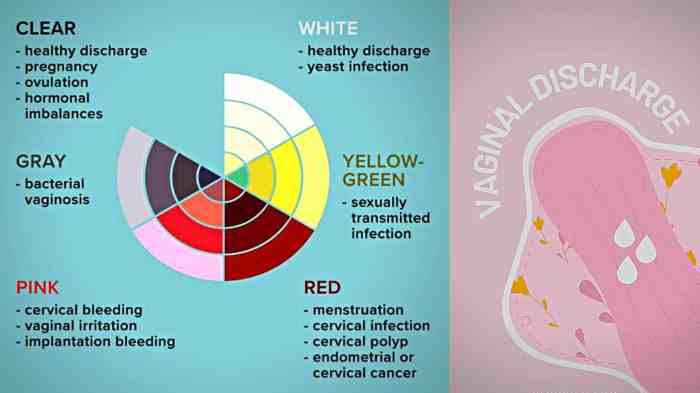
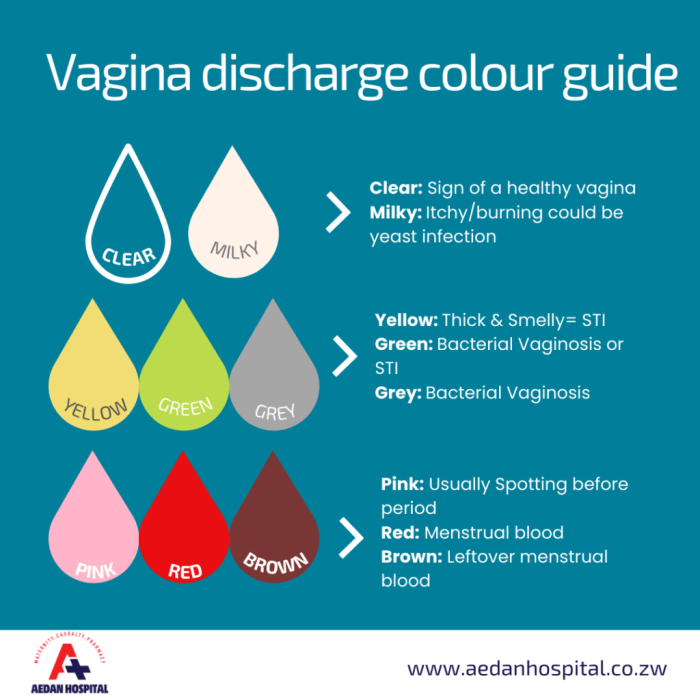
Vaginal discharge color guide sets the stage for understanding your body’s natural functions. This guide delves into the spectrum of normal and abnormal vaginal discharge, exploring the various colors, consistencies, and potential causes. From clear to white, yellow, and even brown or red, we’ll unravel the mysteries behind these variations, helping you distinguish between healthy and concerning discharge.
We’ll examine the factors that influence vaginal discharge, such as your menstrual cycle and hygiene practices. Understanding the potential causes associated with each color variation, alongside other symptoms like itching or pain, is crucial for recognizing potential issues. The guide also emphasizes the importance of seeking professional medical advice for any concerns about your discharge.
Introduction to Vaginal Discharge
Vaginal discharge is a natural bodily fluid produced by the vagina. It plays a crucial role in maintaining vaginal health by cleansing and lubricating the area. While often invisible, it’s a normal and healthy part of a woman’s reproductive system. The amount, consistency, and color of discharge can vary depending on several factors, including the menstrual cycle, hormonal changes, and hygiene practices.
Understanding these variations is important for recognizing when something might be amiss.The purpose of vaginal discharge is multifaceted. It helps to remove dead cells and bacteria from the vagina, keeping the area clean and preventing infection. The lubrication provided by the discharge also facilitates sexual intercourse. Healthy vaginal discharge is typically clear or milky white, and can vary in consistency from watery to slightly sticky.
Normal Variations in Vaginal Discharge
The characteristics of vaginal discharge can fluctuate throughout a woman’s cycle. Before ovulation, discharge is often more watery and stretchy, acting as a lubricant. Around ovulation, the discharge becomes even more abundant, clear, and slippery, which is often associated with heightened fertility. After ovulation, the discharge tends to become thicker and less abundant. These changes are all part of the normal hormonal fluctuations throughout the menstrual cycle.
