Yeast infection on skin is a common skin condition that can affect various parts of the body. This guide dives deep into the world of skin yeast infections, exploring their causes, symptoms, diagnosis, treatment, and prevention strategies. Understanding these aspects is crucial for effective management and a healthier you.
This comprehensive guide covers everything from the different types of skin yeast infections and their unique characteristics to the diagnostic procedures and treatment options. It also delves into preventive measures, highlighting the importance of good hygiene and lifestyle choices.
Introduction to Skin Yeast Infections
Skin yeast infections, also known as dermatophytosis, are common fungal infections of the skin. These infections are caused by various types of yeasts, primarilyCandida albicans*, but also other species. They thrive in warm, moist environments, making certain areas of the body particularly susceptible. Understanding the causes, symptoms, and prevention strategies is crucial for managing and preventing these infections effectively.Skin yeast infections can affect various parts of the body, creating discomfort and sometimes requiring medical intervention.
Common locations include areas with folds of skin, like the groin (jock itch), under the breasts, and between the toes (athlete’s foot). These areas provide a warm, humid environment ideal for yeast growth. Recognizing the symptoms and knowing the common causes can facilitate early intervention and prevent the spread of infection.
Types of Yeast Involved
Skin yeast infections are predominantly caused by the
- Candida* species, particularly
- Candida albicans*. Other
- Candida* species and non-
- Candida* yeasts can also cause infections, although
- Candida albicans* is the most frequent culprit. This highlights the importance of proper identification and treatment, as different types of yeast may respond differently to certain therapies.
Common Locations
Skin yeast infections commonly affect areas with folds of skin where moisture and warmth are retained. These include the groin (causing jock itch), under the breasts, between the toes (athlete’s foot), and under the fingernails or toenails. Other less common locations include the skin folds around the neck, the armpits, and the skin creases on the body.
Symptoms of Skin Yeast Infections
The symptoms of skin yeast infections typically involve redness, itching, and a white or yellowish rash. The rash might appear as a smooth, moist area or be characterized by small, raised bumps. In some cases, the affected skin may be flaky or have a scaly texture. These symptoms can vary depending on the location and severity of the infection.
Common Causes of Skin Yeast Infections
Skin yeast infections often arise due to environmental factors that promote yeast growth. These include prolonged exposure to moisture, such as from sweating or not adequately drying after bathing. Certain lifestyle factors can also contribute, such as wearing tight-fitting clothing, which can trap moisture against the skin. Poor hygiene practices, such as not frequently washing affected areas, also increase the risk of infection.
Prevention and Management Strategies
| Location | Symptoms | Typical Causes | Prevention Tips |
|---|---|---|---|
| Groin (Jock Itch) | Redness, itching, burning, rash | Prolonged moisture, tight clothing, poor hygiene | Keep the area clean and dry, use loose-fitting clothing, and dry thoroughly after bathing. |
| Between Toes (Athlete’s Foot) | Redness, itching, scaling, blisters | Moisture, sharing footwear, poor hygiene | Keep feet dry, use separate footwear, and ensure proper hygiene. |
| Under Breasts | Redness, itching, rash, burning | Moisture, tight clothing, poor hygiene | Wear breathable clothing, avoid tight bras, and ensure proper hygiene. |
| Skin Folds | Redness, itching, rash, cracking | Prolonged moisture, friction, poor hygiene | Keep skin folds dry, avoid tight clothing, and practice good hygiene. |
Types and Variations
Skin yeast infections, also known as dermatophytosis, manifest in various forms, each with unique characteristics. Understanding these differences is crucial for accurate diagnosis and effective treatment. Different fungal species and their interactions with the skin contribute to the distinct presentations of these infections. This section will explore the diverse types of skin yeast infections, their symptoms, and the underlying causes.Different types of skin yeast infections vary significantly in their appearance, location, and symptoms.
These variations stem from the specific fungal species involved, the individual’s immune response, and environmental factors. This diversity necessitates a nuanced approach to diagnosis and treatment.
