Weight loss surgery for PCOS risks and info provides a comprehensive overview of the potential benefits and drawbacks of surgical interventions for individuals with Polycystic Ovary Syndrome (PCOS). We’ll explore the link between PCOS and weight, different surgical procedures, potential risks and complications, and crucial considerations before, during, and after the surgery, alongside nutritional guidance and the impact on fertility.
This in-depth look will empower you to make informed decisions about your health.
The surgical procedures available for weight loss, such as gastric bypass and sleeve gastrectomy, are explored in detail, with a focus on how these procedures might affect individuals with PCOS. The content includes detailed comparisons of the potential risks and benefits of each procedure. Further information about pre- and post-operative considerations, including nutritional needs and support systems, will be presented.
Introduction to PCOS and Weight Loss Surgery
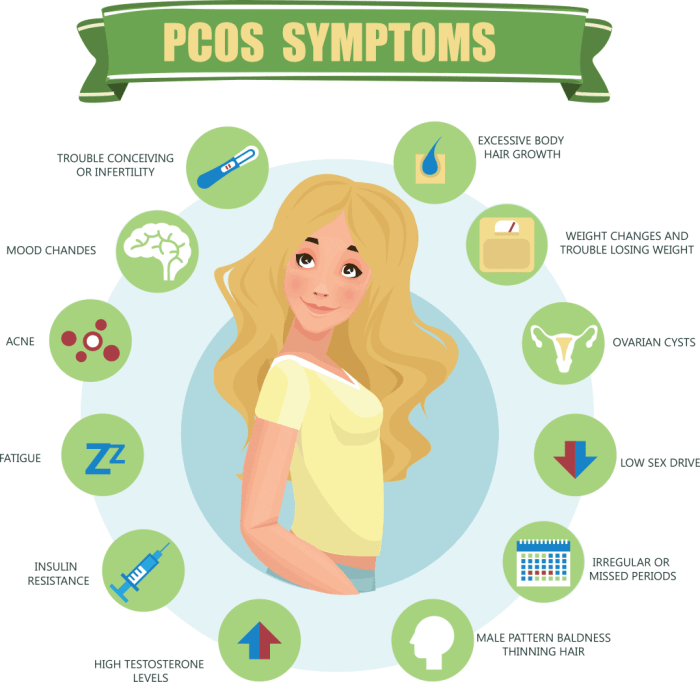
Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects women of reproductive age. Characterized by an imbalance in reproductive hormones, PCOS often leads to irregular periods, excess hair growth, acne, and difficulty conceiving. Beyond these symptoms, PCOS frequently presents with insulin resistance, a condition where the body doesn’t effectively use insulin, the hormone responsible for regulating blood sugar.
This insulin resistance can contribute significantly to weight gain and obesity, often making weight management a significant challenge for those with PCOS.The link between PCOS and weight issues is complex. Insulin resistance in PCOS often leads to higher levels of androgens (male hormones), which can increase appetite and fat storage. Furthermore, the hormonal imbalances associated with PCOS can disrupt metabolism, making it harder to burn calories and maintain a healthy weight.
Weight gain, in turn, exacerbates PCOS symptoms, creating a vicious cycle. Therefore, addressing weight concerns is often a crucial part of managing PCOS. Weight loss surgery can be a viable option for those struggling to lose weight through diet and exercise alone, especially when weight is a significant factor in PCOS symptoms.
Types of Weight Loss Surgeries
Weight loss surgeries, also known as bariatric surgeries, aim to reduce the size of the stomach or change how the small intestine absorbs nutrients. Different procedures have varying degrees of impact on the digestive system. Understanding these procedures is essential for anyone considering weight loss surgery.