Factors Influencing Vaginal Discharge
Several factors can impact the appearance and consistency of vaginal discharge. Menstrual cycle phases, as mentioned earlier, play a significant role. Hormonal changes, including those associated with pregnancy, birth control pills, or menopause, can also influence the discharge. Furthermore, hygiene practices can affect the environment of the vagina, potentially leading to changes in the discharge. Proper hygiene, including regular cleansing, is crucial for maintaining vaginal health.
Categorizing Discharge Types
Understanding the different types of vaginal discharge can be helpful in recognizing potential issues. Here’s a breakdown of common discharge types:
| Discharge Type | Appearance | Consistency | Possible Causes |
|---|---|---|---|
| Watery | Clear or slightly cloudy | Thin and watery | Normal during ovulation, after exercise, or stress. |
| Thick | White or off-white | Creamy or sticky | Normal during the luteal phase of the menstrual cycle, pregnancy, or certain medications. |
| White | Thick and white or opaque | Often thick, sometimes clumpy | Yeast infection (candidiasis) is a common cause, but other infections and conditions may also present with white discharge. Hormonal fluctuations can also be a factor. |
| Yellow | Yellow or greenish | May be thick or thin | Possible signs of bacterial vaginosis (BV) or other infections. Important to consult a healthcare professional if this is accompanied by other symptoms like itching, burning, or odor. |
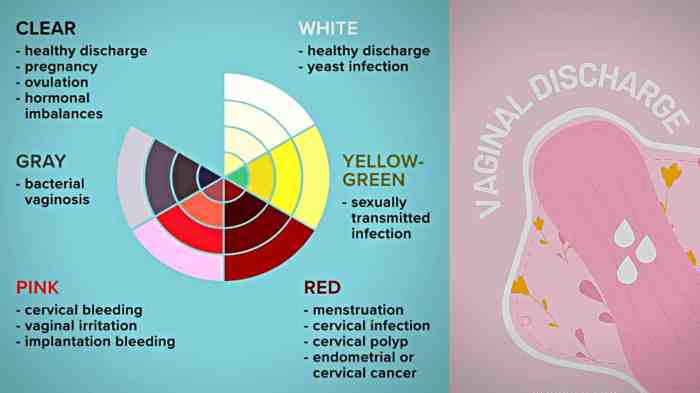
Understanding Discharge Color Variations
Knowing the color of your vaginal discharge can be a helpful clue to potential health issues. Changes in color, texture, or consistency, along with other symptoms, can indicate various conditions, from minor irritation to more serious concerns. Paying attention to these changes is crucial for your overall well-being.Understanding the possible causes behind different discharge colors is important for making informed decisions about your health.
Not all changes are cause for alarm, but consistent or unusual changes warrant attention and consultation with a healthcare provider.
Understanding vaginal discharge colors is key to knowing your body. But sometimes, other symptoms, like a fever, can also signal something’s amiss. Knowing when a fever is concerning is just as important as understanding your vaginal discharge color guide. For instance, if you’re experiencing a fever, checking when is a fever too high can help you determine if it warrants a visit to the doctor.
Ultimately, a clear understanding of both vaginal discharge color and fever levels will give you a better picture of your overall health.
Possible Vaginal Discharge Colors and Potential Causes
Vaginal discharge comes in a variety of colors, each potentially linked to different underlying reasons. The color alone isn’t a definitive diagnosis, but it can be a valuable piece of information for your healthcare provider.
- Clear or Slightly Cloudy Discharge: This is often considered normal, especially if it’s thin and watery. It can be related to the normal hormonal fluctuations throughout the menstrual cycle. However, if the discharge is excessive, thick, or accompanied by other symptoms, it’s important to consult a doctor.
- White or Thick Discharge: This can sometimes be a sign of yeast infections. It often has a thick, clumpy, or cottage cheese-like consistency. Other potential causes include bacterial vaginosis or certain sexually transmitted infections. Accompanying symptoms such as itching, burning, or odor can help determine the cause.
- Yellow or Green Discharge: A yellow or greenish discharge can be a sign of bacterial vaginosis or a sexually transmitted infection (STI). It often has a strong odor. This requires immediate medical attention as these infections can lead to complications if left untreated. Other symptoms like itching, burning, or pain during urination should also be reported.