Candida Infections
Candida infections, often caused by theCandida albicans* fungus, are among the most common types. These infections typically appear as red, itchy patches, often with a slightly raised or bumpy texture. Sometimes, the affected area may be covered in white, cheesy-like patches, especially in the case of oral thrush. The location of the infection can range from the skin folds, such as the groin (jock itch) or under the breasts, to the mouth, nails, or even the vagina.
Treatment usually involves antifungal medications, either topical or oral, depending on the severity and location of the infection. Proper hygiene practices, including maintaining dry and clean skin folds, are essential in preventing recurrence.
Dealing with a yeast infection on the skin can be frustrating. It’s important to look for natural remedies, and one intriguing option is exploring the potential benefits of shilajit. Studies suggest that this natural substance may have antimicrobial properties, potentially aiding in the healing process. Learning more about the benefits of shilajit could provide valuable insights into supporting your body’s natural defenses against yeast infections.
Of course, consulting a healthcare professional remains crucial for proper diagnosis and treatment of skin yeast infections. the benefits of shilajit
Intertrigo
Intertrigo is a type of skin yeast infection that primarily affects skin folds. It arises from moisture and friction in areas like the groin, under the breasts, or between the buttocks. Characterized by redness, maceration (softening of the skin), and often a burning or itching sensation, intertrigo can sometimes develop a secondary bacterial infection. The moisture and warmth in these areas create an ideal environment for yeast growth, highlighting the importance of keeping these areas dry and well-ventilated.
Treatment usually involves antifungal creams and maintaining good hygiene to prevent further moisture buildup.
Tinea Versicolor
Tinea versicolor, also known as pityriasis versicolor, is caused by theMalassezia* yeast. This infection often presents as discolored patches on the skin, ranging from light brown to pink or even white. The patches are typically flat and slightly scaly, and they often occur on the chest, back, or shoulders. The infection doesn’t usually cause significant itching or pain, making it sometimes difficult to detect.
Treatment options include antifungal creams, oral medications, and even topical solutions. Avoiding excessive sweating and maintaining good hygiene can reduce the risk of recurrence.
Table of Skin Yeast Infections
| Type | Key Symptoms | Common Causes |
|---|---|---|
| Candida Infections | Red, itchy patches; raised or bumpy texture; white, cheesy patches; various locations (skin folds, mouth, nails, vagina) | *Candida albicans* fungus; moisture, warmth; poor hygiene |
| Intertrigo | Redness, maceration (softening of skin); burning or itching; skin folds (groin, under breasts, buttocks) | Moisture, friction; yeast growth; warm, humid conditions |
| Tinea Versicolor | Discolored patches (light brown, pink, white); flat, slightly scaly; chest, back, shoulders | *Malassezia* yeast; excessive sweating; warm, humid environments |
Diagnosis and Assessment
Pinpointing the specific cause of skin irritation is crucial for effective treatment. A proper diagnosis often involves a combination of physical examination, patient history, and potentially, further tests. Understanding the diagnostic process helps patients and healthcare professionals work together to identify the root cause and choose the most appropriate course of action.
Physical Examination
A thorough physical examination is fundamental in diagnosing skin yeast infections. A healthcare professional will carefully inspect the affected area, noting the location, appearance, and extent of the rash. This visual assessment provides valuable clues about the nature of the infection. Features like redness, scaling, itching, or the presence of characteristic lesions are carefully documented. The practitioner will also look for any signs of secondary bacterial infections, which often accompany or follow skin yeast infections.
Patient History
Gathering a detailed patient history plays a significant role in the diagnostic process. Information about the onset, duration, and progression of symptoms, including the presence of any other symptoms or predisposing factors, is essential. A history of recent antibiotic use, recent changes in hygiene practices, or known allergies can provide crucial insights into the potential causes. This information, combined with the physical examination, assists in differentiating skin yeast infections from other skin conditions.
Medical Professional’s Role
A qualified healthcare professional, such as a dermatologist or primary care physician, plays a vital role in confirming a diagnosis and guiding treatment. They possess the expertise to differentiate between various skin conditions, considering the patient’s specific symptoms and medical history. Their professional judgment is critical in ruling out other possible causes, and their experience in interpreting clinical findings is invaluable in arriving at an accurate diagnosis.
