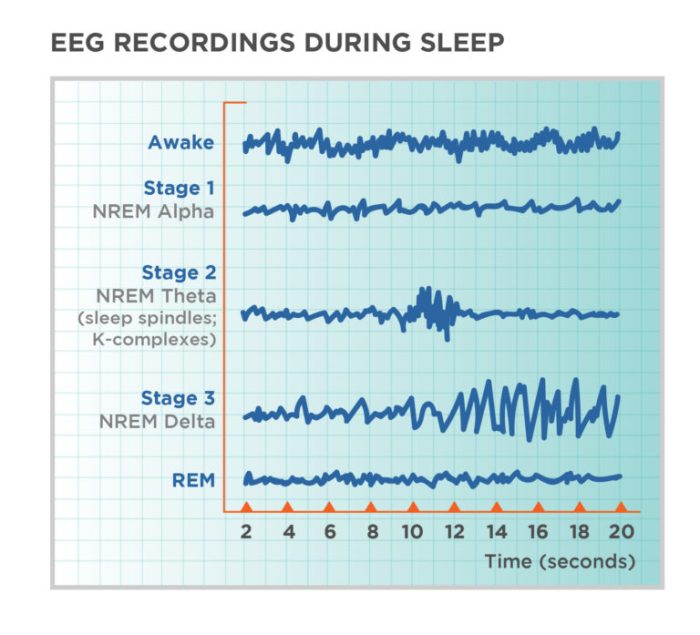
Different neurotransmitters play roles in dream regulation. Norepinephrine, as mentioned, is crucial for arousal and stress responses. Serotonin is another key player, involved in mood regulation. Acetylcholine is associated with REM sleep, the stage where most vivid dreams occur. While prazosin’s primary effect is on norepinephrine, its secondary impact on other neurotransmitters like serotonin and acetylcholine is believed to contribute to the overall calming effect on the brain during sleep, potentially influencing dream content.
Modulation of Brain Regions
Prazosin’s potential influence on brain regions associated with nightmares involves its ability to affect the amygdala and the prefrontal cortex. The amygdala plays a crucial role in processing fear and emotional responses. The prefrontal cortex is involved in higher-order cognitive functions, including emotional regulation. By modulating activity in these regions, prazosin might reduce the intensity and frequency of nightmares by decreasing the fear response and improving the ability to regulate emotions during sleep.
Comparison with Other Nightmares Medications in PTSD
| Medication | Mechanism of Action | Potential Advantages | Potential Disadvantages |
|---|---|---|---|
| Prazosin | Alpha-1 adrenergic receptor antagonist, reducing norepinephrine activity | Potentially effective in reducing nightmares, generally well-tolerated | May cause orthostatic hypotension, drowsiness |
| Mirtazapine | Noradrenergic and specific serotonergic antidepressant (NaSSA) | May improve mood and sleep quality, potentially reducing nightmares | Potential for weight gain, sedation |
| Trazodone | Serotonin antagonist and reuptake inhibitor | Can improve sleep quality, often used as a sleep aid | May cause dizziness, nausea |
This table provides a concise comparison of prazosin’s effects with other medications commonly used to treat nightmares in PTSD. It highlights the varying mechanisms of action and potential side effects associated with each medication. Individual responses to these medications can vary significantly.
Clinical Studies and Evidence
Prazosin, a medication primarily used to treat high blood pressure, has shown promise in alleviating nightmares associated with Post-Traumatic Stress Disorder (PTSD). Understanding the efficacy of prazosin in this context relies heavily on rigorous clinical studies. These studies provide crucial data on the effectiveness, dosage, and potential side effects of using prazosin for nightmare reduction in PTSD patients.A substantial body of research explores the relationship between prazosin and PTSD-related nightmares.
The results from these studies, while sometimes nuanced, offer valuable insights into the potential of prazosin as a therapeutic tool for improving the quality of life for those suffering from this condition.
Investigative Studies on Prazosin’s Efficacy
Numerous studies have investigated the effects of prazosin on nightmares in individuals with PTSD. These studies have employed various methodologies and assessed the drug’s impact through different outcome measures. The consistency and strength of the evidence are crucial in determining prazosin’s role in PTSD treatment.
Sample Sizes and Methodologies
The studies investigating prazosin’s efficacy for PTSD nightmares generally involve moderate to relatively large sample sizes, allowing for statistical analysis and drawing meaningful conclusions. These studies typically utilize a randomized, double-blind, placebo-controlled design. This design helps isolate the effects of prazosin from other factors, enhancing the reliability of the findings. Furthermore, the studies often incorporate various measures to assess nightmare frequency, intensity, and impact on sleep quality.