Comparison of Weight Loss Surgical Procedures
| Procedure | Description | Potential Risks | Benefits |
|---|---|---|---|
| Gastric Bypass | Creates a small pouch at the top of the stomach and reroutes a portion of the small intestine. | Potential complications include leaks, obstructions, and nutritional deficiencies if not managed properly. There is a risk of dumping syndrome, a condition causing nausea and diarrhea after eating. | Generally considered more effective for long-term weight loss compared to other procedures. Reduces the absorption of calories and promotes significant hormonal changes that can help manage PCOS symptoms like insulin resistance. |
| Sleeve Gastrectomy | Reduces the size of the stomach by removing a large portion of it, creating a sleeve-shaped stomach. | Potential complications include leaks, obstructions, and nutritional deficiencies. Some patients may experience dumping syndrome. | Less invasive than gastric bypass, leading to a lower risk of certain complications. It is effective in promoting significant weight loss and can improve PCOS-related hormonal imbalances. |
| Adjustable Gastric Banding | A band is placed around the upper part of the stomach, creating a small pouch. The band’s tightness can be adjusted. | Potential complications include slippage, band erosion, and the need for further surgeries. May not provide as much weight loss compared to other procedures. | Less invasive than gastric bypass or sleeve gastrectomy. It allows for gradual weight loss and some improvement in PCOS-related hormonal issues. |
Important Considerations
Weight loss surgery is a significant decision. Thorough evaluation by a multidisciplinary team, including a surgeon, endocrinologist, and dietitian, is crucial. This team can assess individual needs and risks, ensuring that surgery is the most appropriate option and a personalized treatment plan can be implemented. Patients should be prepared for significant lifestyle changes, including dietary modifications, nutritional supplements, and ongoing follow-up care.
Weight loss surgery is not a quick fix; it’s a commitment to a long-term healthier lifestyle. Patients should be aware that, as with any major surgery, there are potential risks.
Risks Associated with Weight Loss Surgery for PCOS
Choosing weight loss surgery is a significant decision, and understanding the potential risks is crucial. While these procedures can offer substantial benefits for individuals with PCOS, they also come with potential complications. It’s essential to weigh the risks against the potential improvements in health and well-being, and to have an open and honest discussion with your healthcare provider.
Short-Term Complications
Short-term complications following weight loss surgery can range from mild discomfort to more serious issues. These complications often arise during the immediate postoperative period and typically include nausea, vomiting, and abdominal pain. Blood clots, infections, and leaks from the surgical site are also potential risks. The severity and frequency of these complications can vary based on individual factors, the specific surgical technique employed, and the patient’s overall health.
Long-Term Risks Specific to PCOS Patients
PCOS patients may experience unique long-term complications due to the interplay between the hormonal imbalances of PCOS and the surgical procedures. For instance, the hormonal fluctuations can potentially affect the body’s ability to regulate blood sugar levels post-surgery. This could increase the risk of developing diabetes or worsen existing conditions. Furthermore, PCOS-related issues like irregular periods or polycystic ovaries might be exacerbated or influenced by the surgical intervention.
A deeper understanding of these potential interactions is vital for personalized care.
Nutritional Deficiencies
Significant nutritional deficiencies can occur after weight loss surgery, impacting overall health, including those with PCOS. Post-surgery, the body may struggle to absorb essential vitamins and minerals from food, potentially leading to deficiencies in vitamins like vitamin D, vitamin B12, and iron. These deficiencies can have severe consequences, especially in individuals with PCOS, as these nutritional imbalances can exacerbate existing PCOS symptoms or contribute to new health problems.
For example, iron deficiency can worsen fatigue and anemia, while vitamin D deficiency can impact insulin sensitivity, a crucial factor in managing PCOS.
Comparison of Risks: Surgery vs. Lifestyle Changes
Lifestyle changes, while potentially less dramatic in their immediate effects, are not without risk. For instance, individuals with PCOS might experience emotional setbacks or frustrations in their weight loss journey. Conversely, weight loss surgery has immediate and long-term risks that must be considered. The risks of surgery should be weighed against the potential benefits of surgery versus the long-term risks of lifestyle changes alone.
It is crucial to remember that individual responses vary, and a thorough discussion with a healthcare provider is essential.
Navigating the world of weight loss surgery for PCOS can be tricky, and understanding the potential risks is crucial. While exploring different options, it’s also important to consider the safety of alternative dietary choices, like raw milk. Learning about the potential health implications of consuming raw milk, as discussed in this helpful resource ( is raw milk safe ), can broaden your understanding of holistic health.
Ultimately, thorough research and open communication with your doctor remain essential when considering weight loss surgery options for PCOS.
