Pelvic floor physical therapy offers a specialized approach to addressing various pelvic floor issues. It focuses on restoring the function and strength of the muscles supporting the pelvic organs, which play crucial roles in bladder and bowel control, sexual function, and overall pelvic health. This guide delves into the intricacies of pelvic floor physical therapy, exploring its assessment methods, treatment approaches, and the conditions it effectively manages.
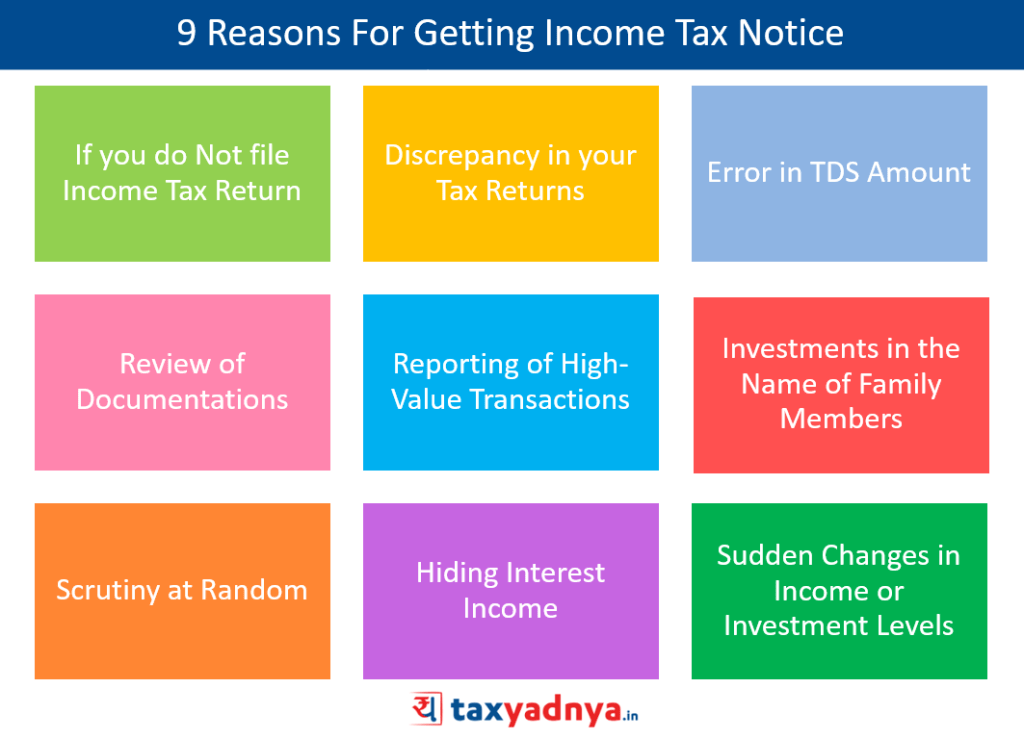
Understanding the key functions of the pelvic floor muscles, the different types of conditions they can address, and the common symptoms associated with pelvic floor dysfunction is paramount. The guide also includes a table comparing common conditions like urinary incontinence, fecal incontinence, and pelvic organ prolapse, detailing their symptoms, possible causes, and treatment options.
Introduction to Pelvic Floor Physical Therapy
Pelvic floor physical therapy is a specialized field of physical therapy focused on the muscles and tissues of the pelvic floor. It’s a non-invasive approach to addressing a wide range of conditions affecting this intricate area of the body. This therapy uses hands-on techniques, exercises, and education to restore function and alleviate discomfort.Pelvic floor muscles play a crucial role in supporting the pelvic organs (bladder, uterus, rectum) and maintaining continence.
These muscles also contribute to sexual function and overall pelvic health. Dysfunction in these muscles can lead to a variety of problems, and pelvic floor physical therapy offers a valuable path towards recovery and improved quality of life.
Key Functions of the Pelvic Floor Muscles
The pelvic floor muscles are responsible for supporting the pelvic organs, maintaining continence, and facilitating sexual function. They act like a hammock, holding the organs in place and preventing leakage. They also play a significant role in the coordination of urination, bowel movements, and sexual response.