They will often perform a physical examination and consider a patient’s medical history before recommending additional tests.
Diagnostic Tools and Procedures
Proper identification of skin yeast infections often relies on a combination of approaches. This section Artikels the common diagnostic tools and procedures.
| Diagnostic Tool | Procedure Details |
|---|---|
| Visual Inspection | Careful observation of the affected area, noting characteristics like redness, scaling, itching, and the presence of characteristic lesions. This initial assessment is crucial for determining the potential presence of a skin infection. |
| KOH Preparation | A potassium hydroxide (KOH) preparation is a microscopic examination technique used to identify fungal elements. A skin sample is prepared and examined under a microscope to look for hyphae (filaments) or yeast cells, which are characteristic of fungal infections. This is a relatively simple and inexpensive test. |
| Culture | A skin sample can be cultured to isolate and identify the specific type of fungus causing the infection. This can help in tailoring treatment strategies to target the particular fungal species. This test takes longer than the KOH preparation. |
| Wood’s Lamp Examination | A Wood’s lamp is a device that uses ultraviolet light to visualize certain skin conditions. While not exclusively for yeast infections, it can sometimes help identify characteristic fluorescence patterns associated with certain types of fungal infections. |
Treatment and Management: Yeast Infection On Skin
Treating skin yeast infections effectively involves addressing the underlying cause and managing the symptoms. A multifaceted approach often proves most successful, encompassing topical medications, lifestyle adjustments, and potentially oral antifungal treatments. Understanding the different treatment options and adhering to a prescribed plan are crucial for successful resolution and prevention of recurrence.Effective management of skin yeast infections requires a proactive approach.
This includes recognizing the signs and symptoms early and seeking professional medical advice for accurate diagnosis and tailored treatment. Delayed or inadequate treatment can lead to complications, while self-treatment without professional guidance may be ineffective or even harmful.
Common Treatment Approaches
Various treatment options are available for skin yeast infections, ranging from over-the-counter (OTC) remedies to prescription medications. Choosing the right treatment depends on the severity of the infection, the location of the affected area, and the specific type of yeast involved.
Over-the-Counter Medications
OTC antifungal creams and powders are often the first line of defense for mild to moderate skin yeast infections. These products typically contain ingredients like clotrimazole, miconazole, or nystatin, which work by disrupting the growth of the yeast. Applying these products as directed on the packaging, typically for several days, can help alleviate symptoms. It’s important to note that OTC treatments might not be effective for all cases and may not be sufficient for severe infections.
Dealing with a yeast infection on your skin can be frustrating. It’s important to understand that certain medications, like those containing benzonatate, might interact negatively with other drugs. For example, learning about what drugs should not be taken with benzonatate is crucial if you’re trying to treat a yeast infection and are already on other medications.
Ultimately, consulting a doctor is always the best course of action for proper diagnosis and treatment of skin yeast infections.
Prescription Medications
For more persistent or widespread infections, prescription antifungal medications may be necessary. These can include oral medications, such as fluconazole or itraconazole, or stronger topical creams. Prescription treatments are usually reserved for cases where OTC remedies have failed or when the infection is particularly severe. Doctors may also prescribe these for recurrent or chronic infections.
Importance of Following a Prescribed Treatment Plan
Adhering to the prescribed treatment plan is paramount for effective management. Skipping doses or prematurely stopping treatment can lead to incomplete eradication of the yeast, potentially causing the infection to persist or recur. Following the instructions provided by the healthcare professional, including duration of treatment and application frequency, is essential for successful outcomes.
Potential Complications if Left Untreated
Left untreated, skin yeast infections can become more widespread and potentially lead to secondary skin infections. This can happen when the affected area becomes irritated or damaged, creating an entry point for bacteria. In rare cases, severe infections may cause systemic complications, though this is less common.
