What is trigeminal neuralgia? This debilitating condition causes excruciating facial pain, often described as electric shocks or stabbing sensations. Understanding its complexities, from the anatomy of the trigeminal nerve to potential treatments, is key to navigating this challenging health issue.
This comprehensive guide explores the various aspects of trigeminal neuralgia, including its definition, causes, diagnosis, treatment options, management strategies, and potential complications. We’ll also examine illustrative cases and resources for support.
Definition and Overview
Trigeminal neuralgia, often called tic douloureux, is a chronic neurological disorder characterized by sudden, excruciatingly painful episodes in the face. These attacks can range from brief to prolonged, and the pain is typically sharp, stabbing, or electric-like. Understanding the anatomy of the trigeminal nerve and its associated triggers is crucial for comprehending this debilitating condition.This condition affects the trigeminal nerve, a crucial cranial nerve responsible for sensation in the face, and motor functions of the muscles of mastication.
A deep understanding of its various branches and their specific locations within the face is vital for accurate diagnosis and treatment.
Anatomy of the Trigeminal Nerve
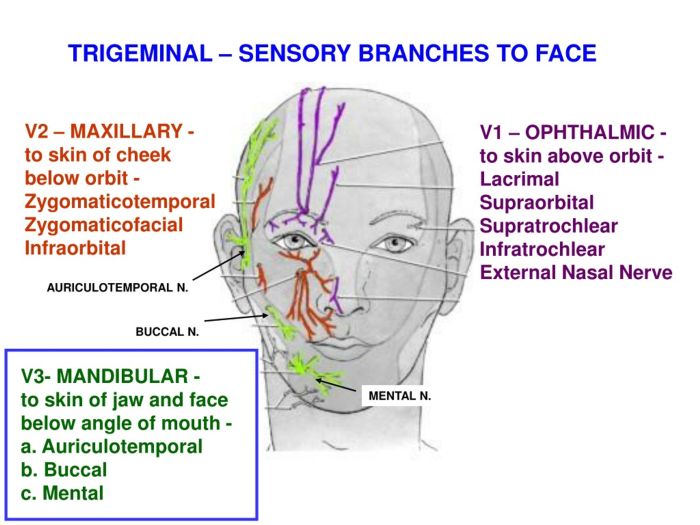
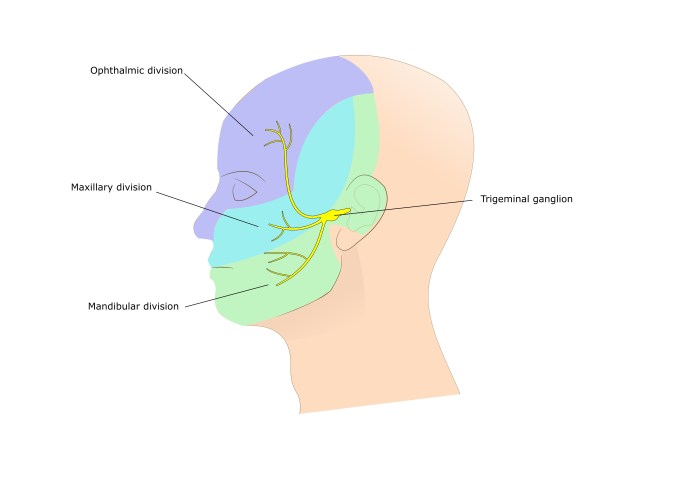
The trigeminal nerve (CN V) is a complex nerve with three major branches: the ophthalmic (V1), maxillary (V2), and mandibular (V3) divisions. These branches supply sensory information to different areas of the face, including the forehead, cheek, jaw, and gums. The ophthalmic nerve (V1) carries sensory information from the upper face, the maxillary nerve (V2) from the mid-face, and the mandibular nerve (V3) from the lower face.
Motor fibers of the mandibular branch control the muscles of mastication. Precise localization of pain within these areas can help determine which branch of the nerve is involved.