Psychological Effects
The psychological impact of weight loss surgery on individuals with PCOS should not be overlooked. The procedure itself can be emotionally challenging, especially for those who have struggled with their weight for an extended period. There’s a potential for body image issues, feelings of anxiety, or even depression. This is a multifaceted issue requiring attention and support.
Common Complications Table
| Complication | Probability | Symptoms | Management |
|---|---|---|---|
| Nausea and Vomiting | High | Feeling unwell, stomach upset, retching | Medications, dietary modifications, close monitoring |
| Infection | Moderate | Fever, redness, swelling, pus | Antibiotics, wound care |
| Blood Clots | Low | Pain, swelling, redness in the leg or arm | Compression stockings, blood thinners |
| Nutritional Deficiencies | High | Fatigue, hair loss, anemia | Supplementation, dietary counseling, regular blood tests |
| Leakage | Low | Pain, fever, infection | Surgical repair, close monitoring |
Benefits of Weight Loss Surgery for PCOS
Weight loss surgery, often a last resort but sometimes a life-changing intervention, can significantly improve the lives of individuals with Polycystic Ovary Syndrome (PCOS). This procedure, when combined with lifestyle modifications, can lead to substantial improvements in PCOS symptoms, hormonal balance, and overall well-being. It’s crucial to remember that weight loss surgery is not a magic bullet and must be approached with a holistic view of health, encompassing lifestyle changes and ongoing medical support.Weight loss surgery, particularly procedures like gastric bypass or sleeve gastrectomy, can lead to substantial improvements in PCOS symptoms.
This improvement often stems from a reduction in circulating androgens (male hormones), which are frequently elevated in women with PCOS. This, in turn, can help restore hormonal balance. The reduction in circulating androgens is frequently accompanied by a significant drop in insulin resistance, another key characteristic of PCOS.
Improved Hormonal Imbalances
Weight loss following surgery can significantly impact hormonal imbalances associated with PCOS. A reduced body mass index (BMI) often leads to a decrease in insulin levels, which is crucial for regulating androgen production. This regulation is often accompanied by a return to a more normal menstrual cycle and a reduction in acne and excess hair growth. These improvements aren’t always immediate, and the experience varies between individuals, but consistent monitoring and adjustments in medication can significantly improve outcomes.
Enhanced Fertility and Menstrual Regularity
Weight loss surgery can positively influence fertility and menstrual regularity in women with PCOS. By addressing the underlying hormonal imbalances, the surgery often helps restore ovulation cycles, making it easier to conceive naturally. This is not a guarantee, but it is a significant benefit that has been observed in many cases. Improved menstrual regularity often follows, with periods becoming more predictable and less problematic.
Many women report experiencing reduced symptoms of irregular periods and painful cramps.
Positive Outcomes and Examples
Numerous case studies demonstrate the positive impact of weight loss surgery on individuals with PCOS. One study observed a marked decrease in hirsutism (excessive hair growth) and acne in women who underwent surgery, alongside improved insulin sensitivity. Another study reported a substantial improvement in fertility rates, enabling natural conception in women who had previously struggled. These positive outcomes highlight the potential of surgery as a treatment option, but they should be interpreted within the context of individual experiences and the need for ongoing medical support.
Summary of Potential Improvements
| Aspect | Improvement | Example |
|---|---|---|
| Hormonal Imbalances | Reduced androgens, improved insulin sensitivity, normalized estrogen levels | A woman with PCOS experiences a decrease in acne and excess hair growth after surgery. |
| Fertility | Improved ovulation, increased chances of natural conception | A woman with PCOS who had struggled with infertility successfully conceives after surgery. |
| Menstrual Regularity | More predictable and less problematic periods | A woman with PCOS reports a more regular menstrual cycle with fewer painful cramps after surgery. |
| Metabolic Health | Reduced insulin resistance, improved blood sugar control | A woman with PCOS experiences a significant decrease in blood sugar levels after surgery. |
Pre- and Post-Operative Considerations for PCOS Patients
Embarking on weight loss surgery is a significant decision, especially for individuals with PCOS. Careful pre-operative evaluation and post-operative management are crucial for maximizing the success and minimizing potential complications. This involves a multifaceted approach that considers the unique challenges presented by PCOS, ensuring optimal outcomes for patients.Pre-operative planning is not merely about the surgery itself; it’s about creating a foundation for long-term health improvement.
