Types of heart disease is a broad and complex topic, encompassing a variety of conditions that affect the heart’s function. Understanding the different types, from coronary artery disease to congenital heart defects, is crucial for effective prevention and treatment. This guide delves into the specifics of each, exploring their causes, symptoms, and available treatment options. We’ll also examine the historical context of heart disease research and the remarkable advancements in treatment methods.
Each type of heart disease has its own unique characteristics, risk factors, and progression. This exploration will help readers gain a deeper understanding of these conditions, empowering them to make informed decisions about their health and well-being.
Introduction to Heart Disease
Heart disease, a broad term encompassing various conditions affecting the heart and blood vessels, remains a leading cause of death globally. It encompasses a spectrum of issues, from coronary artery disease (CAD) and heart valve problems to cardiomyopathies and congenital heart defects. Understanding the different types, risk factors, and preventative measures is crucial for proactive health management.Heart disease arises from a complex interplay of genetic predispositions and lifestyle choices.
Early detection and a focus on preventative measures can significantly reduce the risk of developing severe complications. Historical research into heart disease has yielded invaluable insights into its causes and mechanisms, leading to advancements in diagnostic tools and treatment options. Modern medicine offers a range of effective therapies, including lifestyle modifications, medications, and surgical interventions.
Common Risk Factors
Several factors increase the likelihood of developing heart disease. These factors can be broadly categorized into modifiable and non-modifiable risk factors. Modifiable risk factors, such as smoking, high blood pressure, high cholesterol, and a sedentary lifestyle, can be addressed through lifestyle changes. Non-modifiable risk factors, such as age, family history, and gender, while not directly controllable, highlight the importance of proactive health management and early screening.
- Smoking: Nicotine and other harmful chemicals in tobacco smoke damage blood vessels and increase the risk of blood clots, contributing to heart attacks and strokes. Long-term smokers are significantly more prone to cardiovascular issues.
- High Blood Pressure: Persistent high blood pressure strains the heart and blood vessels, potentially leading to damage and the development of various heart diseases.
- High Cholesterol: High levels of LDL (“bad”) cholesterol can accumulate in the arteries, forming plaques that narrow the vessels and reduce blood flow, potentially leading to heart attacks.
- Physical Inactivity: Lack of regular physical activity contributes to weight gain, high blood pressure, and high cholesterol, increasing the risk of heart disease.
- Diabetes: Diabetes significantly elevates the risk of heart disease. High blood sugar levels can damage blood vessels and nerves, increasing the risk of blood clots and other complications.
Significance of Early Detection and Prevention
Early detection and proactive preventative measures are paramount in mitigating the impact of heart disease. Regular checkups, including blood pressure and cholesterol screenings, allow for timely intervention and management of risk factors. Lifestyle modifications, such as adopting a healthy diet, engaging in regular exercise, and quitting smoking, play a pivotal role in reducing the risk of developing heart disease.
Historical Context and Advancements
The understanding of heart disease has evolved significantly over time. Early research focused on identifying symptoms and correlating them with underlying conditions. Subsequent advancements in medical technology have allowed for more precise diagnoses and targeted treatments. From angioplasty and stenting to heart valve replacements and pacemakers, modern medicine offers a range of interventions to address various forms of heart disease.