Conditions Addressed by Pelvic Floor Physical Therapy
Pelvic floor physical therapy can effectively address a wide range of conditions, including urinary and fecal incontinence, pelvic organ prolapse, and chronic pelvic pain. This therapy provides a tailored approach to restore the proper function and strength of the pelvic floor muscles, leading to symptom relief and improved overall well-being.
Common Symptoms of Pelvic Floor Dysfunction
Common symptoms associated with pelvic floor dysfunction include urinary incontinence (leaking urine), fecal incontinence (leaking stool), pelvic pain, painful intercourse, and difficulty with bowel or bladder control. These symptoms can vary significantly in severity and impact daily life, making specialized therapy crucial for effective management.
Comparison of Pelvic Floor Dysfunction Conditions
| Condition | Symptoms | Possible Causes | Treatment Options |
|---|---|---|---|
| Urinary Incontinence | Frequent urination, urgency, leaking urine with coughing, sneezing, or physical exertion. Some experience leakage even when not actively trying to urinate. | Pregnancy and childbirth, aging, neurological conditions, weakened pelvic floor muscles, certain medications, obesity, chronic cough, and stress. | Pelvic floor muscle exercises (Kegels), biofeedback, electrical stimulation, lifestyle modifications (bladder training), and in some cases, surgical intervention. |
| Fecal Incontinence | Inability to control bowel movements, leakage of stool, straining during bowel movements, and frequent bowel movements. | Weakened pelvic floor muscles, neurological conditions, constipation, irritable bowel syndrome (IBS), injury to the pelvic area, and certain medications. | Pelvic floor muscle exercises, biofeedback, bowel retraining, dietary modifications, and in some cases, surgical intervention. |
| Pelvic Organ Prolapse | Feeling of heaviness, pressure, or bulging in the pelvic area, especially during physical activity or standing for extended periods. Prolapse can involve the bladder, uterus, rectum, or small bowel. | Pregnancy and childbirth, weakened pelvic floor muscles, chronic straining during bowel movements, obesity, and genetic predisposition. | Pelvic floor muscle exercises, supportive devices (pessaries), and in some cases, surgical intervention. |
Assessment and Evaluation Methods
Understanding the intricacies of a patient’s pelvic floor dysfunction requires a thorough assessment process. This process isn’t just about identifying symptoms; it’s about uncovering the underlying causes and contributing factors. A skilled pelvic floor physical therapist uses a combination of subjective and objective methods to gain a comprehensive picture of the patient’s condition. This allows for the development of a personalized treatment plan tailored to their specific needs.
Typical Assessment Process
A typical pelvic floor physical therapy assessment involves a detailed discussion of the patient’s medical history, symptoms, and lifestyle. This initial consultation lays the groundwork for understanding the patient’s concerns and identifying potential contributing factors. The physical examination then moves beyond the surface, employing various techniques to assess pelvic floor muscle function and surrounding structures. This evaluation is crucial in determining the most effective treatment approach.
Methods for Evaluating Pelvic Floor Muscle Function
Pelvic floor muscle function is evaluated using a variety of methods, each offering unique insights. These methods include palpation, which allows the therapist to assess the tone, strength, and mobility of the muscles. Other techniques include internal and external assessments, which help identify potential restrictions or dysfunctions within the pelvic floor. Further, tests of muscle endurance and response to various stimuli are crucial in determining the patient’s individual limitations and capacities.
Diagnostic Tools and Techniques
A range of diagnostic tools and techniques are used in assessing pelvic floor function. These tools include internal and external examinations, allowing the therapist to evaluate the muscles and surrounding tissues. Digital palpation is used to assess muscle tone, strength, and mobility. Other techniques like vaginal or rectal examinations allow for a more comprehensive assessment of the pelvic floor and surrounding tissues.
Pelvic floor physical therapy is amazing for so many things, and it often addresses surprising issues! Have you ever experienced a sore throat, particularly when yawning? It might seem unrelated to your pelvic floor, but sometimes issues in that area can affect other parts of the body, like the muscles supporting your throat. If you’re experiencing a throat hurts when i yawn, check out this article on the topic here.
