Which providers prescribe glps – Which providers prescribe GLP-1s? This question is crucial for anyone considering these medications. Understanding the different types of healthcare professionals who can prescribe GLP-1s, the geographic variations in prescribing practices, insurance coverage, and methods for finding providers are all vital factors to consider. This exploration delves into the intricacies of GLP-1 prescribing, from identifying the right provider to navigating insurance considerations and patient factors.
The landscape of GLP-1 medication prescribing is complex, encompassing a variety of healthcare providers, each with their own areas of expertise and scope of practice. This article will explore the different provider types, their varying levels of experience, geographic variations in prescribing, and the crucial role of insurance coverage. It also covers the importance of patient research and consultation, as well as relevant prescribing guidelines and protocols.
Identifying Provider Types
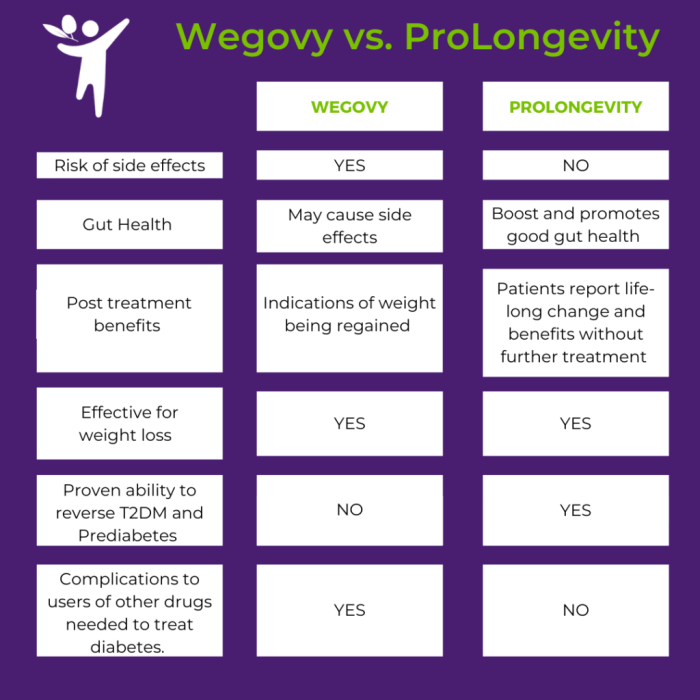
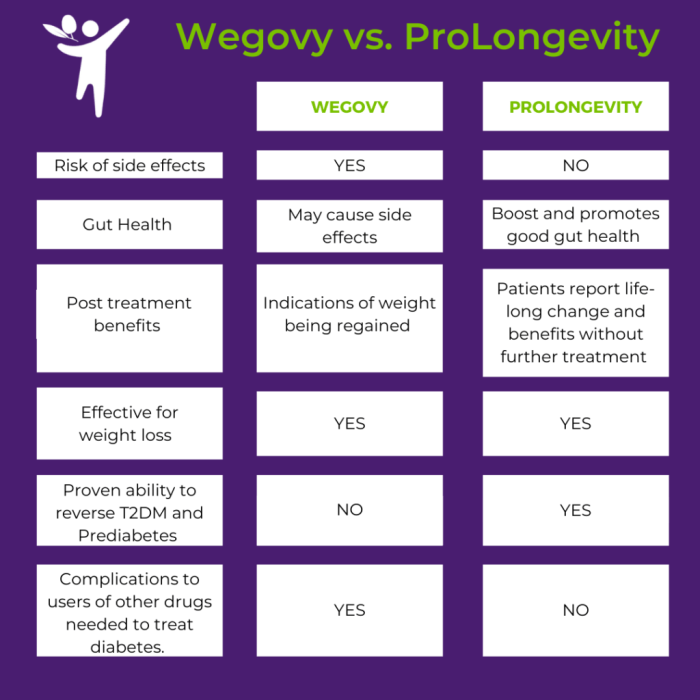
GLP-1 medications, like Ozempic and Trulicity, are increasingly popular for weight management and type 2 diabetes. Understanding who can prescribe these medications and their varying levels of expertise is crucial for patients seeking these treatments.