Post-operative support is equally vital, providing the necessary tools and guidance for patients to sustain their progress and address potential challenges.
Pre-Operative Evaluation Process
The pre-operative evaluation process for PCOS patients considering weight loss surgery is comprehensive and individualized. This process ensures that the patient is a suitable candidate for the procedure and that potential risks are addressed proactively. A thorough medical history, including a detailed assessment of PCOS symptoms, is critical. Blood tests to assess overall health, including liver function, kidney function, and hormone levels, are essential.
A complete metabolic panel, along with assessment of cardiovascular risk factors, are also necessary. Nutritional and psychological evaluations help assess the patient’s readiness for lifestyle changes, a critical component of post-surgical success.
Importance of Pre-Operative Lifestyle Modifications
Pre-operative lifestyle modifications are vital for PCOS patients. These modifications not only improve overall health but also contribute to a smoother recovery process and improved long-term outcomes. A tailored dietary plan, emphasizing whole foods and portion control, helps manage insulin resistance, a common feature of PCOS. Increased physical activity, even moderate exercise, can positively impact insulin sensitivity and contribute to weight management.
Stress management techniques, such as yoga or meditation, can also be beneficial. These changes help the body better prepare for the surgical procedure and promote healthy habits for long-term success.
Importance of Post-Operative Support and Management
Post-operative support is paramount for PCOS patients. It involves ongoing guidance and support to help patients adapt to their new lifestyle and address potential complications. Regular follow-up appointments with the surgical team and endocrinologist are essential to monitor progress, adjust medications, and address any emerging issues. This ensures the patient receives the personalized care they need to navigate the post-surgical period.
Crucial Factors to Consider Before Surgery
- Detailed medical history, including a thorough assessment of PCOS symptoms and current medications.
- Comprehensive blood tests to assess overall health, including hormone levels, liver function, and kidney function.
- Nutritional and psychological evaluations to assess the patient’s readiness for lifestyle changes and potential emotional support needs.
- Assessment of cardiovascular risk factors and pre-existing conditions.
- Discussion of potential risks and benefits, including long-term complications.
- Realistic expectations regarding weight loss and health improvements.
Thorough preparation before surgery minimizes potential complications and maximizes the likelihood of a positive outcome.
Recommended Specialists Involved in the Process
- Surgeon specializing in weight loss surgery
- Endocrinologist to manage PCOS-related hormonal imbalances.
- Nutritionist to create a personalized dietary plan.
- Psychologist or therapist for emotional support and coping strategies.
- Registered dietitian to provide ongoing nutritional guidance.
- Diabetes educator to address insulin resistance and diabetes management.
Collaboration between specialists is essential to address the complex needs of PCOS patients undergoing weight loss surgery.
Post-Surgical Dietary Recommendations
- Focus on whole foods: Prioritize fruits, vegetables, lean proteins, and whole grains. This approach provides essential nutrients and promotes satiety.
- Portion control: Even with a healthy diet, portion sizes must be carefully managed. This is vital to prevent regaining lost weight.
- High-fiber foods: Incorporate foods rich in fiber to promote digestive health and manage blood sugar levels. Fiber slows down the absorption of sugars, which can help regulate insulin response.
- Limit processed foods, sugary drinks, and unhealthy fats: These items contribute to weight gain and can exacerbate PCOS symptoms. Substituting healthier alternatives is key to long-term success.
- Regular meals and snacks: Avoid skipping meals, as this can lead to blood sugar fluctuations and potential cravings.
- Hydration: Drink plenty of water throughout the day to aid digestion and overall well-being.
Post-surgical dietary adjustments are essential for long-term weight management and maintaining overall health. Examples of tailored plans should be discussed with the nutritionist or dietitian.