Types of Trigeminal Neuralgia
While there isn’t a strict categorization of types based on anatomical differences, clinicians often differentiate trigeminal neuralgia based on its cause. Some cases are idiopathic (of unknown cause), while others might be linked to vascular compression. In these cases, blood vessels, particularly arteries and veins, can press on the trigeminal nerve, leading to the characteristic pain.
Symptoms of Trigeminal Neuralgia
The hallmark symptom of trigeminal neuralgia is sudden, severe pain. Attacks are often triggered by stimulation of the affected areas, such as chewing, talking, or even a light touch. The pain is typically described as sharp, shooting, or electric, and it’s often unilateral, meaning it affects only one side of the face. The pain can be extremely intense, making everyday activities difficult to perform.
Patients might report brief, intense episodes, lasting seconds or minutes, or more prolonged attacks.
Triggers for Trigeminal Neuralgia Attacks
Numerous factors can act as triggers for trigeminal neuralgia attacks. These include:
- Facial movement: Activities like chewing, brushing teeth, talking, or even a slight touch can stimulate the nerve and initiate a painful episode.
- Environmental stimuli: Exposure to cold air or drafts, touching the face, or certain types of food can sometimes trigger an attack.
- Stress and emotional factors: Stress and anxiety have been noted by some patients as potential triggers, although the precise mechanisms are not fully understood. For example, one patient might find that stress leads to a greater frequency or severity of pain attacks.
- Mastication: The act of chewing can be a significant trigger for pain attacks, leading to significant discomfort and affecting daily routines. For example, eating certain foods, or even the act of chewing gum, can be a major trigger.
Causes and Risk Factors
Trigeminal neuralgia, that agonizing facial pain, isn’t always straightforward. While the exact cause remains elusive in many cases, several factors are believed to play a role in its development. Understanding these potential triggers can help in diagnosis and management strategies. Pinpointing the underlying cause can also be crucial for developing personalized treatment plans.The pain of trigeminal neuralgia is often intense and debilitating, impacting daily life significantly.
Research suggests that various factors, both vascular and neurological, can contribute to the development of this condition. This exploration delves into these factors to provide a clearer picture of the complexities behind this neurological disorder.
Potential Underlying Causes
Several factors can contribute to the development of trigeminal neuralgia. While a definitive cause isn’t always identified, research suggests that a combination of factors might be involved. This complexity underscores the need for a multifaceted approach to diagnosis and treatment.
Vascular Compression
A frequent culprit in trigeminal neuralgia is vascular compression. Blood vessels, particularly arteries and veins, can press against the trigeminal nerve, leading to irritation and pain. This compression disrupts the normal function of the nerve, causing the characteristic episodes of intense pain. This phenomenon is often observed in cases where blood vessels are abnormally positioned near the nerve.
For instance, a tortuous (winding) artery might press against the nerve, leading to pain. Similarly, a nearby aneurysm (a bulge in a blood vessel) could also contribute to the compression.
Trigeminal neuralgia is a debilitating facial pain condition, often described as excruciating. While the exact causes are still being researched, it’s a condition that can significantly impact daily life. Interestingly, there’s a complex interplay between various health factors, and exploring conditions like hepatitis D can offer valuable insights into the broader neurological landscape. For a comprehensive overview of hepatitis D, including its causes, symptoms, and treatments, check out this helpful resource: hepatitis d overview and more.
Ultimately, understanding trigeminal neuralgia requires a deep dive into the intricacies of the nervous system.
Neurological Factors
Beyond vascular compression, other neurological factors can also contribute to trigeminal neuralgia. These factors include:
- Degeneration of the trigeminal nerve: Over time, the trigeminal nerve, responsible for sensation in the face, may undergo degeneration, leading to pain. This degeneration can be a consequence of various underlying conditions, such as multiple sclerosis. This condition is characterized by the deterioration of the myelin sheath, the protective covering around nerve fibers, leading to nerve damage and, in some cases, trigeminal neuralgia.