- Brown Discharge: Brown discharge can be a result of old blood mixed with discharge, often occurring after menstruation or during ovulation. It could also indicate an infection or hormonal imbalance. If the discharge is accompanied by pain, unusual odor, or significant changes in consistency, a healthcare professional should be consulted.
- Red Discharge: Red discharge usually indicates bleeding. This could be due to a variety of factors, including menstruation, trauma, or infections. The presence of significant bleeding, particularly if accompanied by severe pain, requires immediate medical attention to rule out serious conditions.
Importance of Considering Associated Symptoms
Discharge color is just one piece of the puzzle. Other symptoms, such as itching, burning, pain during urination, or unusual odor, can provide valuable context. These additional symptoms can help differentiate between various potential causes and aid in accurate diagnosis.
Discharge Color, Potential Causes, and Associated Symptoms
| Discharge Color | Potential Causes | Associated Symptoms | Additional Notes |
|---|---|---|---|
| Clear/Slightly Cloudy | Normal hormonal fluctuations, vaginal lubrication | None, or mild itching, slight odor | Monitor for changes in consistency or volume. |
| White/Thick | Yeast infections, bacterial vaginosis, STIs | Itching, burning, thick/clumpy discharge, odor | Prompt medical evaluation recommended. |
| Yellow/Green | Bacterial vaginosis, STIs | Strong odor, itching, burning, pain during urination | Urgent medical attention required. |
| Brown | Post-menstrual bleeding, ovulation, infections, hormonal imbalances | Pain, unusual odor, changes in consistency, amount | Consult a healthcare provider for evaluation. |
| Red | Menstruation, trauma, infections, STIs | Severe pain, significant bleeding, unusual odor | Immediate medical attention needed. |
Identifying Potential Medical Concerns
Knowing your body is key to overall well-being, and that includes understanding normal vaginal discharge. While changes in color, consistency, or odor can sometimes be perfectly normal, other times they signal a potential underlying issue. It’s essential to recognize when unusual discharge warrants medical attention. This section will explore various situations where seeking professional advice is crucial.
Situations Requiring Medical Attention
Changes in vaginal discharge can be a sign of an infection or other medical condition. If you experience any of the following, schedule an appointment with your gynecologist or healthcare provider: persistent unusual discharge, especially if accompanied by other symptoms. Prompt evaluation can ensure prompt treatment and prevent potential complications.
So, you’re trying to figure out your vaginal discharge color guide? It can be tricky, right? Sometimes, unusual colors or changes in consistency can be a sign of something more serious, but understanding the normal variations is key. Interestingly, there’s a connection between certain health conditions, like autoimmune diseases, and unexpected bodily changes. For example, some autoimmune conditions might impact various aspects of our health, including vaginal discharge.
If you’re concerned about potential connections between tattoos and autoimmune disease, be sure to check out this informative article on the subject tattoos and autoimmune disease. Ultimately, it’s always best to consult a healthcare professional for accurate information about your vaginal discharge color guide and overall health.
Symptoms Accompanying Abnormal Discharge
Several symptoms often accompany abnormal vaginal discharge, making it easier to identify potential concerns. These include fever, pain in the pelvic area, lower abdominal cramping, burning sensation during urination, and a foul odor. The presence of these symptoms alongside unusual discharge strongly suggests the need for medical evaluation. A healthcare provider can assess the situation and determine the underlying cause.
Conditions Associated with Abnormal Discharge
Several conditions can cause changes in vaginal discharge. Understanding these conditions can help you recognize when medical attention is necessary.
- Bacterial Vaginosis (BV): This is a common bacterial infection. Symptoms include a thin, grayish-white discharge with a fishy odor, especially after intercourse. Itching, burning, or pain during urination can also occur. This is a treatable condition, and early diagnosis is essential.
- Yeast Infections (Candidiasis): These infections are caused by a fungus. Symptoms frequently include a thick, white, clumpy discharge that resembles cottage cheese. Itching, burning, and redness in the vaginal area are also common. Over-the-counter treatments are often effective, but it’s essential to consult a healthcare provider to confirm the diagnosis and ensure appropriate treatment.