Nutritional Considerations and PCOS
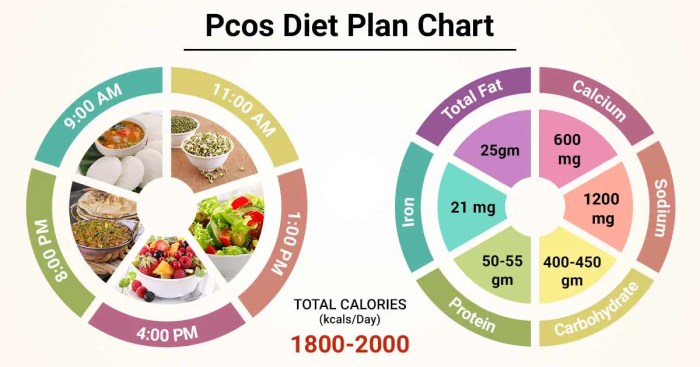
Proper nutrition plays a crucial role in managing PCOS symptoms and preparing for weight loss surgery. A tailored dietary approach can significantly impact insulin resistance, inflammation, and other hormonal imbalances often associated with PCOS. Understanding how PCOS affects nutrient absorption and metabolism is essential for creating a personalized dietary plan that supports overall health and recovery. This section delves into the importance of pre-surgery, intra-surgery, and post-surgery nutritional strategies for PCOS patients.Understanding how PCOS impacts metabolism and nutrient absorption is critical for creating an effective dietary plan.
Insulin resistance, a common feature of PCOS, affects how the body utilizes glucose and other nutrients. This can lead to difficulties with maintaining stable blood sugar levels and proper nutrient absorption. Furthermore, hormonal imbalances within PCOS can influence appetite regulation, leading to cravings and difficulties in controlling food intake.
Navigating weight loss surgery for PCOS risks and information can be tricky. While exploring those options, it’s also interesting to see how advancements in continuous glucose monitoring, like continuous glucose monitoring the arrival of dexcom 5 , are impacting diabetes management. Ultimately, understanding the potential risks and benefits of weight loss surgery for PCOS remains crucial for making informed decisions about your health journey.
Pre-Surgery Dietary Guidelines for PCOS
A healthy pre-surgery diet for PCOS patients aims to improve insulin sensitivity, manage weight, and reduce inflammation. A diet rich in whole foods, lean proteins, and complex carbohydrates is essential. These foods provide sustained energy and essential nutrients without spiking blood sugar levels. Prioritizing fiber-rich foods, like fruits, vegetables, and whole grains, is crucial for regulating blood sugar and promoting satiety.
- Focus on whole foods: Emphasize fruits, vegetables, lean proteins (like fish, poultry, and beans), and whole grains.
- Control portion sizes: Careful portion control helps manage calorie intake and promotes gradual weight loss.
- Prioritize fiber intake: High-fiber foods aid digestion, promote satiety, and regulate blood sugar levels. Examples include oats, lentils, and leafy greens.
- Limit processed foods, refined sugars, and unhealthy fats: These foods contribute to inflammation and can worsen PCOS symptoms. Limit intake of sugary drinks, white bread, and fried foods.
- Hydration: Adequate water intake is vital for overall health and helps with nutrient absorption.
Impact of PCOS on Nutrient Absorption and Metabolism
PCOS can impact the absorption and metabolism of several nutrients. For instance, insulin resistance can impair the body’s ability to utilize glucose, leading to elevated blood sugar levels. This, in turn, can affect the absorption of other nutrients, like vitamins and minerals. Additionally, hormonal imbalances within PCOS can alter the body’s metabolism of fats, proteins, and carbohydrates.
This disruption can make it challenging to manage weight and maintain overall health.
Dietary Impact on PCOS Symptoms
Different dietary approaches can significantly affect PCOS symptoms. For example, a diet high in processed foods and refined sugars can exacerbate insulin resistance and worsen hormonal imbalances. Conversely, a diet rich in whole foods, lean proteins, and healthy fats can improve insulin sensitivity, reduce inflammation, and regulate menstrual cycles. These positive effects highlight the crucial link between diet and PCOS management.
Specific Dietary Recommendations for PCOS Patients
Specific dietary recommendations for PCOS patients often focus on balancing blood sugar levels and reducing inflammation. This often involves prioritizing complex carbohydrates over simple sugars, lean proteins over processed meats, and healthy fats over saturated or trans fats. For example, choosing whole grains over white bread and incorporating foods rich in omega-3 fatty acids (like salmon and flaxseeds) can be beneficial.