- Other neurological conditions: Certain neurological conditions, including multiple sclerosis (MS), can increase the risk of developing trigeminal neuralgia. MS is an autoimmune disease that affects the central nervous system, potentially leading to nerve damage and pain syndromes. The exact mechanisms connecting these conditions to trigeminal neuralgia are still under investigation, but the link is strong enough to warrant attention in cases of suspicion.
Trigeminal neuralgia, a notoriously painful condition, involves intense, sudden jolts of facial pain. While the sharp, shooting sensations are often debilitating, it’s interesting to consider the neurological quirks of other conditions like exploding head syndrome, a phenomenon where people experience a sound or sensation of an explosion in their head, even though there’s no actual explosion. Learning more about conditions like what is exploding head syndrome helps us understand the vast spectrum of neurological experiences.
Ultimately, understanding trigeminal neuralgia requires delving into the intricacies of the nervous system and the precise pathways involved in pain perception.
- Idiopathic trigeminal neuralgia: In some cases, no specific cause can be identified. This form, referred to as idiopathic trigeminal neuralgia, highlights the complexities of this disorder. In such instances, the focus shifts towards targeted symptom management.
Risk Factors
Certain factors may increase the likelihood of developing trigeminal neuralgia. While not definitive causes, they contribute to the risk profile.
- Age: The prevalence of trigeminal neuralgia tends to increase with age. While this correlation is not fully understood, it suggests a potential role for age-related changes in the nervous system.
- Gender: Women seem to be slightly more prone to trigeminal neuralgia than men. However, this difference isn’t consistently observed in all studies.
- Medical conditions: Individuals with certain medical conditions, such as multiple sclerosis, might be at a higher risk of developing trigeminal neuralgia.
Comparison of Causes
The diverse potential causes of trigeminal neuralgia highlight the need for a comprehensive evaluation. Vascular compression, often related to blood vessel abnormalities, is a common factor. However, other neurological factors, such as nerve degeneration or other neurological conditions, can also contribute. Idiopathic cases, where no clear cause is identified, emphasize the complexity of this disorder.
Diagnosis and Evaluation
Pinpointing the cause of trigeminal neuralgia, a condition marked by excruciating facial pain, hinges on a meticulous diagnostic process. A thorough evaluation of symptoms, combined with a comprehensive neurological examination, plays a crucial role in distinguishing trigeminal neuralgia from other conditions that may mimic its symptoms. Accurate diagnosis is vital for determining the most suitable treatment approach, ensuring optimal pain relief and quality of life for the patient.
Diagnostic Process
The diagnostic process for trigeminal neuralgia typically begins with a detailed patient history. This involves carefully documenting the location, frequency, intensity, and duration of the pain episodes. Understanding triggers, such as chewing, talking, or even light touch, can be invaluable in narrowing down the potential causes. A comprehensive patient history is a crucial first step in determining the possible underlying causes of the pain.
Evaluating Patient Symptoms
Evaluating the patient’s symptoms is a crucial step in the diagnostic process. This involves assessing the characteristics of the pain, such as its quality (e.g., sharp, stabbing, burning), intensity (e.g., mild, moderate, severe), and location. Furthermore, noting the specific circumstances that trigger the pain, such as specific movements or stimuli, can significantly assist in the diagnostic evaluation. Recording the patient’s pain experience in a detailed manner will aid in pinpointing the exact nature of the pain and its triggers.
Potential Diagnostic Tests
Several diagnostic tests might be employed to rule out other conditions. These tests can be helpful in confirming the presence of trigeminal neuralgia or determining if there are any other underlying conditions contributing to the pain. Imaging studies, such as magnetic resonance imaging (MRI) of the brain and/or the cranium, are often utilized to look for structural abnormalities that might be compressing the trigeminal nerve.
Electrodiagnostic studies, such as electromyography (EMG), can help determine if there are any nerve abnormalities. Neurological assessments and medical history analysis are critical in confirming a diagnosis and ruling out other potential causes.