Importance of Consulting a Doctor Before Self-Treating
Before self-treating a skin yeast infection, consulting a doctor is crucial. Self-diagnosis and treatment can delay proper care and potentially mask underlying conditions. A healthcare professional can accurately diagnose the infection, determine the appropriate treatment, and monitor the response to therapy. This ensures effective management and prevents potential complications.
Treatment Options Table
| Treatment Option | Description | Potential Side Effects |
|---|---|---|
| OTC Antifungal Creams/Powders (e.g., clotrimazole, miconazole) | Topical application to affected area. Available over-the-counter. | Possible skin irritation, redness, or burning at the application site in some individuals. |
| Prescription Antifungal Creams | Prescription-strength topical medications containing stronger antifungal agents. | Similar potential skin reactions as OTC creams, though may be more pronounced in some cases. |
| Oral Antifungal Medications (e.g., fluconazole, itraconazole) | Taken orally to target systemic yeast infections. | Possible side effects include nausea, vomiting, headache, or liver problems in some patients. |
Prevention and Hygiene
Skin yeast infections, while often manageable, can be recurring if preventative measures aren’t taken. Proactive hygiene and understanding the factors that contribute to infection risk are key to maintaining healthy skin and preventing future outbreaks. This section Artikels strategies to reduce the likelihood of developing these infections.Maintaining healthy skin and practicing good hygiene are crucial for preventing skin yeast infections.
By understanding the conditions that favor yeast growth and implementing the appropriate preventive measures, individuals can significantly reduce their risk.
Maintaining Healthy Skin
Healthy skin acts as a natural barrier against infection. Factors like moisture levels, pH balance, and overall skin health influence the likelihood of yeast overgrowth. Proper skin care routines and lifestyle choices can contribute to a healthier skin barrier.
- Maintaining proper hydration: Adequate hydration keeps skin supple and less prone to cracking, reducing entry points for infection. Drinking enough water and using moisturizers can help maintain optimal skin moisture.
- Maintaining a healthy diet: A balanced diet rich in fruits, vegetables, and whole grains provides the nutrients necessary for healthy skin cell regeneration and overall immune function, which can indirectly help reduce the risk of infection.
- Avoiding excessive sweating: Sweating creates a warm, moist environment that encourages yeast growth. Regular showering and changing into dry clothes after sweating can help minimize this risk. In hot and humid climates, the risk is particularly high, emphasizing the importance of hygiene practices.
- Managing underlying health conditions: Certain medical conditions, such as diabetes, can increase the risk of skin yeast infections. Managing these conditions effectively can help reduce this risk.
Proper Hygiene Practices
Consistent hygiene practices are essential in preventing skin yeast infections. Regular cleaning, especially in areas prone to moisture, is key to minimizing the growth of yeast.
- Regular cleansing: Gentle cleansing with mild soap or a body wash, avoiding harsh chemicals or soaps that can disrupt the skin’s natural pH balance, is important. This helps remove dead skin cells and excess moisture, limiting the environment for yeast growth.
- Thorough drying: After showering or bathing, ensure the affected area is completely dry. This prevents moisture buildup, a crucial factor in yeast proliferation. Using a clean towel is vital, as a damp towel can spread the infection.
- Avoiding tight clothing: Tight clothing traps heat and moisture, creating a breeding ground for yeast. Wearing loose-fitting clothing allows for better airflow and helps keep the skin dry.
- Properly cleaning and drying equipment: Use clean towels, and wash or clean items such as athletic gear, workout clothes, or clothing that frequently come into contact with skin in a timely manner to avoid repeated exposure to moisture.
Personal Protective Equipment (PPE)
In specific situations, PPE can provide an extra layer of protection against skin yeast infections. Examples include occupations involving frequent contact with moisture or environments with high humidity.
Dealing with a yeast infection on skin can be frustrating, and sometimes, seemingly unrelated health factors like blood pressure can play a role. Maintaining healthy systolic and diastolic blood pressure systolic and diastolic blood pressure might indirectly influence your body’s overall response to the infection, impacting its severity and healing time. So, while not a direct cause, keeping a watchful eye on these factors might be beneficial for your skin health journey.