How Surgery Can Alter Nutrient Needs
Weight loss surgery can significantly alter nutrient absorption and metabolism. The reduced stomach size or changes in intestinal function can affect how the body absorbs nutrients. This necessitates careful monitoring of nutrient intake and supplementation after surgery. Patients may require additional vitamins, minerals, and other nutrients to compensate for any deficiencies.
Comparison of Pre- and Post-Surgery Dietary Guidelines for PCOS
| Dietary Aspect | Pre-Surgery | Post-Surgery |
|---|---|---|
| Carbohydrates | Focus on complex carbohydrates, limiting refined sugars. | Careful monitoring of carbohydrate intake, often needing smaller portions and adjustments in type. |
| Protein | Include lean protein sources in meals. | Increased protein intake may be necessary to support healing and tissue repair. |
| Fats | Prioritize healthy fats like avocados and nuts. | Monitoring fat intake to ensure adequate absorption and prevent deficiencies. |
| Fiber | High fiber intake is essential for blood sugar control. | Fiber intake needs to be carefully managed due to potential digestive changes. |
| Vitamins & Minerals | Focus on a balanced diet to obtain essential vitamins and minerals. | Potential need for supplementation to address any deficiencies resulting from altered absorption. |
Impact on Fertility and Pregnancy
Weight loss surgery can significantly impact fertility and pregnancy outcomes for individuals with PCOS. The improvements in metabolic health and hormonal balance often lead to positive changes in reproductive function. Understanding these potential effects is crucial for PCOS patients considering this procedure.
Effect of Weight Loss Surgery on Fertility for PCOS Patients
Weight loss surgery, particularly bariatric procedures, can lead to improvements in insulin resistance, which is a common feature of PCOS. This improvement can normalize ovulation cycles, making conception more likely. For example, studies have shown that significant weight loss following bariatric surgery can restore regular menstrual cycles and improve egg quality in women with PCOS. Furthermore, a decrease in androgens (male hormones) is often observed, which can further contribute to improved fertility.
How Weight Loss Can Improve Chances of Conception
Weight loss itself plays a crucial role in enhancing the chances of conception for PCOS patients. Excess weight and associated metabolic issues can disrupt ovulation and make it difficult to conceive. By reducing weight through surgery, individuals with PCOS can improve their metabolic health, regulate their hormonal balance, and increase the likelihood of regular ovulation. This often results in improved egg quality and a more favorable environment for fertilization and implantation.
Importance of Managing PCOS Symptoms During Pregnancy
Managing PCOS symptoms during pregnancy is vital for both the mother’s and the baby’s health. The presence of elevated androgens, insulin resistance, and other PCOS-related factors can increase the risk of gestational diabetes, preeclampsia, and other pregnancy complications. Maintaining a healthy lifestyle, including regular exercise, a balanced diet, and monitoring blood sugar levels, is crucial to mitigate these risks.
Potential Challenges and Considerations for Pregnancy After Surgery
Pregnancy after weight loss surgery can present some challenges. The rapid change in body composition can sometimes affect nutrient absorption, necessitating careful dietary planning and potentially the use of nutritional supplements. Women should consult with their healthcare providers to develop a personalized plan that addresses these potential complications. Furthermore, the long-term effects of the surgery on the body need to be considered and managed during pregnancy.
Insights into Long-Term Fertility After Weight Loss Surgery
The long-term fertility outcomes after weight loss surgery for PCOS patients are generally positive. Normalization of hormonal imbalances and improvement in metabolic health contribute to a higher likelihood of sustained fertility. However, individual experiences may vary, and ongoing monitoring and management of PCOS symptoms are essential. It is important to note that while weight loss surgery can be a beneficial treatment for fertility, it is not a guarantee of conception or long-term fertility.
Understanding the risks and benefits of weight loss surgery for PCOS is crucial. Factors like potential complications and the impact on overall health, including blood flow through the heart, need careful consideration. Blood flow through the heart is vital for the entire body, and any surgical procedure can affect this delicate system. Ultimately, thorough research and consultation with medical professionals are key when exploring this option for PCOS management.
