The digital rectal exam (DRE) is a vital diagnostic tool used by healthcare professionals to assess various health conditions, particularly in the lower abdomen and pelvic regions. This procedure, while sometimes uncomfortable, plays a crucial role in detecting potential issues, from prostate cancer to other underlying problems. Understanding the purpose, procedure, and implications of a DRE is essential for both patients and healthcare providers.
This comprehensive guide explores the various aspects of the digital rectal exam, from the initial patient preparation to the interpretation of findings. We’ll delve into the steps involved, highlighting the importance of proper technique and patient comfort. Furthermore, we’ll discuss the different scenarios where a DRE is indicated, the potential complications, and the role it plays in a patient’s overall care.
Introduction to Digital Rectal Exam (DRE)
A digital rectal exam (DRE) is a physical examination technique where a healthcare provider uses a gloved finger to examine the rectum and prostate gland. This straightforward yet crucial procedure provides valuable information about the patient’s overall health, particularly concerning the lower gastrointestinal tract and male reproductive system. It’s a relatively quick and non-invasive method to detect potential abnormalities.The purpose of a DRE is multifaceted.
It helps identify abnormalities like tumors, inflammation, or narrowing within the rectum and prostate. Furthermore, it assists in assessing the size, shape, and consistency of the prostate gland in men, which is vital for detecting prostate cancer or other prostate-related conditions. The rationale behind the DRE lies in its ability to detect early warning signs of potentially serious health issues, enabling timely interventions and improved patient outcomes.
While a digital rectal exam (DRE) can be an important diagnostic tool, sometimes it’s helpful to explore alternative approaches to managing health concerns. For example, if you’re dealing with diverticulitis, exploring home remedies like those found in home remedies for diverticulitis might offer relief. Ultimately, though, a DRE remains a crucial part of a comprehensive health evaluation, especially when considering potential underlying issues.
Indications for a Digital Rectal Exam
A DRE is indicated in various clinical scenarios. Common reasons include suspected prostate cancer, rectal bleeding, changes in bowel habits (constipation or diarrhea), or pain in the rectal area. The exam is also used to assess the presence of any masses or abnormalities within the rectum, as well as to evaluate the tone and size of the anal sphincter.
Types of Digital Rectal Exams (DREs)
While the fundamental technique remains the same, the specific focus of a DRE can vary. There are no distinct “types” in the traditional sense. However, the information gathered during the examination might be categorized based on the presenting complaint or suspected condition. A DRE might be used to:
- Assess prostate health in men, particularly to evaluate for enlargement or abnormalities that may indicate prostate cancer or benign prostatic hyperplasia (BPH).
- Evaluate for rectal masses, inflammation, or other abnormalities, such as diverticulitis, fissures, or polyps.
- Screen for possible fecal impaction, which can cause bowel obstructions or discomfort.
- Assess for anal sphincter function and integrity, which is relevant in cases of incontinence or trauma.
A healthcare professional’s clinical judgment and the patient’s symptoms guide the specific focus of the examination.
Procedure and Technique: The Digital Rectal Exam
The digital rectal examination (DRE) is a valuable diagnostic tool used to assess the prostate, rectum, and surrounding structures. It provides crucial information about potential abnormalities, enabling early detection and appropriate management of various conditions. This section delves into the specifics of performing a DRE, outlining the steps, patient positioning, equipment, techniques, and potential complications.
Patient Positioning
Proper patient positioning is paramount for a comfortable and effective DRE. The patient should be positioned on their side, with the knees drawn up towards the chest. This relaxed position facilitates easy access to the rectum and minimizes discomfort for the patient. Alternatively, a supine position with the legs slightly apart and bent at the knees can also be used.
Ever wonder what a digital rectal exam (DRE) checks for beyond just prostate health? Chronic inflammation can manifest in surprising ways, impacting various bodily systems, including the digestive tract. This is why understanding the 11 atypical signs of chronic inflammation, like unusual fatigue or skin rashes, can be incredibly helpful in pinpointing potential underlying issues. For a deeper dive into recognizing these subtle indicators, check out this insightful article on 11 atypical signs of chronic inflammation.