Ultimately, pelvic floor physical therapy can help improve overall body function, even impacting things like throat discomfort.
Further, electromyography (EMG) can be used to measure the electrical activity of the pelvic floor muscles, providing further insight into muscle function and response.
Assessment Tools and Their Applications
| Assessment Tool | Description | Application | Limitations |
|---|---|---|---|
| Patient History and Symptom Questionnaire | Detailed discussion of medical history, symptoms, and lifestyle factors. | Identifying potential contributing factors, understanding patient’s concerns, and guiding the assessment. | Reliance on patient accuracy and recall; potential for bias. |
| External Inspection | Visual examination of the perineal area and surrounding tissues. | Identifying external abnormalities or indicators of potential pelvic floor dysfunction. | Limited insight into internal structures; requires additional assessments. |
| Internal Pelvic Floor Examination | Palpation of the pelvic floor muscles through the vagina or rectum. | Assessing muscle tone, strength, and mobility, identifying trigger points or restrictions. | Requires patient comfort and cooperation; potential for discomfort. |
| Pelvic Floor Muscle Testing | Assessment of muscle strength, endurance, and coordination through various maneuvers. | Evaluating muscle function, identifying weaknesses or imbalances, and determining the severity of dysfunction. | Requires active patient participation; results may be influenced by patient’s understanding and effort. |
| Electromyography (EMG) | Measuring electrical activity of the pelvic floor muscles. | Providing detailed information about muscle activation patterns, identifying potential neuromuscular issues. | Expensive; requires specialized equipment; potential for discomfort during the procedure. |
Common Patient Questions Regarding the Assessment Process
- What will the physical examination involve? The physical examination involves a range of techniques, including external inspection, internal pelvic floor examinations, and muscle testing. These evaluations help the therapist understand the condition of the pelvic floor muscles and surrounding tissues.
- How long will the assessment take? The assessment process can vary depending on the complexity of the patient’s condition and the specific techniques used. A thorough assessment can take from 45 minutes to an hour or more.
- Will it be painful? While some patients may experience some discomfort during the assessment, particularly during internal examinations, the therapist will work to ensure the patient’s comfort throughout the process. The therapist will adjust the examination techniques as needed to minimize discomfort.
- What happens after the assessment? Following the assessment, the therapist will discuss the findings with the patient and develop a personalized treatment plan. This plan will address the identified issues and work towards improving pelvic floor function.
Treatment Approaches and Techniques
Pelvic floor physical therapy employs a multifaceted approach to address pelvic floor dysfunction, tailoring interventions to the specific needs and goals of each patient. This often involves a combination of manual therapy, targeted exercises, and biofeedback to restore proper function and alleviate symptoms. Effective treatment plans frequently incorporate patient education, emphasizing self-management strategies for long-term well-being.Treatment strategies aim to restore normal pelvic floor muscle tone, coordination, and sensation.
This is achieved through a comprehensive approach that combines various techniques, with the goal of reducing pain, improving bladder and bowel control, and enhancing overall pelvic floor health. Careful consideration is given to the underlying causes of dysfunction and the patient’s individual response to treatment.
Common Treatment Approaches
Treatment approaches for pelvic floor dysfunction are diverse and often integrated. A tailored plan considers factors such as the patient’s medical history, symptoms, and lifestyle. These plans typically involve manual therapy, exercise programs, and biofeedback techniques. Each approach plays a crucial role in restoring pelvic floor function and alleviating symptoms.
Manual Therapy Techniques
Manual therapy techniques are frequently incorporated into pelvic floor physical therapy. These techniques aim to address restrictions in the surrounding tissues and structures that may contribute to pelvic floor dysfunction. Techniques such as myofascial release, trigger point therapy, and mobilization of the sacrum and hips may be employed. These hands-on approaches can help to reduce pain, improve mobility, and promote relaxation of the pelvic floor muscles.