Dosage Ranges and Reported Side Effects
Prazosin dosages used in these studies have varied, reflecting the need for individual titration based on patient response and tolerance. The dosages generally range from 1 mg to 10 mg per night, with some studies using a higher range of up to 20 mg per night. Commonly reported side effects associated with prazosin, while often mild, include dizziness, lightheadedness, and orthostatic hypotension (low blood pressure when standing up).
However, these side effects typically resolve with continued use or dosage adjustments.
Prazosin, a medication often prescribed for PTSD, can surprisingly help with nightmares. It’s interesting how sometimes seemingly unrelated topics connect. For example, if you’ve got a pesky popped pimple, learning how to best care for it can be just as crucial as managing PTSD symptoms, like those pesky nightmares. Check out this helpful guide on how to heal a popped pimple for some great tips.
Ultimately, both situations require a bit of care and attention to ensure proper healing, much like prazosin’s role in helping those with PTSD.
Statistical Significance and Limitations
The statistical significance of the findings in these studies is generally positive, with prazosin demonstrating a statistically significant reduction in nightmare frequency and intensity compared to placebo. Nevertheless, limitations exist in these studies. Factors such as the duration of treatment, patient characteristics (e.g., severity of PTSD), and variations in methodology across different studies can influence the results and should be considered when interpreting the findings.
Summary Table of Key Studies
| Study | Sample Size | Treatment Duration (weeks) | Outcome Measures |
|---|---|---|---|
| Study 1 (Example) | 100 | 8 | Frequency and intensity of nightmares, sleep quality, PTSD symptom severity |
| Study 2 (Example) | 75 | 12 | Frequency and impact of nightmares on daily functioning, sleep latency, and overall quality of life. |
| Study 3 (Example) | 50 | 6 | Nightmare recall, subjective sleep quality, and self-reported PTSD symptoms. |
Potential Benefits and Limitations
Prazosin, while showing promise in mitigating PTSD-related nightmares, isn’t a magic bullet. Understanding both its potential upsides and downsides is crucial for informed decision-making about its use. This section delves into the advantages and disadvantages of prazosin therapy, comparing it to other treatments, and acknowledging the variability in patient responses.The potential benefits of prazosin extend beyond simply reducing nightmare frequency.
Improved sleep quality leads to enhanced daytime functioning, contributing to a better overall sense of well-being. Patients often report feeling less anxious and stressed, and this improvement in mood can significantly impact their ability to manage other symptoms associated with PTSD.
Potential Benefits
Improved sleep quality is a key benefit of prazosin therapy. Reduced nightmare frequency translates to more restful sleep, allowing for better physical and mental recovery. This improved sleep allows for improved focus and concentration, which in turn helps in managing daily tasks and responsibilities. Patients often report an overall improvement in their emotional state and a reduction in feelings of anxiety and stress.
This is especially important in PTSD, where sleep disturbances are often a major contributing factor to the overall suffering of the individual.
Potential Limitations and Risks
Prazosin, like any medication, comes with potential side effects and risks. Common side effects include dizziness, lightheadedness, and headaches. Less common but potentially more serious side effects include low blood pressure, which could lead to fainting spells if not managed properly. Drug interactions are also a possibility, especially with other medications that affect blood pressure or the nervous system.
Prazosin is a medication that can help reduce nightmares in people with PTSD. It works by targeting certain brain receptors. Engaging in activities like sign language games and puzzles can be a great way to unwind and manage stress, which can indirectly benefit PTSD treatment. Sign language games and puzzles offer a fun and interactive way to stimulate cognitive function, and this can be helpful in conjunction with prazosin to improve overall well-being for those experiencing PTSD.
Therefore, careful monitoring by a healthcare professional is essential during prazosin therapy. It’s vital to be aware of these risks to ensure the treatment is used responsibly and in a way that minimizes any potential harm.