Ultimately, a thorough understanding of these signs can enhance the overall diagnostic process, potentially revealing clues that a DRE might otherwise miss.
The position chosen should prioritize patient comfort and accessibility.
Equipment Required
The equipment needed for a DRE is relatively straightforward. A lubricated, gloved hand is the primary instrument. The examination gloves should be sterile and appropriately sized. A lubricant, such as KY jelly or similar, is crucial for easing insertion and minimizing friction. A lubricant reduces discomfort and aids in the examination’s smooth execution.
Steps Involved in Performing a DRE
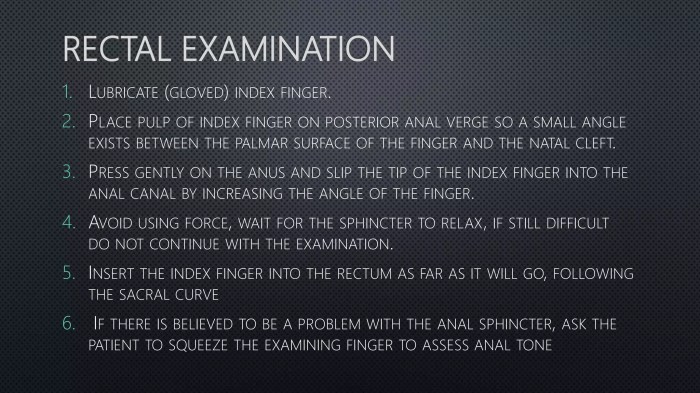
The procedure involves several steps: First, the examiner should wash their hands thoroughly and don sterile gloves. Next, ensure the patient is positioned comfortably. Then, apply a sufficient amount of lubricant to the examining finger. Gently insert the lubricated finger into the rectum, maintaining a slow and controlled approach. Assess the prostate’s size, shape, consistency, and any tenderness or abnormalities.
Finally, withdraw the finger and note any observations.
Comparison of DRE Techniques
| Technique | Advantages | Disadvantages ||—|—|—|| Standard DRE | Simple, readily available, inexpensive. | Can be less sensitive for detecting subtle abnormalities. || DRE with Prostate Massage (for Prostate Assessment) | Aids in assessing prostate secretions and detecting subtle changes. | Can be more uncomfortable for the patient, and requires expertise. || DRE with Rectal Biopsy | Enables tissue sampling for histological analysis.
| Involves a higher degree of invasiveness, potential for complications. |
Potential Complications
While generally safe, DRE carries potential complications. These can include bleeding, rectal trauma, and infection if proper hygiene and technique aren’t adhered to. Bleeding is a common concern and may result from trauma or the presence of underlying conditions. The risk of complications is minimized with careful technique and attention to patient comfort. It is important to carefully monitor the patient for any signs of discomfort or complications during and after the procedure.
Indications and Contraindications
A digital rectal exam (DRE) is a valuable diagnostic tool, but its use must be carefully considered. Understanding when a DRE is appropriate and when it’s contraindicated is crucial for patient safety and effective healthcare. This section delves into the specific medical conditions that necessitate a DRE, situations where it’s contraindicated, and the importance of assessing the patient’s medical history.Performing a DRE requires a nuanced understanding of the patient’s overall health.
Careful consideration of both potential benefits and risks is paramount to ensuring a safe and informative procedure. The following sections Artikel specific considerations regarding indications and contraindications for this procedure.
Medical Conditions Requiring a DRE, The digital rectal exam
Properly performed DREs can reveal critical information about various medical conditions. Prostate cancer screening, for instance, frequently relies on DREs to detect abnormalities in the prostate. Rectal bleeding, a common symptom, often requires a DRE to assess the source and extent of the bleeding. Conditions like inflammatory bowel disease and rectal prolapse can also necessitate a DRE for diagnosis and monitoring.
Contraindications for a DRE
Certain situations pose risks to patients, making a DRE inappropriate. Acute anal fissures or severe hemorrhoids can lead to discomfort and complications during the procedure. Active infections of the rectum, such as severe inflammatory conditions, should preclude a DRE. Patients with recent rectal surgery or trauma should also be assessed carefully.