Exercise Programs
Exercise programs are fundamental in pelvic floor physical therapy, targeting specific muscles and improving coordination. These programs typically involve a combination of strengthening, relaxation, and coordination exercises. The exercises aim to restore normal muscle tone and function. Correctly executed exercises are crucial for positive outcomes.
Types of Pelvic Floor Exercises and Their Effectiveness
Pelvic floor exercises encompass various types, each targeting specific muscle groups and offering unique benefits. The effectiveness of each type depends on factors such as patient compliance, technique, and consistency. Different exercises address various aspects of pelvic floor function, promoting strength, flexibility, and coordination.
Comparison of Pelvic Floor Exercises
| Exercise | Target Muscles | Description | Benefits |
|---|---|---|---|
| Kegels | Pubococcygeus (PC) muscle, levator ani muscle, and other pelvic floor muscles | Contracting and releasing the pelvic floor muscles as if stopping the flow of urine. Different variations can target different aspects of the pelvic floor. | Strengthens pelvic floor muscles, improves bladder control, and can help with sexual function. |
| Pelvic Tilt | Abdominal muscles, pelvic floor muscles, and hip flexors | Involves tilting the pelvis upward by engaging core muscles, while maintaining proper posture. | Improves core strength, reduces back pain, and enhances pelvic floor stability. |
| Bird Dog | Core muscles, including pelvic floor muscles, back extensors, and hip muscles. | Involves extending one arm and opposite leg simultaneously while maintaining a straight back. | Improves core stability, strengthens back muscles, and enhances pelvic floor engagement. |
| Bridge | Gluteal muscles, hamstrings, and pelvic floor muscles | Involves lying on the back and lifting the hips off the ground, engaging the glutes and core. | Strengthens glutes, improves hip mobility, and activates pelvic floor muscles. |
Biofeedback Techniques
Biofeedback techniques are used to help patients become more aware of their pelvic floor muscles. These techniques involve providing real-time feedback on muscle activity through visual or auditory signals. This allows patients to learn to control their pelvic floor muscles more effectively. Biofeedback can help individuals identify and correct any muscle imbalances or inefficient activation patterns. This can improve symptoms of pelvic floor dysfunction and enhance self-management strategies.
Pelvic floor physical therapy can be incredibly helpful for various issues, from pain to incontinence. Sometimes, skin conditions like rosacea, psoriasis, or eczema can also impact overall well-being and potentially be connected to underlying health concerns, such as those addressed by pelvic floor therapy. If you’re curious to learn more about identifying these skin conditions, check out this helpful resource: do you have rosacea psoriasis or eczema.
Ultimately, addressing the root causes of discomfort through pelvic floor physical therapy can lead to significant improvements in overall health and quality of life.
Common Conditions Addressed: Pelvic Floor Physical Therapy
Pelvic floor physical therapy isn’t just about preventing or treating incontinence; it’s a versatile approach to managing a wide array of conditions affecting the pelvic region. Physical therapists specializing in this area use a combination of hands-on techniques, exercises, and education to help patients regain control and function. Understanding the specific conditions addressed allows for more targeted and effective treatment plans.Addressing these conditions often involves a holistic approach, considering the patient’s overall health, lifestyle, and individual needs.
This individualized care ensures that the treatment is not only effective but also sustainable. Physical therapy isn’t a one-size-fits-all solution; it’s about tailoring a plan to meet each patient’s unique circumstances.
Specific Conditions Treated
Pelvic floor physical therapy addresses a diverse range of conditions. These conditions span across various areas of the pelvic region and affect both men and women.
- Urinary incontinence: This encompasses various types, from stress incontinence (leaking with exertion) to urge incontinence (sudden, strong urges to urinate). Physical therapists employ exercises to strengthen the pelvic floor muscles, improve bladder control, and re-educate the nervous system’s response to bladder signals. Outcomes often include reduced incontinence episodes and improved quality of life.
- Fecal incontinence: Similar to urinary incontinence, this condition involves involuntary leakage of stool. Physical therapy focuses on strengthening pelvic floor muscles, improving bowel habits, and promoting better stool consistency. Successful outcomes may include reduced episodes of incontinence and improved bowel regularity. Furthermore, the approach addresses any contributing factors like constipation or irritable bowel syndrome.