Summary Table: Impact on Pregnancy and Fertility
| Factor | Impact | Considerations |
|---|---|---|
| Weight Loss | Improved ovulation, increased likelihood of conception, better metabolic health | Careful dietary planning, potential nutrient deficiencies, ongoing monitoring |
| Hormonal Balance | Normalization of hormonal imbalances, reduced androgens | Potential for gestational diabetes, preeclampsia, careful monitoring during pregnancy |
| Metabolic Health | Reduced insulin resistance, improved glucose regulation | Potential for changes in nutrient absorption, personalized dietary plans |
| Long-Term Fertility | Generally positive, sustained fertility potential | Individual experiences may vary, ongoing monitoring of PCOS symptoms |
Alternatives to Weight Loss Surgery: Weight Loss Surgery For Pcos Risks And Info
Weight loss surgery is a significant decision, and understanding alternative approaches to managing PCOS-related weight gain and symptoms is crucial. Many individuals can achieve positive outcomes through lifestyle modifications and medical treatments, potentially avoiding the more invasive nature of surgical procedures. These alternatives often offer a more gradual and holistic approach to managing weight and overall health.These alternative methods often prove effective in the long run by addressing the root causes of PCOS-related weight gain and improving overall well-being.
They may also be more suitable for individuals with specific health concerns or preferences. Furthermore, lifestyle changes and medical treatments can complement or even precede surgical interventions, improving patient outcomes.
Lifestyle Changes for PCOS Management
Lifestyle modifications play a pivotal role in managing PCOS symptoms and promoting weight loss. Consistent dietary changes and regular physical activity are fundamental to achieving and maintaining a healthy weight. Adopting a balanced diet that includes plenty of fruits, vegetables, lean proteins, and whole grains, while limiting processed foods, sugary drinks, and excessive saturated fats, can lead to significant improvements.Regular physical activity, including both aerobic exercise and strength training, is essential for burning calories, boosting metabolism, and improving overall health.
This should be tailored to individual needs and preferences.Examples of effective lifestyle changes include:
- Dietary Modifications: A balanced diet focused on whole foods, lean proteins, and fruits and vegetables is key. Reducing refined carbohydrates and sugary drinks is crucial. Portion control is also vital to managing calorie intake. Examples of dietary modifications include swapping sugary cereals for oatmeal, replacing processed snacks with fruits, and opting for lean meats over fatty cuts.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity per week, such as brisk walking, swimming, or cycling. Incorporating strength training exercises two or three times a week is also beneficial. Examples include squats, lunges, push-ups, and rows. The key is consistency and choosing activities you enjoy.
- Stress Management: Chronic stress can exacerbate PCOS symptoms. Practicing stress-reducing techniques like yoga, meditation, or deep breathing exercises can help manage stress levels. Examples include mindfulness exercises, deep relaxation techniques, and practicing yoga.
Medical Treatments for PCOS Management, Weight loss surgery for pcos risks and info
Medical treatments can be used in conjunction with lifestyle changes to help manage PCOS symptoms and promote weight loss. Different medication options target various aspects of PCOS, including hormonal imbalances and insulin resistance. These treatments can help to improve metabolic health and potentially facilitate weight loss.
- Metformin: This medication is commonly prescribed to improve insulin sensitivity, which can help regulate blood sugar levels and potentially lead to weight loss. Its effectiveness in PCOS management has been well-documented in numerous studies.
- Hormonal Contraceptives: These medications can help regulate menstrual cycles and reduce the symptoms associated with hormonal imbalances, which may, in turn, impact weight management. However, their effectiveness in promoting weight loss is less pronounced compared to lifestyle changes and metformin.
- Anti-androgen Medications: These medications are used to address symptoms like acne and excessive hair growth, which can be associated with PCOS. While they don’t directly target weight loss, they can improve overall well-being and potentially indirectly contribute to a healthier lifestyle.