Patient History Assessment
Prior to performing a DRE, it is critical to assess the patient’s medical history. This includes a review of any recent surgeries, previous rectal issues, and any underlying medical conditions that might impact the procedure. A thorough history, including any allergies or medication use, is crucial for identifying potential complications. For example, a patient with a history of anticoagulant use might require a modified approach to minimize bleeding risk.
Using a DRE to Rule Out Conditions
A DRE can be a valuable tool in ruling out certain conditions. For example, if a patient presents with lower abdominal pain, a DRE can help distinguish between possible causes, such as an inflamed appendix or a prostate problem. In cases of rectal bleeding, a DRE can help differentiate between conditions like hemorrhoids and more serious issues like colorectal cancer.
The results of the DRE, along with other diagnostic tests, can contribute to a more comprehensive understanding of the patient’s condition.
Tailoring the Procedure Based on Patient Condition
The DRE procedure should be adapted to the individual patient’s condition. For example, if the patient has a history of anal fissures, a gentler approach is necessary to avoid exacerbating the condition. In patients with certain medical conditions or a history of bleeding disorders, the procedure might require specific precautions. Using appropriate lubrication and employing a gentle technique can minimize discomfort and complications.
Patient Preparation and Comfort
Preparing a patient for a digital rectal exam (DRE) involves more than just scheduling the appointment. It encompasses creating a comfortable and reassuring environment to help patients feel at ease and reduce anxiety about the procedure. Effective preparation ensures the exam proceeds smoothly and yields accurate results. The focus should be on clear communication, respecting patient privacy, and addressing any concerns they may have.A well-prepared patient is more likely to cooperate fully, allowing for a thorough and accurate examination.
This cooperation, in turn, minimizes the discomfort associated with the procedure and ultimately leads to a better overall experience. Careful attention to patient preparation is a crucial element in providing high-quality healthcare.
Strategies for Preparing the Patient
Effective patient preparation begins with clear communication. The healthcare provider should explain the purpose of the DRE, the procedure itself, and any potential sensations the patient might experience. This proactive approach helps the patient feel informed and empowered. This explanation should be tailored to the individual’s understanding and concerns.
Methods to Ensure Patient Comfort
Creating a comfortable environment is paramount. Using a warm examination room, ensuring privacy, and offering a reassuring presence can significantly reduce anxiety. Providing a comfortable position, such as having the patient lie on their side with their knees bent, can also contribute to their comfort. Explaining the expected sensations and allowing the patient to ask questions can ease apprehension.
Table Outlining Various Patient Preparation Strategies
| Preparation Strategy | Description | Benefits |
|---|---|---|
| Clear Explanation | Providing a detailed, patient-centered explanation of the purpose, procedure, and potential sensations. | Reduces anxiety and improves patient understanding and cooperation. |
| Privacy and Respect | Ensuring a private and respectful environment. | Builds trust and reduces patient discomfort. |
| Comfortable Setting | Maintaining a warm and comfortable examination room, providing a supportive presence, and using appropriate lighting. | Creates a calming atmosphere and reduces anxiety. |
| Positioning | Helping the patient assume a comfortable position (e.g., lying on their side with knees bent). | Reduces discomfort and facilitates the exam. |
| Open Communication | Encouraging questions and addressing concerns promptly and empathetically. | Promotes a sense of control and understanding for the patient. |
Addressing Patient Concerns and Anxieties
Patients may have various concerns about a DRE, ranging from discomfort to potential implications of the results. Openly acknowledging and addressing these concerns is crucial. Empathy and active listening are vital in creating a trusting environment where patients feel comfortable sharing their anxieties. Reassuring the patient that the exam is a routine procedure that aids in diagnosis and treatment can help alleviate anxieties.
Table Comparing Different Methods for Patient Education and Preparation
| Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Verbal Explanation | Directly explaining the procedure in a clear and concise manner. | Immediate feedback and clarification. | May not be as comprehensive as other methods. |
| Written Materials | Providing written information about the procedure, including diagrams or illustrations. | Provides ongoing reference and allows for independent review. | May not be as engaging as other methods for all patients. |
| Video Demonstration | Showing a video of the procedure. | Provides a visual representation of the procedure, aiding comprehension. | May not be suitable for all patients due to sensitivity or anxiety. |
Findings and Interpretation
A digital rectal exam (DRE) allows for the assessment of the rectum and prostate, providing crucial information about potential underlying conditions. Interpreting the findings requires careful attention to detail and a thorough understanding of the potential implications of various sensations and observations. The examiner must be able to distinguish normal from abnormal findings and communicate these observations accurately to the healthcare provider.The DRE is not a definitive diagnostic tool.