- Pelvic organ prolapse: This occurs when pelvic organs, such as the bladder, uterus, or rectum, descend from their normal position. Physical therapy can help support the weakened tissues and pelvic floor muscles through targeted exercises and techniques to reposition the organs. Positive outcomes may include improved comfort, reduced symptoms, and an enhanced ability to perform daily activities without discomfort. The approach often includes education about lifestyle modifications and supportive measures.
- Chronic pelvic pain: This can stem from various underlying causes, including endometriosis, interstitial cystitis, or muscle tension. Physical therapy can help identify and address the root causes of the pain. This might involve releasing tension in surrounding muscles, improving posture, and teaching relaxation techniques. Expected benefits include reduced pain intensity, improved mobility, and enhanced quality of life.
- Postpartum recovery: After childbirth, many women experience pelvic floor dysfunction. Physical therapy plays a crucial role in restoring pelvic floor strength and function. Exercises are tailored to the individual’s specific needs, and the physical therapist educates the patient on the importance of proper posture, body mechanics, and pain management. Positive outcomes often include improved bladder and bowel control, reduced pain, and enhanced overall well-being.
Comparison with Other Treatment Options
While medication and surgery are sometimes used to treat pelvic floor disorders, physical therapy offers a non-invasive and often cost-effective approach. It can be used as a standalone treatment or in conjunction with other therapies. For instance, pelvic floor exercises can complement medications for urinary incontinence. Furthermore, physical therapy often improves the effectiveness of surgical procedures.
| Condition | Description | Physical Therapy Approach | Expected Outcomes |
|---|---|---|---|
| Urinary Incontinence | Involuntary leakage of urine. | Pelvic floor muscle exercises, bladder retraining, biofeedback. | Reduced incontinence episodes, improved bladder control, improved quality of life. |
| Fecal Incontinence | Involuntary leakage of stool. | Pelvic floor muscle exercises, bowel retraining, dietary modifications. | Reduced incontinence episodes, improved bowel regularity, improved quality of life. |
| Pelvic Organ Prolapse | Pelvic organs descending from normal position. | Pelvic floor muscle exercises, posture training, education. | Improved support for pelvic organs, reduced symptoms, improved quality of life. |
| Chronic Pelvic Pain | Persistent pain in the pelvic region. | Identifying root causes, manual therapy, exercise, relaxation techniques. | Reduced pain intensity, improved mobility, improved quality of life. |
| Postpartum Recovery | Pelvic floor dysfunction after childbirth. | Tailored exercises, education on body mechanics, pain management. | Improved bladder and bowel control, reduced pain, improved overall well-being. |
Patient Education and Self-Management
Empowering patients with knowledge and practical skills is crucial for successful pelvic floor rehabilitation. Effective patient education goes beyond simply explaining symptoms and diagnoses. It involves providing actionable strategies for self-management, promoting long-term adherence to treatment plans, and fostering a partnership between the patient and therapist. This collaborative approach ensures that patients are active participants in their recovery journey.Understanding the importance of self-management empowers patients to take control of their health and prevent future problems.
By learning about their specific condition and practicing techniques, they can significantly improve their quality of life and achieve lasting results. A strong focus on patient education promotes independence and empowers patients to actively participate in their healing process.
Importance of Patient Education
Thorough patient education is essential for successful pelvic floor rehabilitation. It equips patients with the knowledge needed to understand their condition, participate actively in their treatment, and maintain long-term health. Effective communication about symptoms, diagnoses, and treatment plans builds trust and encourages patient compliance. Educating patients about self-management techniques ensures they can effectively address their needs independently, leading to sustained improvements.
Strategies for Patient Education and Self-Management
Clear and concise communication is paramount. Use language that patients can easily understand, avoiding medical jargon. Visual aids, such as diagrams and videos, can enhance comprehension. Interactive sessions, group workshops, and personalized handouts further reinforce learning.