Thorough Neurological Examination, What is trigeminal neuralgia
A thorough neurological examination is paramount in the diagnostic process. This examination focuses on assessing the function of the trigeminal nerve, including its sensory and motor components. Assessing the patient’s facial sensation, strength, and reflexes can help distinguish trigeminal neuralgia from other neurological conditions. Specific testing for facial sensations, including light touch, temperature, and pain, will help to establish the specific location of the pain and its potential triggers.
Steps in Confirming the Diagnosis
Confirming the diagnosis of trigeminal neuralgia involves a multi-faceted approach. Firstly, a comprehensive patient history, including a detailed account of the pain’s characteristics and triggers, is gathered. Secondly, a thorough neurological examination is conducted to assess the function of the trigeminal nerve. Finally, imaging studies, such as MRI, might be employed to identify any structural abnormalities that could be compressing the nerve.
This comprehensive process helps to accurately identify the cause of the pain and differentiate it from other conditions.
Treatment Options
Trigeminal neuralgia, characterized by excruciating facial pain, demands targeted treatment strategies. Effective management aims to reduce pain frequency and intensity, improving quality of life for those affected. A multi-faceted approach, often combining medication with potential surgical interventions, is frequently necessary.
Medication Approaches
Medications play a crucial role in managing trigeminal neuralgia. Several types of drugs are employed, each with varying degrees of effectiveness and potential side effects. Careful consideration of individual patient responses and potential interactions is paramount.
- Anticonvulsants: These medications, such as carbamazepine and oxcarbazepine, are frequently prescribed as first-line treatments. They work by stabilizing nerve impulses, thereby reducing the frequency and severity of pain episodes. For example, carbamazepine is known to effectively control pain in a substantial portion of patients with trigeminal neuralgia, although individual responses vary.
- Antidepressants: Certain antidepressants, like amitriptyline and nortriptyline, can also be beneficial in managing trigeminal neuralgia pain. These medications can impact the way the brain processes pain signals. While often used in combination with anticonvulsants, their effectiveness can be variable, and side effects like drowsiness and weight gain should be considered.
- Other Medications: Other medications, including gabapentin and pregabalin, may be considered if anticonvulsants or antidepressants are insufficient or poorly tolerated. Their mechanisms of action differ, offering alternative avenues for pain relief.
Surgical Interventions
Surgical interventions are considered for patients who do not adequately respond to medication or experience significant side effects. These procedures aim to alleviate pain by either altering the nerve pathways or physically separating the nerve from the blood vessel causing irritation.
- Microvascular Decompression (MVD): MVD is a highly specialized surgical procedure. A small craniotomy (opening in the skull) is performed, and the surgeon meticulously identifies the compressed trigeminal nerve root. A small piece of material, typically Teflon or a similar substance, is placed between the nerve and the blood vessel to relieve the pressure. This procedure is considered highly effective in many cases, offering long-term pain relief for a significant percentage of patients.
Minimally Invasive Procedures
These procedures are alternative approaches for patients who may not be suitable candidates for or wish to avoid open craniotomy. They offer a less invasive path to addressing trigeminal neuralgia.
- Radiofrequency Ablation: This procedure involves using heat to destroy or reduce the activity of the affected nerve branches. It’s a less invasive alternative to surgery, often performed with local anesthesia. However, its effectiveness can be limited and may not provide the long-term pain relief seen with MVD.
Comparing Medication Effectiveness
The effectiveness of various medications in treating trigeminal neuralgia varies significantly among individuals. While anticonvulsants like carbamazepine often prove effective as a first-line treatment, antidepressants may be helpful adjuncts or in cases where anticonvulsants are not well-tolerated. Individual responses to medication should be closely monitored, and adjustments to the treatment plan made as needed.