It serves as a valuable initial screening method. Findings must be considered in conjunction with other diagnostic tests and the patient’s overall clinical picture. A thorough understanding of the possible interpretations is essential for effective communication and appropriate patient management.
Identifying Various Findings
The examination involves palpating the rectal wall and, if applicable, the prostate gland. The examiner feels for abnormalities such as masses, tenderness, or changes in consistency. Careful attention should be paid to the size, shape, and texture of any observed abnormalities. For example, a smooth, firm mass might differ from a hard, irregular one. The consistency of the stool can also be a crucial observation, providing insights into potential digestive issues.
Significance of Different Findings
Various findings during a DRE have different implications. A mass, for instance, could indicate a tumor, polyp, or other growths. The location, size, and consistency of the mass are crucial factors in determining the nature of the condition. Tenderness in the rectal area might suggest inflammation, infection, or other irritations. Any abnormality should be meticulously noted.
Importance of Accurate Documentation
Detailed documentation of the findings is critical. A comprehensive record should include the size, shape, consistency, and location of any observed abnormalities. The presence or absence of tenderness, the overall condition of the rectal wall, and any relevant patient symptoms should be documented. Accurate documentation is essential for communication with the healthcare provider and for follow-up evaluations.
Table of Potential Findings and Interpretations
| Finding | Possible Interpretations |
|---|---|
| Smooth, firm mass, 2cm in diameter, located in the upper rectum | Possible tumor, benign polyp, or other growth; further investigation needed. |
| Hard, irregular mass, 1cm in diameter, located near the prostate | Possible prostate cancer; urgent referral for further evaluation is necessary. |
| Tenderness in the prostate gland | Possible prostatitis, infection, or inflammation; further evaluation needed. |
| Normal consistency, no tenderness | Indicates no apparent abnormalities. |
| Presence of blood in the stool | Indicates potential bleeding source within the digestive tract; further investigation needed. |
Communicating Findings to the Healthcare Provider
Accurate and comprehensive communication of findings is essential. The examiner should clearly describe the findings, using appropriate medical terminology and emphasizing any unusual or concerning aspects. The examiner should also relay any relevant patient symptoms, such as pain, discomfort, or changes in bowel habits. A concise, yet detailed summary of the exam, including the specific location, size, consistency, and any notable tenderness or masses, should be provided.
Role of DRE in Diagnosis

The digital rectal exam (DRE) remains a crucial tool in the initial assessment of various conditions affecting the rectum, prostate, and surrounding structures. While not a definitive diagnostic tool on its own, its simplicity and accessibility make it an important component of a comprehensive evaluation. A skilled examiner can glean valuable information about the size, shape, consistency, and mobility of the prostate and surrounding tissues, often revealing subtle changes that may indicate underlying pathology.DRE findings are often integrated with other diagnostic methods, such as blood tests, imaging studies, and biopsies, to reach a conclusive diagnosis and develop an appropriate treatment plan.
This integrated approach maximizes the chances of accurate diagnosis and effective management.
Prostate Cancer Diagnosis
DRE plays a vital role in the early detection of prostate cancer. Changes in prostate size, shape, consistency, or mobility can signal potential abnormalities. For instance, a hard, irregular, or nodular prostate can suggest the presence of cancerous tissue. However, it is crucial to remember that not all hard prostates are cancerous, and other conditions can produce similar findings.
A meticulous physical examination, along with other diagnostic tests, is essential for accurate assessment.
Other Conditions Diagnosed with DRE
The DRE is also useful in diagnosing conditions other than prostate cancer. Rectal prolapse, hemorrhoids, fistulas, polyps, and other lesions or masses in the rectum or surrounding areas can be detected during the examination. Changes in the surrounding tissues, such as tenderness or inflammation, can also indicate problems such as infections or inflammatory bowel disease.