Healthcare Provider Types Prescribing GLP-1 Medications
Several healthcare professionals can prescribe GLP-1 medications, each with varying levels of experience and expertise. Knowing the differences in training and scope of practice is essential for patients to make informed decisions.
| Provider Type | Description | Typical Patient Population |
|---|---|---|
| Endocrinologist | Specialists in diabetes, thyroid, and hormone disorders. | Patients with type 2 diabetes, prediabetes, or other related conditions. |
| Primary Care Physician (PCP) | General practitioners who provide comprehensive primary care. | Individuals with a range of health concerns, including those with obesity or prediabetes. |
| Diabetologist | Specialists focused solely on diabetes and its related complications. | Patients with complex or severe cases of diabetes. |
| Internal Medicine Physician | Specialists in internal medicine, with a broad understanding of various medical conditions. | Patients with a wide range of chronic health conditions, including obesity or type 2 diabetes. |
| Surgeon (Bariatric) | Specialists in weight loss surgery. | Patients who have obesity and may need combined approaches for weight loss, such as surgery and medication. |
Comparing Provider Expertise and Patient Volume
The level of experience and expertise in prescribing GLP-1 medications varies significantly among different provider types. This difference impacts the complexity of patient care and the potential outcomes.
| Provider Type | Expertise Level | Typical Patient Volume | Common Treatment Approaches |
|---|---|---|---|
| Endocrinologist | High; extensive training in diabetes and metabolic disorders. | Relatively high; may manage complex cases. | Comprehensive management of diabetes, including lifestyle modifications, medication adjustments, and potential use of other medications. |
| Primary Care Physician | Moderate; training in general medicine, may have additional certifications. | High; often sees a large volume of patients. | Focus on lifestyle changes and medication initiation, often referring to specialists for complex cases. |
| Specialist | High; specialized training in a particular area of medicine. | Variable; depends on the specific specialty. | Highly focused approach on the specific condition, often including advanced monitoring and treatment options. |
Differences in Scope of Practice and Authorization Processes, Which providers prescribe glps
Prescribing GLP-1 medications involves specific authorization and regulatory processes, which differ slightly between provider types. This ensures patient safety and appropriate management of the medication.
Endocrinologists, often have the most comprehensive understanding of diabetes management and may have more experience with complex cases, including potential drug interactions and patient monitoring needs. Primary care physicians, on the other hand, may focus on initiating GLP-1 therapy for patients with more straightforward cases, often referring to specialists for those with complications.
Authorization processes for each provider type are regulated by local licensing boards and insurance companies. The specific requirements and procedures can vary significantly depending on the provider’s specialty, the patient’s condition, and the insurance coverage. Patients should consult their provider to understand the specific authorization processes involved.
Geographic Variations in Prescribing Practices
Geographic variations in the prescribing of GLP-1 medications are a complex issue influenced by several interconnected factors. These variations are not simply random; they reflect differences in healthcare access, local guidelines, and even societal norms. Understanding these differences is crucial for tailoring effective public health initiatives and ensuring equitable access to these potentially life-altering treatments.
Potential Differences in Prevalence of GLP-1 Prescribers
Geographic disparities in the prevalence of providers prescribing GLP-1 medications are likely. Different regions may have varying degrees of specialist availability, leading to differences in prescribing patterns. For example, a region with a high concentration of endocrinologists might see a higher rate of GLP-1 prescriptions compared to a region with limited specialist access. These variations could also be related to the availability of education and training opportunities for healthcare professionals within a specific area.
Factors Influencing Prescribing Patterns
Several factors contribute to the variations in prescribing practices across different regions. Insurance coverage policies can significantly influence treatment choices. Regions with more comprehensive coverage for GLP-1 medications might see higher rates of prescription. Conversely, regions with limited or inconsistent coverage might show lower rates. Access to specialists, as previously mentioned, is also a key determinant.
Figuring out which providers prescribe GLP-1 receptor agonists (GLP-1s) can be tricky, but understanding the different types of heart failure medications and their options can help. For example, learning about the various heart failure medications and their availability, like those detailed in this helpful resource on heart failure medications types and available options , can indirectly provide insight into the specialists who are likely to prescribe GLP-1s in this context.
Ultimately, though, checking with your doctor or a cardiologist is the best way to find out which providers can prescribe these medications for your specific needs.
Rural areas often face challenges in accessing endocrinologists or other specialists who are knowledgeable in GLP-1 prescriptions. Furthermore, local guidelines and recommendations issued by medical societies or regulatory bodies can affect the decision-making process of healthcare providers.