- Sexually Transmitted Infections (STIs): Various STIs can cause changes in vaginal discharge, often accompanied by other symptoms. These symptoms can include unusual discharge colors (yellow, green, or brown), strong odor, pain during intercourse, sores, blisters, or itching. The presence of any of these symptoms necessitates immediate medical attention to confirm the diagnosis and initiate appropriate treatment. Early detection and treatment are crucial to prevent potential complications and protect your sexual health.
Table of Medical Conditions and Associated Symptoms, Vaginal discharge color guide
The table below summarizes various medical conditions associated with abnormal vaginal discharge, their common symptoms, and the typical discharge colors. This table is for informational purposes only and should not be used for self-diagnosis. Always consult a healthcare provider for accurate diagnosis and treatment.
| Medical Condition | Symptoms | Discharge Color(s) |
|---|---|---|
| Bacterial Vaginosis | Thin, grayish-white discharge; fishy odor; itching; burning; pain during urination | Grayish-white |
| Yeast Infection | Thick, white, clumpy discharge (cottage cheese-like); itching; burning; redness | Thick, white, clumpy |
| Sexually Transmitted Infections (STIs) | Unusual discharge color (yellow, green, brown); strong odor; pain during intercourse; sores; blisters; itching | Yellow, green, brown, or other unusual colors |
Importance of Seeking Professional Advice
Knowing your body and its normal functions is crucial for overall well-being. However, vaginal discharge, while often a normal bodily process, can sometimes indicate an underlying health concern. This section emphasizes the importance of consulting a healthcare professional if you have any questions or concerns about your vaginal discharge. Seeking timely medical advice ensures prompt diagnosis and treatment, preventing potential complications.
Significance of Professional Consultation
Consulting a healthcare provider is essential for accurate diagnosis and appropriate management of vaginal discharge. A medical professional can differentiate between normal variations and potential medical issues. They possess the expertise to identify the cause of any abnormal discharge, whether it’s due to an infection, hormonal imbalance, or other factors. This professional evaluation ensures that the treatment plan is tailored to the specific cause, preventing unnecessary treatments and potential side effects.
Ignoring or delaying professional help can sometimes lead to the worsening of conditions or the development of more complex issues.
Steps to Take When Seeking Medical Advice
Preparing for your consultation will help ensure a smooth and productive visit. Here are the steps to effectively communicate your concerns to your healthcare provider:
- Gather information about your discharge, including its color, consistency, odor, and any associated symptoms (such as itching, pain, or burning).
- Note any recent changes in your discharge or other relevant factors, like recent sexual activity, use of medications, or stress levels.
- Keep a record of any relevant information that might be useful to your healthcare provider, including the date of onset, frequency, and any other symptoms.
- Be prepared to discuss your medical history, including any known allergies, previous infections, or current medications.
Role of a Healthcare Provider in Diagnosis and Management
A healthcare provider plays a vital role in diagnosing and managing vaginal discharge issues. They will conduct a thorough physical examination, which might include a pelvic exam to assess the condition of the vagina and cervix. This examination helps determine if there are any physical abnormalities or signs of infection. The provider will then consider your medical history, symptoms, and the results of any tests performed to develop a diagnosis.
Based on the diagnosis, they will create a personalized treatment plan, which might involve prescribing medication, recommending lifestyle changes, or referring you to a specialist. This personalized approach ensures the best possible outcome for the individual patient.
Steps Involved in Consulting a Healthcare Professional
The following table Artikels the steps involved in consulting a healthcare professional for vaginal discharge concerns.
| Step | Action |
|---|---|
| 1 | Gather relevant information about your discharge (color, consistency, odor, associated symptoms, recent changes). |
| 2 | Document your medical history (previous infections, allergies, current medications). |
| 3 | Schedule an appointment with your healthcare provider. |
| 4 | Thoroughly describe your symptoms and concerns during the appointment. |
| 5 | Follow your healthcare provider’s recommendations and treatment plan. |
Hygiene and Self-Care Practices
Maintaining optimal vaginal health is crucial for overall well-being. Proper hygiene and self-care practices play a vital role in preventing infections and discomfort. Understanding the importance of these practices allows for proactive management of vaginal health and ensures a comfortable experience.