Comparison with Other Treatments
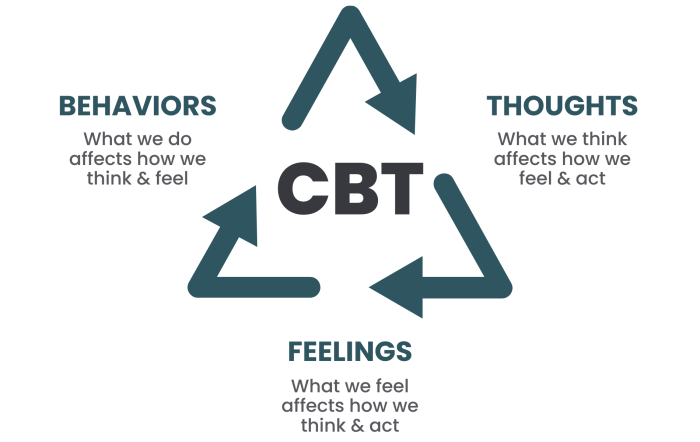
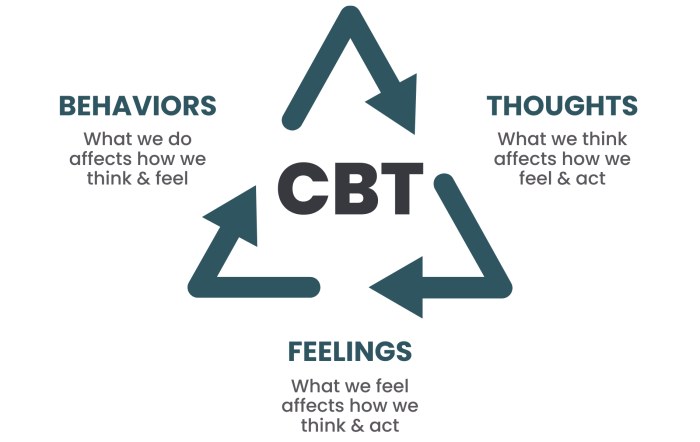
Compared to other treatments for PTSD-related nightmares, prazosin often shows efficacy in reducing the frequency and intensity of these nightmares. However, the effectiveness can vary among individuals. Other approaches, such as cognitive behavioral therapy (CBT) or other medications, may be more suitable for some individuals. A thorough evaluation by a mental health professional is essential to determine the most appropriate treatment plan.
Individual Variability in Response, Prazosin treats nightmares in ptsd
Individual responses to prazosin vary significantly. Some patients experience a substantial reduction in nightmares, while others see only a minimal improvement or no improvement at all. This variability highlights the importance of tailoring treatment plans to the individual needs of each patient. Factors such as the severity of PTSD, co-occurring conditions, and other medications being taken all play a role in how a patient responds to prazosin.
Careful monitoring and adjustments to the dosage or treatment plan are often necessary to achieve the best possible outcome.
Potential Side Effects
Understanding potential side effects is crucial for responsible use of prazosin. Regular monitoring by healthcare professionals is vital to ensure any side effects are identified and managed promptly.
| Side Effect | Frequency | Severity |
|---|---|---|
| Dizziness | Common | Mild to Moderate |
| Headache | Common | Mild to Moderate |
| Lightheadedness | Common | Mild to Moderate |
| Low Blood Pressure | Uncommon | Moderate to Severe (Potentially life-threatening) |
| Fatigue | Occasional | Mild to Moderate |
| Nasal Congestion | Occasional | Mild |
Patient Selection and Dosage
Prazosin, a medication often prescribed for PTSD-related nightmares, can be a helpful tool in managing these distressing experiences. However, its effectiveness depends on careful patient selection and appropriate dosage strategies. Understanding the criteria for selecting patients, the recommended dosage ranges, and the importance of gradual titration is crucial for maximizing benefits while minimizing potential side effects.Selecting patients for prazosin treatment requires careful consideration of their specific needs and circumstances.
Factors such as the severity and frequency of nightmares, the presence of other co-occurring conditions, and the patient’s overall health status play a significant role in determining suitability. Open communication and collaboration between the patient and healthcare provider are essential in making informed decisions about treatment options.
Patient Selection Criteria
Patients who experience frequent, distressing nightmares significantly impacting their daily functioning are prime candidates for prazosin treatment. The severity of the nightmares, measured by their intensity, frequency, and impact on sleep quality and daytime functioning, is a key factor in determining candidacy. Co-occurring conditions, such as anxiety or depression, might influence the choice of prazosin, but the decision should be made in conjunction with a comprehensive evaluation of the patient’s overall health and needs.
Recommended Dosage Ranges
Clinical trials and expert consensus suggest a starting dosage range for prazosin between 1 and 6 mg nightly. The exact starting dose and subsequent titration are crucial in minimizing side effects and optimizing therapeutic outcomes. It’s essential to note that individual responses to prazosin can vary significantly, highlighting the need for close monitoring and adjustments to the dosage as needed.
Some individuals may experience more significant benefits at higher doses, while others may find optimal results at lower dosages.