Geographic Comparison: Urban vs. Rural Areas
| Region | Provider Density | Reasons for Variation |
|---|---|---|
| Urban | High | Greater concentration of specialists, more accessible healthcare facilities, potentially higher insurance coverage penetration, and better access to advanced diagnostic tools. |
| Rural | Low | Limited access to specialists, fewer healthcare facilities, potentially lower insurance coverage penetration, and challenges in transportation and logistics for patients seeking care. |
Prescribing patterns in urban areas often differ significantly from those in rural areas. Urban centers typically have a higher concentration of specialists, leading to potentially higher rates of GLP-1 prescriptions. Conversely, rural areas often struggle with access to specialists and specialized care, which might lead to lower rates of prescription. The demographics of the patient population also play a role.
Rural areas may have a higher prevalence of certain underlying conditions or health disparities that might impact the decision to prescribe GLP-1 medications. Understanding these factors is vital to developing strategies for improving access and equity in healthcare.
Figuring out which providers prescribe GLP-1 medications can be tricky, but understanding how quickly Wellbutrin works might help. Different doctors have different specialties, and some might be more familiar with these newer medications. A good place to start learning about how your specific situation might affect treatment speed is to check out this resource on how quickly Wellbutrin works.
Ultimately, talking to your primary care doctor or a specialist is the best way to find out which providers are the right fit for you regarding GLP-1 prescriptions.
Insurance Coverage and Reimbursement
Navigating the world of GLP-1 medications often involves a complex interplay of factors, including insurance coverage and reimbursement policies. Understanding these aspects is crucial for patients and healthcare providers alike to ensure access to these potentially life-altering treatments. Insurance companies play a significant role in determining the financial burden associated with these medications, and patients need clear information about their options.Insurance coverage for GLP-1 medications varies considerably, dependent on the specific plan and the individual’s circumstances.
Different insurance companies employ diverse criteria for evaluating and approving these medications, which often includes medical necessity and cost-effectiveness. Patients should always consult with their insurance provider to understand their specific coverage.
Insurance Coverage Policies
Insurance policies vary significantly in their coverage for GLP-1 medications. Factors like the specific type of GLP-1 medication, the patient’s medical condition, and the plan’s formulary all influence coverage decisions. Some plans may cover GLP-1 medications as part of a broader diabetic treatment plan, while others may require pre-authorization or limit coverage to certain situations.
| Insurance Type | Coverage Details | Potential Barriers |
|---|---|---|
| Commercial Health Insurance | Coverage can vary widely, often dependent on the specific plan and formulary. Some plans may cover GLP-1 medications for type 2 diabetes if deemed medically necessary. Pre-authorization or prior approval may be required. Co-pays, co-insurance, and out-of-pocket maximums can significantly impact the financial burden. | Varying levels of coverage, potential for high co-pays or deductibles, pre-authorization delays, and exclusions for specific conditions. |
| Medicare | Medicare Part D prescription drug plans can cover GLP-1 medications. Coverage often depends on the specific plan and the patient’s medical condition. There can be varying co-pays, deductibles, and limitations on coverage. | Variations in coverage levels, potential for high co-pays and deductibles, limited formulary options in some cases. |
| Medicaid | Medicaid coverage for GLP-1 medications can vary significantly by state and individual plans. Coverage criteria often consider medical necessity and may require prior authorization. Co-pays, co-insurance, and out-of-pocket maximums can influence the patient’s financial burden. | State-by-state variations in coverage, potential for high co-pays and deductibles, and restrictions on the types of GLP-1 medications covered. |
Criteria for Determining Coverage
Insurance companies employ specific criteria to determine coverage for GLP-1 medications. These criteria often include demonstrating a clear medical need, such as uncontrolled type 2 diabetes despite other treatments, and the medication’s efficacy in achieving clinically meaningful results. Cost-effectiveness is also a key factor, with companies often prioritizing medications that provide the most value for the cost. Prior authorization is a common requirement, necessitating documentation from a healthcare provider to justify the medication’s necessity.
Financial Barriers
The financial burden of GLP-1 medications can be substantial for some patients. Co-pays, co-insurance, and out-of-pocket maximums can significantly impact the cost, especially for patients with high deductibles. The lack of coverage for certain GLP-1 medications can also create a barrier to access, potentially leading to reduced adherence to prescribed treatments. For example, a patient with a high deductible and a plan with limited coverage for GLP-1 medications might face a significant out-of-pocket expense for each prescription.