Essential Hygiene Practices
Maintaining a healthy vaginal environment involves several key hygiene practices. A clean and balanced vaginal microbiome is essential for preventing infections and promoting overall well-being. Avoid using harsh soaps, douches, or scented products in the genital area. These products can disrupt the natural pH balance, leading to irritation and potential infections.
- Gentle Cleansing: Use mild, unscented soap or a specifically formulated cleanser for the intimate area. Water alone is often sufficient. Avoid harsh scrubbing, as this can irritate the delicate skin. Wipe front to back after urination or bowel movements to prevent the spread of bacteria from the anal area to the vagina.
- Regular Washing: Wash the external genital area regularly with mild soap and water, focusing on cleanliness and avoiding harsh scrubbing.
- Avoiding Harsh Products: Avoid using scented soaps, douches, or other scented products in the genital area. These can disrupt the natural pH balance and potentially lead to irritation.
- Proper Drying: After washing, pat the area gently dry with a soft towel. Avoid rubbing, which can cause irritation.
Avoiding Vaginal Irritation
Irritation of the vaginal area can stem from various factors. Understanding these factors allows for proactive measures to prevent discomfort and maintain optimal health.
- Tight Clothing: Avoid wearing tight-fitting clothing, especially synthetic materials, as these can trap moisture and heat, potentially leading to irritation.
- Chemical Exposure: Limit exposure to harsh chemicals, such as those found in some laundry detergents or fabric softeners, as they can irritate the delicate vaginal tissues.
- Allergic Reactions: Be mindful of potential allergic reactions to certain materials, such as scented lotions or certain fabrics. If an allergic reaction occurs, discontinue use and consult a healthcare professional.
Recommended Self-Care Practices
Practicing self-care can contribute to a healthy vaginal environment.
- Maintaining a Balanced Diet: A balanced diet rich in fruits, vegetables, and whole grains supports overall health, including vaginal health.
- Staying Hydrated: Drinking plenty of water helps maintain the body’s overall hydration, contributing to healthy vaginal tissue.
- Stress Management: Managing stress effectively can positively influence overall health and potentially impact vaginal health.
- Regular Exercise: Regular physical activity supports overall health, potentially influencing vaginal health.
- Wearing Breathable Underwear: Opt for cotton underwear, as it is a breathable material, to reduce moisture buildup and irritation.
Summary of Hygiene Tips
| Hygiene Tip | Potential Risks of Poor Hygiene | Benefits of Proper Care |
|---|---|---|
| Gentle cleansing with mild soap or water | Disruption of the vaginal pH balance, irritation, potential infections | Maintains a healthy vaginal microbiome, reduces the risk of infections, prevents discomfort |
| Avoiding harsh products | Irritation, disruption of the natural pH balance, allergic reactions | Reduces the risk of irritation and discomfort, maintains a healthy vaginal environment |
| Wearing breathable underwear | Moisture buildup, potential for fungal infections, irritation | Reduces the risk of infections, prevents moisture-related discomfort, promotes a healthy vaginal environment |
| Avoiding tight clothing | Trapped moisture, increased heat, potential for irritation | Reduces friction, promotes air circulation, prevents irritation |
Illustrative Examples of Discharge: Vaginal Discharge Color Guide
Understanding the different types of vaginal discharge is crucial for recognizing potential health concerns. Paying attention to the characteristics like color, consistency, and odor can help you identify patterns and when to seek medical advice. This section provides illustrative examples of various discharge types, highlighting their key features.
Normal Discharge
Normal vaginal discharge is typically clear or white, and has a mild, odorless or subtle, non-offensive smell. Its consistency can vary from thin and watery to slightly thicker, similar to egg whites. The amount can fluctuate throughout the menstrual cycle, often increasing around ovulation.
Thick White Discharge
This discharge often resembles cottage cheese in texture and is typically white or off-white. It may have a slightly yeasty or sour odor. The consistency is often thick and clumpy. This type of discharge is frequently associated with yeast infections, but other factors could also contribute to it.
Watery Discharge
Watery vaginal discharge is often clear or slightly whitish and has a thin, watery consistency. It is usually odorless or has a mild, non-offensive smell. An increase in watery discharge is sometimes a sign of ovulation, but other factors can also influence its presence.