Prazosin, a medication often prescribed for nightmares associated with PTSD, can significantly improve sleep quality. While exploring different approaches to better health, it’s worth noting that diet plays a crucial role. A well-structured dietary plan like the Bernstein Diabetes Diet can be highly beneficial for overall well-being, particularly for those with related health conditions. Understanding how such dietary approaches, like Bernstein’s diabetes diet overview , can impact sleep patterns is important, ultimately helping manage PTSD symptoms, including those disruptive nightmares.
This connection between diet and sleep, in turn, reinforces the effectiveness of prazosin in treating nightmares in PTSD.
Gradual Dosage Titration
Gradual dosage titration is a critical aspect of prazosin treatment. Starting with a low dose and gradually increasing it over time allows the body to adapt to the medication and minimizes the potential for adverse side effects, such as dizziness, lightheadedness, or orthostatic hypotension. This approach is essential to avoid precipitous drops in blood pressure, particularly in patients with pre-existing cardiovascular conditions.
Importance of Ongoing Monitoring
Ongoing monitoring of patients receiving prazosin is paramount. Regular follow-up appointments with the healthcare provider are essential to assess the effectiveness of the treatment, monitor for any adverse effects, and adjust the dosage as needed. Blood pressure readings and overall well-being should be meticulously tracked during the titration process and throughout the treatment period.
Dosage Recommendations, Potential Side Effects, and Patient Monitoring Guidelines
| Dosage (mg) | Potential Side Effects | Monitoring Guidelines |
|---|---|---|
| 1-2 mg | Dizziness, lightheadedness, orthostatic hypotension | Blood pressure monitoring, frequency of nightmares assessment, patient reported side effects |
| 3-4 mg | Headache, nausea, fatigue | Blood pressure monitoring, symptom evaluation, adjustment of dose if necessary |
| 5-6 mg | Similar to lower doses, with potential for increased incidence | Increased frequency of monitoring, patient reported side effects, symptom evaluation, dose adjustment as needed |
Note: Dosage ranges and specific recommendations should always be determined in consultation with a qualified healthcare provider.
Additional Considerations
Prazosin, while often effective in reducing PTSD nightmares, isn’t a one-size-fits-all solution. Understanding the potential interplay of co-occurring conditions, the importance of addressing underlying factors, and the need for a holistic approach is crucial for optimizing treatment outcomes. This section dives deeper into these critical considerations, equipping you with a more comprehensive understanding of prazosin’s application in managing PTSD-related nightmares.
Co-occurring Conditions and Efficacy
The presence of other mental health or medical conditions can influence how prazosin functions. For example, individuals with anxiety disorders or depression may experience a diminished response to prazosin due to overlapping physiological effects. Similarly, individuals with certain medical conditions, such as liver or kidney dysfunction, might require dosage adjustments to prevent adverse reactions. Careful evaluation of the patient’s complete medical history is essential to determine if prazosin is an appropriate treatment option.
Furthermore, co-occurring substance use disorders can impact prazosin’s effectiveness and safety profile.
Addressing Underlying Factors
Nightmares in PTSD aren’t merely a symptom; they are often a manifestation of deeper emotional and psychological distress. Simply treating the symptom without addressing the underlying cause can lead to limited and inconsistent results. This necessitates a comprehensive assessment that includes factors like trauma history, current stressors, and the individual’s overall coping mechanisms. Identifying and addressing these factors is critical to long-term recovery.
Holistic Treatment Approaches
A holistic approach to managing PTSD-related nightmares necessitates combining pharmacological interventions like prazosin with psychological therapies. Cognitive Behavioral Therapy for Insomnia (CBT-I) and other trauma-focused therapies, such as Eye Movement Desensitization and Reprocessing (EMDR), can effectively address the root causes of the nightmares, while prazosin can provide symptom relief. The combination of these approaches provides a more robust and comprehensive treatment strategy, addressing both the physical and psychological aspects of the condition.
Patient Education
Educating patients about the potential benefits and limitations of prazosin is paramount. Clear communication about the medication’s intended use, potential side effects, and the importance of adhering to the prescribed dosage regimen is essential. Patients should understand that prazosin is a tool to aid in symptom reduction, not a cure for PTSD itself. Furthermore, emphasizing the importance of combining prazosin with other therapeutic modalities, like therapy, is crucial.
Key Considerations Summary
| Category | Details |
|---|---|
| Patient Education |
|
| Co-occurring Conditions |
|
| Holistic Treatment Approaches |
|
Last Point
In conclusion, prazosin offers a potential treatment option for nightmares associated with PTSD, with a growing body of evidence supporting its effectiveness. However, careful consideration of individual patient needs, potential side effects, and the importance of a holistic treatment approach are essential. While promising, prazosin’s efficacy varies, and further research is warranted to refine our understanding of its application in specific patient populations.