This financial strain can affect the patient’s ability to manage their condition effectively.
Methods of Finding Providers
Finding the right healthcare provider for GLP-1 medications is crucial for effective treatment. This involves more than just a simple search; it requires careful consideration of various factors, including the provider’s experience, approach to patient care, and compatibility with your individual needs. Navigating the process can be simplified with a well-informed approach.Understanding the available methods for locating providers who prescribe GLP-1 medications empowers patients to take an active role in their healthcare journey.
This proactive approach allows for a more personalized and effective treatment plan.
Common Methods for Locating GLP-1 Prescribing Providers
Knowing the various methods for locating providers who prescribe GLP-1 medications helps patients make informed decisions. Different approaches may suit different preferences and circumstances.
| Method | Description | Potential Drawbacks |
|---|---|---|
| Physician Directories | Online directories and databases allow searching for physicians by specialty, location, and other criteria. Many directories include provider profiles, credentials, and contact information. | Some directories may not be comprehensive, and the information available might not be up-to-date. Verification of credentials is crucial. |
| Insurance Provider Networks | Insurance companies maintain networks of in-network providers. Patients can use their insurance plan’s website or app to search for providers who prescribe GLP-1 medications and are within their network. | Providers in the network might not be specialists in GLP-1 medications, and insurance coverage varies depending on the specific plan and medication. |
| Online Search Engines | General search engines can be used to find providers, but this method can yield less targeted results. Combining s like “GLP-1,” “diabetes specialist,” and “location” can be helpful. | Results may not always be comprehensive or vetted. The search might yield providers who aren’t specialists in GLP-1 medications, requiring further research. |
| Patient Reviews and Recommendations | Patient reviews and recommendations from friends, family, or online communities can provide valuable insights into a provider’s experience and approach to care. | Reviews may not be entirely objective and can be influenced by individual experiences. Direct interaction with a provider is crucial for assessing compatibility. |
Online Tools and Resources
Various online tools and resources can streamline the search for GLP-1 prescribing providers. Utilizing these resources allows for a more targeted approach.
- Specialized Provider Directories: Specific directories focused on endocrinology or diabetes care often have detailed profiles of providers with experience in GLP-1 prescribing. These resources offer a more focused approach than general physician search engines.
- Health Insurance Websites: Many insurance providers offer online tools to search for in-network providers, facilitating a search by location and specialty.
- Online Review Platforms: Sites dedicated to healthcare provider reviews can provide valuable insights into providers’ reputations and patient experiences. However, it’s essential to consider reviews in the context of diverse experiences and individual preferences.
Importance of Patient Research and Consultation
Thorough research and consultation are crucial when choosing a GLP-1 prescribing provider. Understanding the provider’s experience, approach, and compatibility with individual needs is vital for effective treatment.
Figuring out which providers prescribe GLP-1 medications can be tricky, but thankfully, many endocrinologists and primary care physicians are well-versed in these treatments. If you’re dealing with an itchy skin rash, a good first step might be trying a hydrocortisone cream for relief. For example, hydrocortisone cream for itchy skin rash can often soothe the discomfort, but if the issue persists or you suspect a more serious condition, consulting a dermatologist or another qualified healthcare professional is essential.
Ultimately, finding the right provider for GLP-1 prescriptions often involves research and recommendations from trusted sources.
- Checking Credentials and Experience: Verify the provider’s medical qualifications, board certifications, and experience with GLP-1 medications. This ensures the provider is adequately trained and knowledgeable about the specific medication.
- Understanding Provider’s Approach: Inquire about the provider’s approach to patient care, their treatment philosophy, and their communication style. This helps determine if the provider’s approach aligns with individual needs and preferences.
- Discussing Treatment Options: Schedule a consultation to discuss individual health history, medical conditions, and treatment options. This allows for a personalized discussion of potential risks and benefits associated with GLP-1 medications.
Prescribing Guidelines and Protocols
Navigating the world of GLP-1 medications requires a deep understanding of the guidelines and protocols that govern their use. These guidelines, developed by various organizations, aim to ensure safe and effective treatment while promoting optimal patient outcomes. Compliance with these protocols is crucial for healthcare professionals to provide the best possible care.