Understanding vaginal discharge color can be a helpful tool for women’s health. Knowing what’s normal is key, and various resources can help you identify potential issues. For instance, considering the pros and cons of different birth control methods like IUDs is also important for overall well-being. A copper IUD, for example, can have a significant impact on discharge, so understanding pros and cons of iud is crucial in combination with monitoring your discharge.
Ultimately, a vaginal discharge color guide is a valuable resource to consult for potential concerns and to stay informed about your body.
Yellow or Green Discharge
Yellow or green discharge can vary in consistency from thin and watery to thick and clumpy. A thick, yellow or green discharge often has a noticeable, unpleasant odor, sometimes described as fishy or foul. This type of discharge can indicate bacterial infections, and prompt medical attention is warranted.
Bloody or Brown Discharge
Bloody or brown discharge can be a sign of various conditions, including hormonal imbalances, infections, or even pregnancy complications. The color and consistency can vary, from light spotting to heavier bleeding. Bloody or brown discharge outside of menstruation or expected changes during pregnancy should be examined by a healthcare provider. Its color can be indicative of different factors.
For example, brown discharge can be an older blood discharge or even a sign of implantation bleeding in pregnancy.
Table of Illustrative Examples
| Type of Discharge | Color | Consistency | Odor | Possible Causes |
|---|---|---|---|---|
| Normal | Clear, white | Thin, watery to slightly thicker | Mild, odorless or subtle | Normal vaginal function |
| Thick White | White, off-white | Thick, clumpy | Slightly yeasty or sour | Yeast infection, other factors |
| Watery | Clear, slightly whitish | Thin, watery | Mild, odorless | Ovulation, other factors |
| Yellow/Green | Yellow, green | Thin to thick, watery to clumpy | Fishy, foul | Bacterial infections |
| Bloody/Brown | Bloody, brown | Variable | Variable | Hormonal imbalances, infections, pregnancy complications |
Normal Discharge vs. Abnormal Discharge
Understanding the difference between normal and abnormal vaginal discharge is crucial for women’s health. While some variation in discharge is perfectly normal, changes in color, consistency, odor, or associated symptoms can signal an underlying issue. This section will detail the key distinctions to help you recognize potential problems and encourage timely medical intervention.
Distinguishing Factors
Normal vaginal discharge is a healthy bodily function. It serves to cleanse and lubricate the vagina, maintaining a balanced environment. Abnormal discharge, on the other hand, often indicates an infection, irritation, or other medical condition. Recognizing the differences is essential for taking appropriate action.
| Characteristic | Normal Discharge | Abnormal Discharge |
|---|---|---|
| Color | Typically clear, milky, or slightly white. May appear white or off-white, but not thick or clumpy. | Yellow, green, gray, brown, or bloody. Significant changes in color from usual discharge. Discharge that is noticeably thick or clumpy. |
| Consistency | Thin, watery, or creamy. May have a slightly sticky or tacky quality, but not thick or clumpy. | Thick, clumpy, frothy, or stringy. May have a cottage cheese-like consistency or resemble mucus. |
| Odor | Mild or odorless. A subtle, natural scent is possible. | Unpleasant, fishy, or foul odor. A strong or unusual odor is a cause for concern. |
| Associated Symptoms | Usually no additional symptoms. May experience mild itching or irritation. | Itching, burning, pain during urination or intercourse, swelling, redness, or fever. Any accompanying pain, discomfort, or fever. |
Importance of Differentiation
Distinguishing between normal and abnormal discharge is vital for prompt diagnosis and treatment. Abnormal discharge can stem from various causes, including infections like bacterial vaginosis, yeast infections, or sexually transmitted infections (STIs). Early detection and treatment are crucial for preventing complications and promoting overall reproductive health. Ignoring changes in discharge could delay necessary medical attention, potentially leading to more serious health concerns.
A timely visit to a healthcare provider can address the underlying issue and prevent further discomfort. For example, a persistent, foul-smelling discharge might indicate an infection needing antibiotic treatment.
Conclusive Thoughts
In conclusion, understanding vaginal discharge is a key part of overall women’s health. This comprehensive guide provides a framework for recognizing normal variations and identifying potential concerns. Remember, while this guide offers valuable insights, it’s essential to consult with a healthcare professional for personalized advice and accurate diagnoses. Don’t hesitate to seek help if you have any questions or concerns about your discharge.