How DRE Findings Guide Treatment
DRE findings can significantly aid in determining the course of treatment. The size, consistency, and mobility of the prostate, as well as the presence of any masses or lesions, can provide crucial information to the physician. This information assists in deciding whether further investigations, such as biopsies, ultrasound, or MRI scans, are necessary. For example, if a DRE reveals an enlarged, hard prostate, a biopsy is likely to follow to confirm or rule out cancer.
Similarly, if the DRE detects a mass in the rectum, a colonoscopy may be recommended for further evaluation.
Comparison of DRE Results with Other Diagnostic Tools
| Feature | Digital Rectal Exam (DRE) | Prostate Biopsy | Transrectal Ultrasound (TRUS) ||—————–|—————————|—————–|—————————–|| Sensitivity | Moderate | High | High || Specificity | Moderate | Moderate | High || Cost | Low | Moderate | Moderate || Invasiveness | Non-invasive | Invasive | Minimally invasive || Time required | Short | Variable | Short || Information on surrounding tissues | Limited | Limited | High |This table highlights the comparative strengths and weaknesses of different diagnostic methods.
The choice of diagnostic approach often depends on the specific clinical context and the need for a comprehensive assessment.
Limitations of DRE in Diagnosis
The DRE has limitations in diagnosing certain conditions. Its accuracy is heavily reliant on the examiner’s experience and skill. Furthermore, early-stage prostate cancer may not be detectable by DRE, and some benign conditions can mimic the findings of prostate cancer. Also, the DRE provides limited information on the surrounding tissues, which may require additional investigations. The examination might also be uncomfortable or even painful for some patients, impacting the quality of the information obtained.
Safety and Hygiene Practices
Maintaining meticulous safety and hygiene standards is paramount during a digital rectal exam (DRE). Adherence to these practices not only protects the patient but also safeguards the healthcare provider from potential infections and cross-contamination. Proper hand hygiene, appropriate personal protective equipment (PPE), and meticulous waste disposal procedures are critical components of a safe DRE.Performing a DRE involves direct contact with the patient’s body, and this inherent risk necessitates stringent precautions.
A commitment to safety procedures safeguards both the patient and the healthcare professional from potential hazards.
Ever wondered about the digital rectal exam? It’s a pretty straightforward procedure, but sometimes, people are more curious about seemingly unrelated topics like whether popping pimples is good or bad for your skin. The truth is, just like a digital rectal exam has its purpose and procedure, proper skincare practices are important. For more on whether popping pimples is harmful, check out this helpful guide: is popping pimples bad for my skin.
Ultimately, both the digital rectal exam and skincare involve understanding the body and taking care of it in the right way.
Importance of Hand Hygiene
Proper hand hygiene is the cornerstone of infection control in healthcare settings. Thorough handwashing before and after every DRE is essential. This practice eliminates transient microorganisms, significantly reducing the risk of transmitting pathogens. A meticulous handwashing technique, including using soap and water for at least 20 seconds, is crucial. Alcohol-based hand sanitizers are also acceptable alternatives when handwashing facilities are unavailable.
Use of Personal Protective Equipment (PPE)
Appropriate PPE is essential to minimize the risk of cross-contamination during a DRE. Gloves are a critical element of PPE. Using disposable, non-latex gloves prevents the transmission of pathogens from the patient to the healthcare professional. Eye protection, such as goggles or a face shield, can also be used to prevent splashes or droplets from reaching the eyes, though not always required in this specific procedure.
The type of PPE used should be determined based on the anticipated level of risk and local protocols.
Prevention of Cross-Contamination
Cross-contamination, the transmission of microorganisms from one source to another, is a serious concern in healthcare. Strict adherence to hand hygiene protocols and the use of appropriate PPE minimize the risk. Using single-use equipment whenever possible and properly disposing of contaminated materials further reduces the likelihood of spreading infections. Regular cleaning and disinfection of examination equipment and surfaces are also essential to maintain a hygienic environment.