Relevant Prescribing Guidelines and Protocols
Numerous organizations publish guidelines for the use of GLP-1 medications. These guidelines provide valuable recommendations for safe and effective treatment. Understanding these recommendations is essential for healthcare providers to make informed decisions about patient care.
| Guideline Source | Key Recommendations | Implications for Patient Care |
|---|---|---|
| American Diabetes Association (ADA) | Emphasizes individualized treatment plans based on patient-specific factors, including A1c levels, cardiovascular risk, and weight goals. Often recommends GLP-1 agonists as a potential second-line therapy for type 2 diabetes after lifestyle modifications and metformin. | Patients benefit from tailored treatment plans, reflecting their unique needs. Early interventions with lifestyle changes and metformin are prioritized. |
| American Association of Clinical Endocrinologists (AACE) | Provides detailed recommendations for the use of GLP-1 medications in various clinical settings, including patients with obesity, cardiovascular disease, and renal impairment. Offers guidance on specific patient populations and medication selection. | Healthcare professionals can utilize detailed guidelines for diverse patient populations. The AACE guidelines assist in selecting the appropriate medication for specific patient conditions. |
| National Institute for Health and Care Excellence (NICE) | Provides recommendations for the use of GLP-1 medications in the United Kingdom. Specific criteria for patient selection, including HbA1c targets and weight loss goals, are emphasized. | Patients in the UK have access to NICE-guided care, leading to standardized treatment protocols. |
Factors Determining Appropriate GLP-1 Medication
Several factors influence the choice of a specific GLP-1 medication for a patient. These factors are often considered in conjunction with the patient’s individual health profile and goals.
- Patient’s comorbidities:
- Patient’s weight goals:
- Patient’s response to previous treatments:
- Potential side effects:
Conditions like heart failure, kidney disease, or pancreatitis may influence the selection of a GLP-1 medication. Careful consideration of these factors is crucial to ensure patient safety.
Some GLP-1 medications are associated with greater weight loss than others. This can be a significant factor in choosing a medication that aligns with the patient’s weight management objectives.
Past responses to different medications, including other diabetes medications, are considered. This historical data helps predict potential responses to GLP-1 medications and personalize the treatment approach.
Individual patient tolerance to potential side effects, such as nausea or gastrointestinal issues, is assessed. Medication selection aims to minimize these adverse effects while maximizing treatment efficacy.
Evolving Guidelines and Patient Access
As research progresses and new data emerges, prescribing guidelines for GLP-1 medications are constantly evolving. This dynamic nature can sometimes affect patient access to these medications.
For example, if new guidelines mandate specific eligibility criteria, certain patients might initially face challenges in obtaining the medication. However, the ultimate goal is to ensure patients receive the best possible care. Efforts are ongoing to facilitate access and ensure that the evolving guidelines do not unduly limit access to these beneficial treatments.
Patient Factors Affecting Prescribing
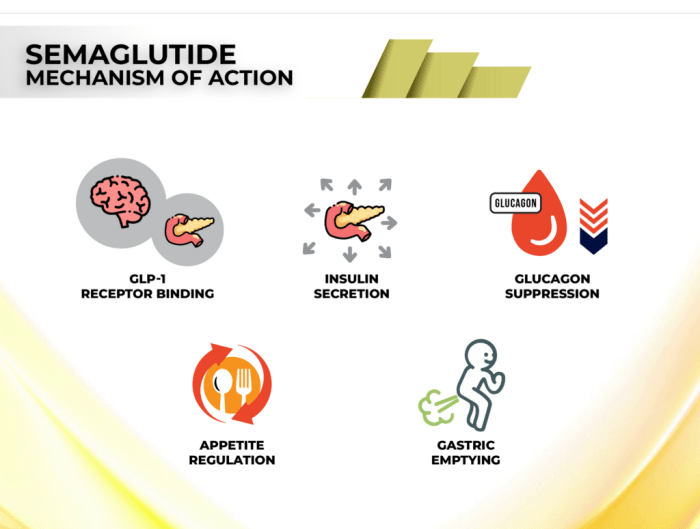
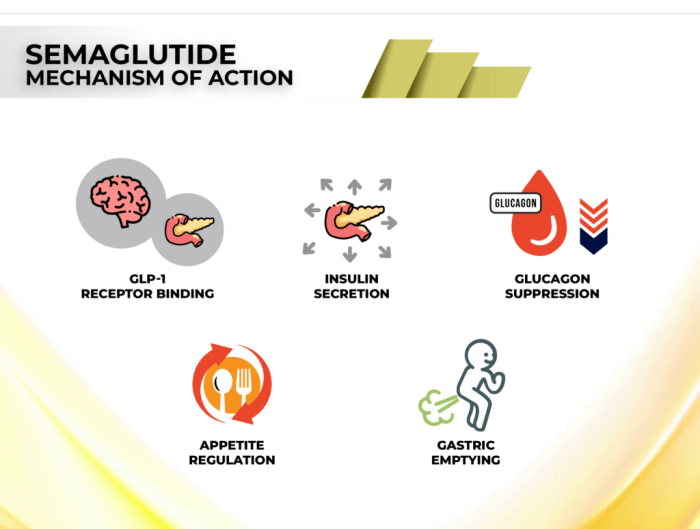
GLP-1 receptor agonists, like semaglutide and dulaglutide, offer promising benefits for weight management and glycemic control. However, their prescription isn’t a one-size-fits-all approach. Understanding the patient’s individual characteristics plays a crucial role in determining the suitability and effectiveness of these medications. This section delves into the key patient factors that influence the prescribing decision.Patient characteristics significantly impact how a patient responds to GLP-1 medications.