Management and Self-Care
Living with trigeminal neuralgia can be challenging, but proactive management strategies can significantly improve your quality of life. This section delves into practical techniques for controlling pain attacks, mitigating triggers, and fostering a supportive lifestyle. Understanding your triggers and developing coping mechanisms are crucial for long-term well-being.Effective management involves a multifaceted approach, combining medication, lifestyle adjustments, and self-care techniques.
Consistent adherence to these strategies can lead to a substantial reduction in the frequency and intensity of pain episodes.
Managing Trigeminal Neuralgia Attacks
Recognizing the pattern of your attacks is a vital first step. Note the specific stimuli that typically precede an attack, such as touching your face, eating, or even a sudden change in temperature. This awareness allows you to proactively mitigate potential triggers.
Coping Mechanisms for Pain Relief
Developing coping mechanisms is essential to manage pain during an attack. Techniques like deep breathing exercises, progressive muscle relaxation, or mindfulness meditation can help calm the body and mind, reducing pain perception. Applying a cold compress to the affected area may also provide temporary relief. A warm compress can be beneficial in other situations, but this should be discussed with your physician to ensure it aligns with your specific condition.
Preventing Triggers and Reducing Attack Frequency
Identifying and avoiding triggers is paramount in preventing trigeminal neuralgia attacks. This may involve dietary adjustments, such as avoiding extremely hot or cold foods, or modifications to your daily routine to minimize facial contact with potentially irritating stimuli. For instance, gentle facial massage or particular skincare routines might be triggers. Consulting your healthcare professional is vital for personalized guidance on identifying and minimizing triggers.
Lifestyle Adjustments to Help
Implementing lifestyle adjustments can be a significant part of managing trigeminal neuralgia. A balanced diet rich in essential nutrients can support overall well-being and potentially reduce inflammation. Adequate hydration is also crucial. Maintaining a regular sleep schedule and managing stress through relaxation techniques are equally important components of a supportive lifestyle.
Importance of Regular Follow-up Appointments
Regular follow-up appointments with your healthcare provider are essential. This allows for ongoing monitoring of your condition, adjustment of treatment plans as needed, and early detection of any potential complications. Your doctor can provide personalized guidance and support throughout your trigeminal neuralgia journey.
Illustrative Cases of Trigeminal Neuralgia
Understanding the diverse presentations of trigeminal neuralgia (TN) is crucial for effective diagnosis and treatment. While the hallmark symptom is excruciating pain, the location, intensity, and triggers can vary significantly from person to person. These variations highlight the importance of a personalized approach to care.
Patient Profiles and Treatment Approaches
Trigeminal neuralgia (TN) is a debilitating condition characterized by sudden, intense, stabbing pain affecting one or more branches of the trigeminal nerve. The pain often arises in response to seemingly innocuous stimuli, such as brushing teeth, chewing, or even light touch. Examining real-world cases illustrates the complexity and variability of this neurological disorder.
| Patient Profile | Symptoms | Treatment |
|---|---|---|
| Patient 1: A 68-year-old female | Experiences sharp, shooting pain, often described as electric shocks, on the right side of her forehead and cheek. The pain is triggered by light touch, brushing her teeth, or even a draft. The intensity is severe, with pain lasting for seconds to minutes, and recurring multiple times a day. | Prescribed carbamazepine, a medication commonly used to manage TN. The medication was initially effective in reducing the frequency and severity of attacks. However, after several months, the patient experienced side effects and required a dosage adjustment. Eventually, the patient opted for a surgical intervention to alleviate the most intense pain. |
| Patient 2: A 45-year-old male | Reports intermittent, severe, lancinating pain localized to the lower jaw on the left side. The pain is triggered by eating, talking, and even a slight pressure on the jaw. The intensity is debilitating, causing significant interference with daily activities. The attacks are less frequent compared to Patient 1, but are equally intense. | Initial treatment involved carbamazepine, which provided partial relief but did not eliminate the pain entirely. The patient was subsequently referred to a neurologist for a possible surgical intervention. A microvascular decompression (MVD) surgery was performed to relieve pressure on the trigeminal nerve, successfully reducing the pain frequency and intensity. |
| Patient 3: A 32-year-old female | Describes a constant, dull ache in the left side of her jaw and temple area, accompanied by episodes of sudden, severe stabbing pain. The pain is exacerbated by talking, yawning, and chewing. The intensity of the stabbing pain is less severe than in Patient 1 but is constant and disruptive. | Initially, gabapentin was prescribed. This medication was effective in managing the constant ache, reducing the overall discomfort, but did not entirely eliminate the sudden stabbing pain. Due to the partial response, a combination therapy of gabapentin and low-dose amitriptyline was considered to address the combined pain symptoms. The treatment plan is continually monitored and adjusted based on the patient’s response. |
Potential Complications
Trigeminal neuralgia, while often manageable, can have significant impacts on a patient’s well-being beyond the immediate pain. Understanding potential complications is crucial for effective management and ensuring the best possible quality of life. This section delves into the possible consequences of the condition itself, its treatments, and how these factors influence daily life.The multifaceted nature of trigeminal neuralgia, characterized by unpredictable and severe pain attacks, can lead to a range of physical and psychological complications.