Effectiveness Comparison: Lifestyle vs. Surgery
| Method | Benefits | Drawbacks |
|---|---|---|
| Lifestyle Changes | Improved overall health, manageable cost, reversible, less invasive, and potentially effective long-term. | Requires dedication, may take longer to see results, and individual responses vary. |
| Weight Loss Surgery | Significant and rapid weight loss, potential improvement in PCOS symptoms. | Invasive procedure, potential complications, requires long-term commitment to lifestyle changes post-surgery, and carries risks associated with anesthesia and surgery. |
Long-Term Management and Follow-up
Weight loss surgery for PCOS can significantly improve health outcomes, but sustained success hinges on diligent long-term management. This involves more than just the initial surgery; it’s a journey of ongoing care and lifestyle adjustments. The focus shifts from short-term results to building healthy habits that last a lifetime.
Importance of Ongoing Medical Follow-up
Post-operative care isn’t a one-time event. Regular check-ups are crucial for monitoring overall health, addressing any complications, and adjusting treatment plans as needed. This proactive approach allows for early detection and intervention of potential issues, ensuring the best possible long-term results. Early intervention can prevent or mitigate the severity of complications.
Need for Regular Check-ups and Monitoring
Regular check-ups, often including blood tests, are essential to assess nutritional status, blood sugar levels, and overall metabolic health. Monitoring blood pressure, weight, and the progression of PCOS symptoms are equally important. These checks allow for timely adjustments to medications, dietary plans, or exercise regimens to optimize health. A dedicated healthcare team can help customize a monitoring schedule based on individual needs and progress.
Role of Lifestyle Changes in Long-Term Management
Lifestyle changes are paramount in achieving long-term success after weight loss surgery. This includes maintaining a healthy diet, incorporating regular exercise, and practicing stress management techniques. Adherence to a tailored dietary plan is critical for maintaining weight loss and preventing nutrient deficiencies. Exercise, while potentially challenging after surgery, strengthens the body and enhances overall well-being. Stress management techniques, such as meditation or yoga, can help manage potential emotional challenges and promote a positive outlook.
Examples of Long-Term Support Groups or Resources
Support groups and resources play a vital role in long-term success. These groups offer emotional support, practical advice, and a sense of community among individuals facing similar challenges. Online forums, support groups led by healthcare professionals, and dedicated weight loss surgery centers can provide a network of encouragement and shared experiences. They can provide advice on managing the emotional and physical challenges of long-term recovery.
Importance of Adherence to Post-Operative Recommendations
Adherence to post-operative recommendations is critical for optimal outcomes. This includes diligently following dietary restrictions, attending all scheduled appointments, and taking prescribed medications as directed. Strict adherence is crucial for avoiding complications and maximizing the benefits of the surgery. Open communication with healthcare providers is vital for navigating any challenges or questions that may arise.
Key Elements of Long-Term Management
| Element | Description | Importance |
|---|---|---|
| Regular Check-ups | Scheduled visits with healthcare providers for monitoring health status, including blood work and physical assessments. | Early detection of potential complications and adjustments to treatment plans. |
| Healthy Diet | Following a balanced, nutrient-rich diet tailored to individual needs and post-surgical restrictions. | Maintaining weight loss, preventing nutritional deficiencies, and improving overall health. |
| Regular Exercise | Engaging in regular physical activity, gradually increasing intensity and duration as tolerated. | Strengthening the body, improving metabolic health, and enhancing overall well-being. |
| Stress Management | Utilizing techniques such as meditation, yoga, or counseling to manage stress and promote emotional well-being. | Preventing emotional challenges, improving adherence to treatment plans, and supporting long-term success. |
| Support System | Seeking support from family, friends, support groups, or healthcare professionals. | Providing emotional encouragement, practical advice, and a sense of community. |
Epilogue
In conclusion, while weight loss surgery can offer significant improvements for PCOS, it’s crucial to weigh the potential risks and benefits carefully. Understanding the complexities of PCOS, the various surgical options, and the associated risks, alongside pre- and post-operative considerations, is paramount. This comprehensive guide aims to provide a clear picture of the potential outcomes, highlighting the importance of open communication with medical professionals and the potential need for alternative management strategies.
Ultimately, the decision to undergo surgery should be made in consultation with a healthcare provider, considering individual needs and circumstances.