- Active Listening and Questioning: Actively listening to patients’ concerns and questions fosters trust and ensures their needs are addressed. Encouraging open communication promotes a collaborative therapeutic relationship, where patients feel empowered to ask questions and seek clarification.
- Tailored Educational Materials: Develop customized educational materials that address specific conditions and treatment plans. These materials should include clear explanations, practical exercises, and visual aids. Examples could include brochures, fact sheets, and videos demonstrating specific exercises.
- Interactive Workshops and Demonstrations: Organize interactive workshops or demonstrations to teach practical techniques. These sessions allow patients to practice exercises under supervision and provide a supportive learning environment. Hands-on practice helps solidify understanding and builds confidence in performing the exercises correctly.
Examples of Educational Materials for Patients
Educational materials should be tailored to individual needs and should be available in multiple formats, including print and digital. This allows patients to access information at their convenience and in formats that best suit their learning preferences. Examples include:
- Brochures: Concise summaries of common pelvic floor conditions, explaining causes, symptoms, and treatment options. They provide a quick overview and can be distributed in waiting areas or during initial consultations.
- Fact Sheets: Detailed information about specific exercises, including instructions, modifications, and precautions. These sheets are valuable for patients to take home and refer to as needed.
- Videos: Visual demonstrations of exercises and self-assessment techniques. Videos can be accessed online or shared via a patient portal, offering flexible learning options.
Creating a Home Exercise Program
A home exercise program is essential for maintaining progress and ensuring long-term results. The program should be tailored to the individual’s needs and progress, and should be reviewed regularly by the therapist. The program should be progressive, starting with basic exercises and gradually increasing the difficulty and duration.
Pelvic floor physical therapy is amazing for so many things, like improving strength and control. But did you know that what you eat can also play a role? For example, incorporating foods high in creatine, like red meat and fish ( foods high in creatine ), might contribute to overall muscle health, which can ultimately benefit your pelvic floor.
This is a great way to consider a holistic approach to your health journey when working with your pelvic floor therapist.
- Individualized Program Design: The program should be tailored to each patient’s specific needs, symptoms, and goals. Consider factors like the patient’s physical abilities, lifestyle, and available resources when designing the program.
- Clear Instructions and Visual Aids: Provide clear and concise instructions for each exercise, including verbal explanations, visual demonstrations, and written instructions. Using diagrams, illustrations, or videos further enhances understanding and reduces potential errors.
- Progression and Modifications: The program should be designed with progressive challenges, allowing patients to gradually increase the intensity, duration, or complexity of the exercises as their condition improves. Modifications should be readily available to adjust the exercises based on individual limitations.
Role of Patient Motivation and Adherence to Treatment
Patient motivation and adherence to the treatment plan are crucial for achieving successful outcomes. Encouraging positive attitudes, providing support, and addressing potential barriers are vital for sustained engagement. Regular follow-up appointments and motivational strategies can help maintain patient commitment.
- Building Patient Confidence: Emphasize the patient’s role in their recovery and highlight the positive outcomes achievable through consistent effort. Recognize and celebrate milestones to maintain motivation and reinforce positive behaviors.
- Addressing Barriers to Adherence: Identify and address potential barriers to adherence, such as lack of time, social support, or understanding of the importance of the exercises. Collaboratively create strategies to overcome these challenges.
- Providing Ongoing Support: Regular follow-up appointments provide opportunities to monitor progress, address concerns, and provide encouragement. Maintain open communication channels, including phone calls, emails, or online forums, to facilitate ongoing support and engagement.
Importance of Lifestyle Modifications
Lifestyle modifications play a vital role in managing pelvic floor dysfunction. These modifications address factors that can impact pelvic floor health, such as posture, diet, stress management, and exercise habits.
- Posture and Body Mechanics: Educating patients on proper posture and body mechanics can significantly reduce strain on the pelvic floor. This includes proper lifting techniques, sitting posture, and standing alignment.
- Stress Management Techniques: Stress can negatively impact pelvic floor function. Incorporating stress-reducing techniques, such as mindfulness, meditation, or yoga, can be beneficial.
- Dietary Considerations: Dietary changes can impact bowel habits, which can influence pelvic floor health. Encouraging a balanced diet and adequate hydration can improve overall health.