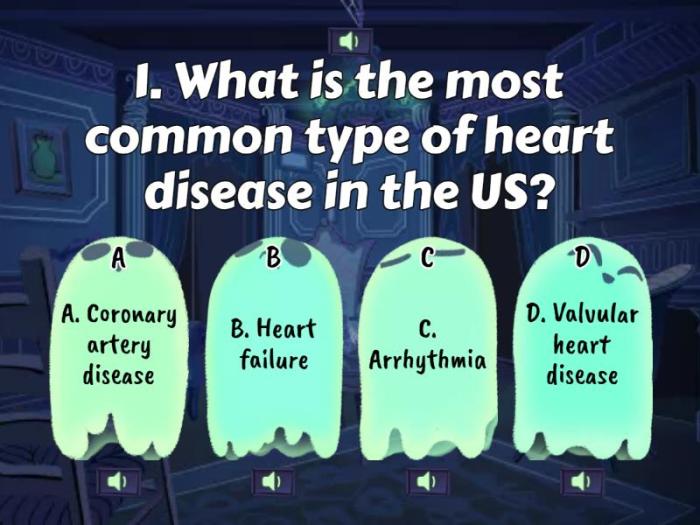
Types of Heart Disease and Prevalence
| Type of Heart Disease | Prevalence (approximate) | Description |
|---|---|---|
| Coronary Artery Disease (CAD) | High | Narrowing of the coronary arteries, reducing blood flow to the heart muscle. |
| Heart Valve Disease | Moderate | Problems with the heart valves, affecting the flow of blood through the heart. |
| Cardiomyopathy | Moderate | Conditions affecting the heart muscle, often leading to weakened or thickened heart walls. |
| Congenital Heart Defects | Moderate | Heart abnormalities present at birth, requiring intervention in some cases. |
| Peripheral Artery Disease (PAD) | Moderate | Narrowing of the arteries in the limbs, reducing blood flow to the extremities. |
Note: Prevalence figures are approximate and can vary based on factors like geographic location and population demographics.
Coronary Artery Disease (CAD)
Coronary artery disease (CAD), often referred to as coronary heart disease, is a prevalent condition characterized by the narrowing or blockage of the coronary arteries, the blood vessels that supply oxygen-rich blood to the heart muscle. This narrowing often results from the buildup of plaque, a mixture of cholesterol, fat, cellular waste products, and calcium. Understanding the mechanisms, symptoms, diagnostics, treatments, and types of CAD is crucial for prevention and effective management.
Mechanisms of CAD Development
The development of CAD is a gradual process, often spanning decades. Atherosclerosis, the primary cause, involves the formation of plaque within the inner lining of the coronary arteries. Inflammation plays a significant role in this process, as it triggers the accumulation of cholesterol and other substances. Factors such as high blood cholesterol levels, high blood pressure, smoking, diabetes, and a sedentary lifestyle accelerate plaque formation.
Genetic predisposition also contributes to an individual’s susceptibility to CAD. In essence, multiple factors interact to create an environment conducive to plaque buildup, eventually leading to narrowing and potential blockage of the arteries.
Symptoms of CAD
CAD’s symptoms can vary significantly, depending on the severity and location of the blockage. Common symptoms include chest pain (angina), which may be described as tightness, pressure, or squeezing. This pain can radiate to the jaw, neck, or arms. Shortness of breath, fatigue, and dizziness are also potential indicators. In some cases, individuals may experience no symptoms until a significant blockage occurs, leading to a heart attack or other serious complications.
It’s crucial to remember that these symptoms can mimic other conditions, and a proper diagnosis is essential.
Diagnostic Methods for CAD
Several diagnostic tools are used to detect and assess CAD. Electrocardiography (ECG) measures the electrical activity of the heart, providing information about the heart’s rhythm and potential damage. Stress tests, typically involving exercise or medication-induced stress, assess the heart’s response to increased demand. Coronary angiography, a procedure involving the injection of contrast dye into the coronary arteries, allows visualization of the arteries and identification of blockages.
Other diagnostic methods may include cardiac CT scans and blood tests to measure cholesterol and other markers. The choice of diagnostic method depends on the individual’s symptoms and overall health.
Treatment Options for CAD
Treatment options for CAD are multifaceted, ranging from lifestyle modifications to medications and procedures. Lifestyle changes, such as adopting a heart-healthy diet, regular exercise, and smoking cessation, are crucial for managing CAD and preventing further progression. Medications, including cholesterol-lowering drugs (statins), blood pressure medications, and antiplatelet agents, play a vital role in reducing the risk of heart attacks and strokes.