These factors, combined with the patient’s medical history and overall health, help physicians tailor treatment plans to maximize efficacy and minimize potential risks. Factors like comorbidities, concurrent medications, and patient adherence all contribute to the overall success of GLP-1 therapy.
Patient Factors Influencing GLP-1 Medication Prescriptions
Patient factors that influence the prescribing decision for GLP-1 medications include a wide range of elements, from their current health status to their willingness to adhere to the treatment plan. A comprehensive evaluation of these factors is critical for achieving positive outcomes.
| Patient Factor | Description | Potential Considerations |
|---|---|---|
| Medical History | Past illnesses, surgeries, and diagnoses. | Existing conditions like heart disease, kidney problems, or pancreatitis can influence the safety and efficacy of GLP-1 medications. A thorough review of the patient’s medical history is essential to identify potential contraindications or precautions. |
| Comorbidities | Simultaneous presence of other medical conditions. | Patients with conditions like hypertension, dyslipidemia, or depression may benefit from GLP-1 therapy but might require careful monitoring or adjustment of other medications. |
| Renal Function | The ability of the kidneys to filter waste products. | Patients with impaired kidney function may require dose adjustments or alternative medications due to potential risks of accumulation and adverse effects. |
| Gastrointestinal Conditions | Issues related to the digestive system. | Patients with conditions like gastroparesis or inflammatory bowel disease might experience increased side effects, necessitating careful monitoring and potential modifications to the treatment plan. |
| Other Medications | Concurrent use of other drugs. | Interactions between GLP-1 medications and other medications can influence their effectiveness or safety. Careful medication reconciliation is crucial. |
| Patient Motivation and Adherence | The patient’s willingness to follow the prescribed treatment plan. | A patient’s commitment to lifestyle changes and adherence to medication schedules significantly impacts the success of GLP-1 therapy. Patient education and support are crucial. |
| Patient Preferences and Lifestyle | Individual preferences and daily routine. | Factors like dietary habits, exercise routines, and personal preferences for injection schedules can impact patient adherence and treatment outcomes. |
Importance of Patient History and Medical Conditions
A thorough patient history is critical in assessing suitability for GLP-1 medications. This involves not only a detailed medical history but also a comprehensive understanding of the patient’s lifestyle and preferences. Identifying potential contraindications and comorbidities is essential to minimize risks and maximize benefits. For example, a patient with a history of pancreatitis might require careful monitoring or an alternative treatment strategy.
Factors Influencing Patient Tolerance
Patient tolerance to GLP-1 medications varies. Factors influencing this tolerance include pre-existing medical conditions, concurrent medications, and the individual patient’s response to the medication. For instance, some patients experience gastrointestinal side effects like nausea or diarrhea, while others may have no issues. Recognizing these variations and providing appropriate support and adjustments is key to ensuring successful treatment.
Closing Notes: Which Providers Prescribe Glps
In conclusion, navigating the process of finding a provider who can prescribe GLP-1s requires careful consideration of several factors. From the expertise of the provider to geographic variations and insurance coverage, patients should be well-informed. This comprehensive overview has provided a roadmap to understand the landscape of GLP-1 prescribing, enabling patients to make informed decisions. Ultimately, the choice of provider should be a collaborative one, based on individual needs and preferences.