Specific Considerations and Populations

Pelvic floor physical therapy isn’t a one-size-fits-all approach. Different life stages and individual circumstances require tailored strategies. Understanding these specific considerations is crucial for effective and compassionate care. This section delves into important factors to consider when working with various patient populations.
Treating Pregnant Women
Pregnancy brings significant changes to the body, impacting the pelvic floor. Understanding these physiological changes is vital for proper assessment and treatment. Pelvic floor muscle function can be affected by hormonal shifts, increased weight, and the growing uterus. Physical therapists specializing in women’s health often employ specific exercises and manual techniques to address the unique needs of pregnant women, focusing on improving pelvic floor strength, mobility, and reducing discomfort.
These interventions can help prepare the body for labor and delivery and support postpartum recovery.
Role of Physical Therapy in Postpartum Recovery
Postpartum recovery encompasses a wide range of needs, from addressing pelvic floor dysfunction to managing general fitness and well-being. Physical therapy plays a critical role in supporting women through this transition. A thorough assessment is key to identifying any issues arising from childbirth, such as diastasis recti (separation of abdominal muscles), urinary incontinence, or pelvic pain. Treatment often includes targeted exercises to restore pelvic floor strength, improve core stability, and address any other related musculoskeletal concerns.
Proper guidance and support during this period are essential for long-term health and well-being.
Treating Individuals with Neurological Conditions
Individuals with neurological conditions, such as multiple sclerosis, spinal cord injury, or stroke, often experience pelvic floor dysfunction. The approach to treatment necessitates a comprehensive understanding of the neurological impact on the pelvic floor muscles. A tailored assessment may involve evaluating the patient’s neurological status, muscle strength, sensation, and range of motion. Physical therapy interventions may include exercises to improve muscle control, pain management techniques, and strategies for improving bowel and bladder function.
Close collaboration with other healthcare professionals is crucial for optimal outcomes.
Treating Older Adults, Pelvic floor physical therapy
Aging often brings changes to the pelvic floor, including decreased muscle tone and flexibility. Physical therapists working with older adults need to consider the potential impact of comorbidities and medications. Treatment plans should prioritize safety, taking into account the individual’s overall health status and functional abilities. This includes modifying exercises to accommodate physical limitations and ensuring the environment is supportive and accessible.
Patient education on self-management strategies and lifestyle adjustments are crucial components of treatment for older adults.
Treating Individuals with Obesity
Obesity can exacerbate pelvic floor dysfunction. Factors such as increased intra-abdominal pressure and altered posture can contribute to pelvic floor weakness or pain. Physical therapists working with this population must consider the unique challenges associated with obesity, such as joint pain, limited mobility, and potential psychological factors. Treatment strategies may include weight management recommendations, exercises tailored to the individual’s capacity, and strategies for reducing intra-abdominal pressure.
Collaboration with other healthcare professionals, such as nutritionists, is often beneficial.
Culturally Sensitive Communication Strategies
Effective communication is essential for building trust and rapport with patients from diverse backgrounds. A culturally sensitive approach acknowledges and respects the patient’s cultural values, beliefs, and preferences. This includes actively listening to the patient’s concerns, using appropriate language and terminology, and being aware of potential cultural barriers to care. Consideration should be given to the patient’s preferred communication style, language, and support systems.
Examples of such strategies include providing written materials in multiple languages, using interpreters when necessary, and demonstrating respect for the patient’s cultural practices.
Advanced Techniques and Emerging Trends
Pelvic floor physical therapy is a dynamic field, constantly evolving with new techniques and research. This evolution reflects the growing understanding of the complex interplay of muscles, nerves, and tissues within the pelvic region and the diverse needs of patients. Advanced techniques are being developed to address specific challenges and enhance treatment outcomes.Advanced techniques build upon foundational knowledge and incorporate innovative approaches to better meet the needs of a diverse patient population.
This includes personalized treatment plans that consider individual factors, such as lifestyle, medical history, and specific goals. The focus is not only on alleviating symptoms but also on empowering patients to take an active role in their recovery.