Furthermore, the treatment strategies employed can also have potential side effects that need careful consideration.
Impact on Daily Activities
The relentless pain associated with trigeminal neuralgia can significantly disrupt daily routines. Patients often experience difficulties with eating, speaking, and even simple facial movements due to the intense pain. This can lead to social isolation and reduced participation in activities previously enjoyed. For instance, the fear of triggering a pain attack can limit outings, social interactions, and even household chores.
Trigeminal neuralgia, a debilitating facial pain condition, is often described as a sudden, intense, electric shock-like sensation. While the exact causes of this nerve pain aren’t fully understood, it’s important to be aware of potential triggers, including conditions like anaphylaxis. Understanding the risk factors for anaphylaxis, such as specific allergies and medications, anaphylaxis causes risk factors , can help us appreciate the multifaceted nature of health issues.
Ultimately, understanding the complexities of trigeminal neuralgia requires a nuanced approach to both the immediate symptoms and the potential underlying triggers.
Impact on Quality of Life
The chronic pain and potential limitations imposed by trigeminal neuralgia can drastically reduce quality of life. The constant fear of an attack, the need for frequent medical appointments, and the potential for side effects of treatment can contribute to stress, anxiety, and depression. Patients may experience decreased enjoyment of life, diminished social engagement, and feelings of helplessness. Furthermore, the unpredictable nature of the condition can lead to significant financial strain due to lost productivity and increased healthcare costs.
Potential Complications of Treatment
Various treatment options exist for trigeminal neuralgia, each with its own potential side effects. Surgical interventions, for example, carry risks of facial nerve damage, numbness, or altered sensation in the affected area. Medications, while effective for pain management, may have side effects such as drowsiness, dizziness, or gastrointestinal issues.
Comparison of Risks Across Treatment Options
A thorough evaluation of the potential benefits and risks of each treatment option is essential for each patient. Factors like the severity of the condition, the patient’s overall health, and personal preferences should all be considered. For example, while surgical interventions can offer long-term pain relief for some patients, they come with a higher risk of complications compared to medication.
It is crucial to discuss these risks and benefits with a healthcare professional to make an informed decision.
Preventive Measures
While a complete prevention of trigeminal neuralgia attacks may not be possible, various strategies can help minimize the risk of complications. These strategies encompass lifestyle modifications, adherence to treatment plans, and regular follow-up appointments.
- Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques, can contribute to overall well-being and potentially reduce the frequency and severity of attacks.
- Adhering strictly to the prescribed treatment plan, including medication schedules and lifestyle adjustments, is crucial for managing the condition effectively and minimizing potential complications.
- Regular communication with healthcare providers, including reporting any changes in symptoms or side effects, ensures prompt identification and management of potential complications.