- Using protective clothing: For individuals in occupations involving prolonged exposure to moisture or high humidity, protective clothing, such as waterproof or moisture-wicking materials, can help prevent yeast infection.
- Proper use of gloves: In situations involving contact with potentially contaminated surfaces or substances, wearing gloves can help prevent infection by avoiding direct skin contact.
- Using barriers: Applying barrier creams or ointments can create a physical barrier against yeast and prevent infection. These creams help prevent yeast from adhering to skin.
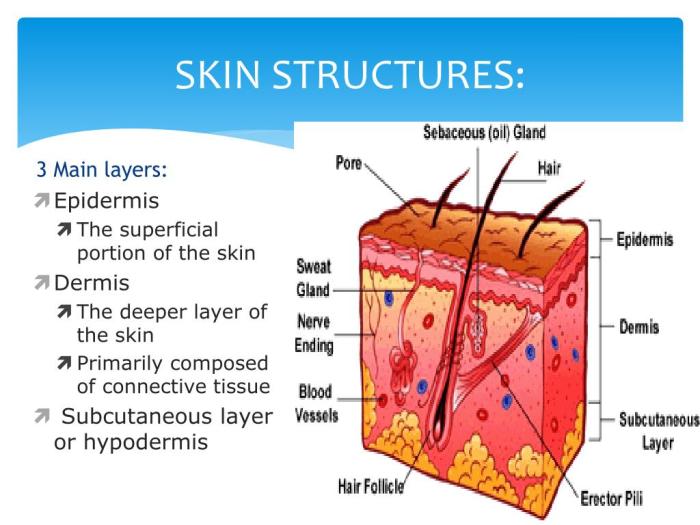
Illustrations and Visual Aids
Visual aids are crucial for understanding complex topics like skin yeast infections. Illustrations help us visualize the intricate mechanisms and appearances of these conditions, making the information more accessible and memorable. They can also be instrumental in aiding diagnosis and treatment planning.
Fungal Structures Causing Skin Yeast Infections
A detailed illustration of the fungal structures responsible for skin yeast infections would show the microscopic morphology of the yeast cells. The image would highlight the characteristic budding yeast cells, which reproduce by forming new cells (budding) from the parent cell. Important features to include are the size and shape of the yeast cells, the presence of any hyphae (filamentous structures), and the cell wall structures, which are crucial in determining the specific type of fungus.
The illustration should also indicate the location of these structures within the skin’s layers, showing where they proliferate and interact with the host’s cells.
Typical Appearance of Different Types of Skin Yeast Infections
Visual representations of various skin yeast infections should clearly demonstrate the diverse presentations. For example, a candidiasis infection, often characterized by redness, may be depicted with images of inflamed skin areas. Other types, like pityriasis versicolor, which causes discolored patches, could be illustrated with images of hypopigmented (lighter) or hyperpigmented (darker) areas on the skin. The illustration should also show the potential for different skin tones to affect the appearance of the infection.
This is crucial for accurate diagnosis and avoiding misdiagnosis, especially in diverse populations.
Progression of a Skin Yeast Infection Over Time, Yeast infection on skin
A graphic depicting the progression of a skin yeast infection would be a series of images, illustrating the evolution from an initial subtle rash to a more pronounced and inflamed state. The first image might show a small, red, slightly raised area, potentially with some scaling. The second image could depict the rash expanding, becoming more inflamed, and perhaps exhibiting some oozing or crusting.
The final image could show the healing stage, where the skin is beginning to return to its normal appearance, although some residual discoloration or scarring might be visible. This visual representation helps patients understand the expected course of the infection and facilitates early intervention.
Body’s Immune Response to a Skin Yeast Infection
A diagram of the body’s immune response to a skin yeast infection should illustrate the complex interaction between the immune cells and the fungal organisms. The diagram would highlight the recruitment of immune cells like neutrophils and macrophages to the infected area. The image should visually demonstrate the process of phagocytosis, where immune cells engulf and destroy the fungal cells.