Advanced Techniques in Pelvic Floor Physical Therapy
Advanced techniques in pelvic floor physical therapy often involve a combination of manual therapy, exercise prescription, and patient education. These methods aim to address complex presentations and improve patient outcomes.
- Biofeedback and Electromyography (EMG): Biofeedback utilizes sensors to provide real-time feedback on muscle activity, enabling patients to learn to control their pelvic floor muscles more effectively. EMG helps to assess muscle activation patterns, identifying imbalances or weaknesses that may be contributing to the patient’s condition. For example, a patient with urinary incontinence may use biofeedback to gain awareness of the specific muscles involved in continence, leading to improved voluntary control.
Combining biofeedback with EMG allows therapists to identify and address specific muscle activation issues more precisely.
- Manual Therapy Techniques: These techniques, including mobilization and myofascial release, can address restrictions and trigger points in the pelvic floor and surrounding tissues. For instance, scar tissue from previous surgeries or trauma can restrict the movement of muscles and nerves, impacting the pelvic floor’s function. Manual therapy can help release these restrictions, improving mobility and reducing pain.
- Specialized Exercise Programs: Exercise programs are increasingly tailored to individual needs and diagnoses. For example, programs for women experiencing pelvic organ prolapse might focus on strengthening specific muscles and promoting tissue support. This approach recognizes the importance of individualized exercise protocols for optimal results.
Emerging Trends and Research
Research in pelvic floor physical therapy is continuously expanding, leading to a deeper understanding of the underlying mechanisms of various conditions. This advancement allows for more effective and targeted treatment approaches.
- Role of the Nervous System: Researchers are exploring the intricate relationship between the nervous system and pelvic floor dysfunction. This includes investigating the impact of stress, anxiety, and other neurological factors on pelvic floor function. This understanding is critical in developing targeted interventions for patients with neurological conditions or those experiencing chronic pain, stress, or anxiety, as these can significantly affect the pelvic floor.
- Personalized Treatment Approaches: The use of advanced diagnostic tools and assessment methods enables the development of more personalized treatment plans. This is crucial in ensuring that interventions are tailored to the specific needs of each patient, leading to improved outcomes.
- Focus on Prevention: Research is increasingly highlighting the importance of preventative strategies, including promoting healthy pelvic floor habits from a young age. This includes educating individuals about the importance of proper posture, avoiding prolonged sitting, and maintaining healthy weight to prevent potential future pelvic floor dysfunction.
Emerging Technologies and Their Potential Impact
New technologies are rapidly transforming pelvic floor physical therapy, offering more precise assessments and treatment options.
- 3D Imaging and Modeling: Three-dimensional imaging techniques provide a detailed visualization of the pelvic floor anatomy, enabling therapists to better understand the structure and function of the pelvic region. This allows for more accurate assessments and personalized treatment plans. For example, 3D imaging can be used to visualize the location and extent of pelvic organ prolapse and to guide surgical interventions or physical therapy.
- Virtual Reality (VR) and Augmented Reality (AR): VR and AR technologies can create immersive and interactive experiences for patients, enabling them to practice exercises and techniques in a safe and controlled environment. This can be particularly beneficial for conditions involving fear or anxiety. A VR simulation of a typical urination process, for example, can help patients visualize and control their pelvic floor muscles.
Interprofessional Collaboration
Interprofessional collaboration is essential in providing comprehensive care for patients with pelvic floor dysfunction.
- Collaboration with other healthcare professionals: Working collaboratively with other healthcare providers, such as gynecologists, urologists, and psychologists, ensures a holistic approach to care. This collaboration allows for the identification and management of contributing factors that might not be apparent during a singular therapy session.
Closing Summary
In conclusion, pelvic floor physical therapy provides a holistic and effective approach to managing a wide range of pelvic floor disorders. The detailed assessment and treatment methods, along with personalized patient education and self-management strategies, empower individuals to regain control and improve their overall well-being. This guide offers a comprehensive understanding of the field, enabling a better comprehension of the various aspects of pelvic floor health and treatment.