Long-Term Effects
The long-term effects of trigeminal neuralgia can range from physical discomfort to psychological distress. Prolonged pain can lead to muscle tension, headaches, and fatigue. The condition can also affect mental well-being, potentially leading to anxiety and depression. Chronic pain and the limitations it imposes can also impact social interactions and professional life. This impact can vary significantly between individuals depending on the severity of the condition and the effectiveness of treatment.
Resources and Support: What Is Trigeminal Neuralgia
Navigating the complexities of trigeminal neuralgia can be challenging, but you’re not alone. Finding reliable resources and supportive communities can make a significant difference in managing this condition. This section Artikels valuable avenues for help, from connecting with healthcare professionals to joining support groups.
Reliable Resources for Patients
Numerous organizations and websites provide crucial information and support for those living with trigeminal neuralgia. These resources offer a wealth of knowledge, from symptom management to navigating the healthcare system.
- National Institutes of Health (NIH): The NIH’s National Institute of Neurological Disorders and Stroke (NINDS) is a leading source of information on neurological conditions. Their website provides detailed explanations of trigeminal neuralgia, including research updates and clinical trials. Information on related disorders and treatment options is also readily available.
- National Headache Foundation: This organization is dedicated to improving the lives of individuals affected by headaches and other facial pain conditions, including trigeminal neuralgia. They offer educational materials, support groups, and information on the latest research.
- Mayo Clinic: A well-regarded medical institution, the Mayo Clinic provides comprehensive information on trigeminal neuralgia, including diagnosis, treatment options, and potential complications. Their website offers clear and concise explanations, making it easy for patients to understand the condition and available resources.
Support Groups and Organizations
Connecting with others who understand what you’re going through can be incredibly helpful. Support groups provide a safe space to share experiences, offer encouragement, and learn coping strategies from others facing similar challenges.
- Patient advocacy groups: Numerous patient advocacy groups focus on specific neurological conditions. These groups can offer invaluable support and guidance to individuals living with trigeminal neuralgia. They often host online forums, meetings, and events, allowing patients to connect with each other.
- Local chapters of national organizations: Many national organizations have local chapters or support groups that provide face-to-face interaction. These groups can offer a sense of community and provide opportunities to connect with others in your local area who understand your situation. This can lead to invaluable peer-to-peer support.
Relevant Websites and Online Communities
The internet offers a wealth of information and support for those with trigeminal neuralgia. Online communities provide a space to connect with others, share experiences, and ask questions.
- Online forums and support groups: Many online forums and support groups cater to patients with neurological conditions. These platforms can be invaluable for sharing experiences, discussing treatment options, and obtaining advice from others who have been through similar situations. Be sure to choose reputable and well-moderated groups for a supportive and helpful experience.
- Patient-focused websites: Several websites focus on patient advocacy and education. These resources can offer information on the condition, treatment options, and the latest research findings. This information can be vital for informed decision-making.
Finding Qualified Healthcare Professionals
Choosing the right healthcare provider is essential in managing trigeminal neuralgia. Consulting with specialists who understand this condition is crucial.
- Neurologists: Neurologists are medical doctors specializing in the nervous system. They are the primary healthcare providers for individuals with trigeminal neuralgia, as they possess the expertise and knowledge to diagnose, treat, and manage this condition.
- Pain management specialists: Pain management specialists can offer specialized care for trigeminal neuralgia, particularly when managing pain. They can provide effective treatment plans that consider the specific needs of the patient.
Table of Resources
| Resource Type | Contact Information |
|---|---|
| National Institutes of Health (NIH) | https://www.ninds.nih.gov/ |
| National Headache Foundation | https://www.headache.org/ |
| Mayo Clinic | https://www.mayoclinic.org/ |
Closing Notes
In conclusion, trigeminal neuralgia is a complex neurological disorder demanding careful attention and personalized care. By understanding the different aspects of this condition, from its causes and diagnosis to potential treatments and long-term management, patients and their loved ones can navigate this journey with greater awareness and informed decision-making. Remember, support networks and resources are available, and seeking professional medical guidance is crucial.