The diagram could also show the release of inflammatory mediators and cytokines, which are crucial for orchestrating the immune response. This diagram will clearly illustrate the role of the immune system in combating the infection and potentially preventing its spread.
Underlying Conditions and Risk Factors
Skin yeast infections, often frustrating and uncomfortable, aren’t always just a matter of poor hygiene. Various underlying conditions and lifestyle choices can significantly increase a person’s susceptibility to these infections. Understanding these factors can help in proactive prevention and effective management.
Medical Conditions Increasing Risk
Several medical conditions can compromise the body’s natural defenses, making individuals more vulnerable to skin yeast infections. These conditions often affect the immune system’s ability to fight off infections effectively.
- Diabetes Mellitus: High blood sugar levels can create an environment that fosters yeast overgrowth. Uncontrolled diabetes can lead to frequent and persistent yeast infections in various locations on the skin, particularly in moist areas like the groin or under the breasts.
- Weakened Immune System: Conditions like HIV/AIDS, cancer treatments, or autoimmune diseases can significantly impair the immune system’s ability to fight off infections. This can make individuals more susceptible to skin yeast infections, which might appear as persistent or recurrent issues.
- Organ Transplant Recipients: Patients who have undergone organ transplants often take immunosuppressant medications to prevent organ rejection. These medications can suppress the immune system, increasing the risk of skin yeast infections and other infections.
- Certain Medications: Some medications, such as corticosteroids, can also weaken the immune system, making the body more susceptible to yeast infections.
Lifestyle Factors Contributing to Yeast Infections
Certain lifestyle choices can contribute to the creation of an environment favorable for yeast overgrowth, increasing the risk of skin yeast infections.
- Poor Hygiene: Insufficient or improper hygiene practices can allow yeast to thrive in moist areas of the skin. Not adequately cleaning and drying these areas after sweating or bathing can create an ideal environment for yeast growth.
- Frequent Use of Antibiotics: While antibiotics are essential for bacterial infections, their indiscriminate use can disrupt the natural balance of the body’s microbial flora. This disruption can lead to an overgrowth of yeast, increasing the risk of yeast infections.
- Prolonged Moisture: Prolonged exposure to moisture, like from sweating, wearing tight clothing, or having certain medical conditions, can create an environment that favors yeast growth. This is particularly relevant for skin folds and areas that retain moisture.
- Diet and Nutrition: A diet high in sugar and processed foods may potentially contribute to yeast overgrowth, though more research is needed in this area.
Role of Immune System Deficiencies
A compromised immune system plays a crucial role in increasing the susceptibility to skin yeast infections. The immune system’s primary function is to defend the body against pathogens, including yeast. When the immune system is weakened, it is less effective in controlling yeast overgrowth, which can lead to more frequent or severe infections.
- Immunodeficiency Disorders: Individuals with immunodeficiency disorders, such as DiGeorge syndrome, experience a weakened immune system, leading to a higher risk of yeast infections.
- Certain Medical Conditions: Conditions like diabetes, malnutrition, and certain chronic illnesses can negatively impact the immune response, increasing susceptibility to yeast infections.
Medications Affecting Immune Response and Infection Risk
Certain medications can have a significant impact on the immune system, making individuals more susceptible to skin yeast infections. Understanding the effect of medications on immune function is crucial for preventing and managing infections.
- Immunosuppressants: Immunosuppressants, commonly prescribed after organ transplants or for autoimmune conditions, directly suppress the immune system’s ability to fight infections. This significantly increases the risk of skin yeast infections and other infections.
- Corticosteroids: Corticosteroids, frequently used for various inflammatory conditions, can also weaken the immune response, increasing the risk of skin yeast infections.
Final Review

In conclusion, yeast infection on skin, while common, can be effectively managed with proper understanding and care. By recognizing the symptoms, understanding the underlying causes, and adhering to a prescribed treatment plan, individuals can effectively address this skin condition. Prevention plays a crucial role, and maintaining good hygiene and a healthy lifestyle can significantly reduce the risk of infection.
Remember, consulting a medical professional is always recommended for accurate diagnosis and tailored treatment.