Standard Safety Procedures for DRE
| Procedure | Description |
|---|---|
| Hand Hygiene | Thoroughly wash hands with soap and water for at least 20 seconds before and after the examination. Use alcohol-based hand sanitizer as an alternative if handwashing facilities are not immediately available. |
| PPE | Wear disposable non-latex gloves during the entire procedure. Consider additional PPE such as eye protection if there is a risk of splashes or droplets. |
| Equipment Use | Use single-use examination tools whenever possible. If reusable equipment is used, ensure proper cleaning and disinfection following established protocols. |
| Waste Disposal | Dispose of used gloves and other contaminated materials in designated biohazard waste receptacles. Follow local regulations for sharps disposal. |
| Environmental Cleaning | Clean and disinfect the examination area and all surfaces that may have come into contact with bodily fluids after the procedure. |
Appropriate Disposal of Used Equipment
Proper disposal of used equipment is critical to preventing the spread of infection. Contaminated gloves, instruments, and other materials should be placed in appropriately labeled biohazard containers. Sharps, such as lancets or needles, should be disposed of in puncture-resistant containers. Adherence to local regulations regarding the disposal of medical waste is essential. Proper waste management procedures prevent the release of pathogens into the environment.
Cultural Sensitivity and Communication
A crucial aspect of performing a digital rectal exam (DRE) is understanding and respecting the diverse cultural backgrounds of patients. Effective communication is paramount, not just for patient comfort but also for obtaining accurate and reliable information during the examination. Cultural nuances can significantly influence how patients perceive and react to medical procedures, impacting their willingness to participate and their overall experience.Cultural sensitivity in healthcare involves recognizing and appreciating the differences in beliefs, values, and practices that may influence a patient’s perspective on health, illness, and medical procedures.
This requires healthcare providers to be mindful of potential biases and to approach each interaction with empathy and respect. By actively listening to and validating patient concerns, healthcare providers can foster a more trusting and collaborative environment, ultimately improving the quality of care.
Addressing Patient Concerns and Anxieties
Understanding that patients may have varying levels of comfort and familiarity with a DRE is essential. Concerns may stem from cultural beliefs about bodily privacy, traditional medical practices, or personal experiences. Open and honest communication, combined with active listening, is crucial to address these anxieties. For example, some cultures may emphasize the importance of a female healthcare provider for a DRE involving a female patient.
Therefore, providers should be prepared to accommodate such preferences.
Effective Communication Strategies
Clear and concise communication is vital. Use simple, straightforward language, avoiding medical jargon. Active listening, demonstrating empathy, and asking clarifying questions to ensure understanding are essential components of effective communication. For example, if a patient expresses discomfort, acknowledge their feelings and work together to find solutions that address their concerns.
Culturally Sensitive Language and Communication Approaches
| Cultural Considerations | Sensitive Language/Approaches |
|---|---|
| Privacy Concerns (some cultures emphasize modesty) | “I understand that this exam might be a little uncomfortable. We can take our time, and I will do everything I can to make you feel as comfortable as possible.” |
| Female Patients (some cultures may prefer a female healthcare provider) | “We can arrange for a female healthcare provider if you would like.” |
| Religious Beliefs (certain religions have specific dietary restrictions or practices) | “Please tell me about any dietary restrictions or religious practices that might affect this procedure.” |
| Language Barriers | “I have a translator available if you would like one.” |
| Non-verbal Communication | “Observe and respond to non-verbal cues. Be attentive to their body language.” |
Addressing Patient Preferences
Patient preferences regarding the DRE procedure should be taken into account. This includes factors like the position during the examination, the use of lubricant, and the presence of a chaperone. Open dialogue and active listening are critical to understanding and accommodating these preferences. For instance, if a patient prefers a chaperone, arrange for one who can communicate effectively with the patient.
Respecting the patient’s choices can enhance their comfort and cooperation.
Final Thoughts
In conclusion, the digital rectal exam remains a critical component of a thorough diagnostic approach. Its ability to detect abnormalities, coupled with proper patient preparation and communication, makes it a valuable tool in healthcare. While the procedure may not be pleasant, understanding its significance and the steps involved can ease concerns and improve the overall patient experience. By recognizing the indications, contraindications, and appropriate safety measures, both patients and healthcare professionals can approach the DRE with confidence and ensure optimal health outcomes.