Procedures such as angioplasty and stenting can mechanically open blocked arteries, improving blood flow. In more severe cases, coronary artery bypass grafting (CABG) may be necessary to reroute blood flow around blocked sections of the arteries. Treatment plans are personalized based on the severity of the disease and the individual’s overall health.
Comparison of CAD Types
CAD can manifest in various ways. Stable angina, a common type, is characterized by predictable chest pain triggered by exertion or stress. Unstable angina, a more serious form, involves unpredictable chest pain that may occur at rest or with minimal exertion. Silent CAD, a less recognized form, doesn’t present with noticeable symptoms. The presence or absence of symptoms, the location and severity of the blockage, and the patient’s overall health can influence the classification and treatment approach.
Stages of CAD Progression and Corresponding Symptoms
| Stage | Description | Symptoms |
|---|---|---|
| Early Stage | Initial plaque buildup in the arteries. | Often asymptomatic or may present with mild, intermittent chest pain. |
| Intermediate Stage | Plaque continues to grow, potentially narrowing the arteries. | Symptoms may include chest pain during exertion, shortness of breath, and fatigue. |
| Advanced Stage | Significant plaque buildup causing significant narrowing or complete blockage. | Severe chest pain, shortness of breath, even at rest, and potentially heart attack or stroke. |
This table Artikels the progression of CAD, highlighting the potential escalation of symptoms. Early detection and intervention are crucial for managing the condition and mitigating potential complications.
Learning about different types of heart disease can be overwhelming, but understanding the various conditions is key to effective treatment. For example, if you or someone you know has a heart condition requiring crutches for mobility, it’s important to know the proper techniques. Knowing how to use crutches correctly is crucial for maintaining balance and avoiding further injury, which is vital when managing any type of heart disease.
Luckily, there’s a great resource for learning how to use crutches effectively: how to use crutches. This knowledge can then help you better understand your heart health journey and make informed decisions about your care.
Valvular Heart Disease
Valvular heart disease is a condition affecting the heart’s valves, which regulate the flow of blood through the heart. These valves, like tiny doors, ensure blood moves in the correct direction. When these valves become damaged or diseased, they may not function properly, leading to various complications. This can result in inefficient blood flow, potentially affecting the entire cardiovascular system.Valvular heart disease can manifest in various forms, each characterized by specific mechanisms of valve dysfunction.
Understanding the different types, causes, symptoms, and treatments is crucial for effective management and prevention of related complications. This will help individuals and healthcare providers better navigate the complexities of this condition.
Types of Valvular Heart Disease
Valvular heart disease encompasses several types, each affecting different heart valves and exhibiting distinct characteristics. These include mitral valve disease, aortic valve disease, tricuspid valve disease, and pulmonary valve disease. Each valve’s specific role in blood flow contributes to the unique symptoms and treatment approaches associated with its dysfunction.
Mitral Valve Disease
Mitral valve disease, affecting the valve between the left atrium and left ventricle, can manifest as mitral stenosis or mitral regurgitation. Mitral stenosis involves the narrowing of the valve opening, hindering blood flow from the left atrium to the left ventricle. Mitral regurgitation, conversely, occurs when the valve doesn’t close completely, allowing blood to leak back into the left atrium during contraction.
Rheumatic fever is a significant contributor to mitral valve disease, as well as age-related degenerative changes.
Aortic Valve Disease
Aortic valve disease, affecting the valve between the left ventricle and the aorta, can present as aortic stenosis or aortic regurgitation. Aortic stenosis involves the narrowing of the valve opening, hindering blood flow from the left ventricle to the aorta. Aortic regurgitation occurs when the valve doesn’t close completely, allowing blood to leak back into the left ventricle during relaxation.
Atherosclerosis, high blood pressure, and age-related calcification are common contributing factors.
Tricuspid Valve Disease
Tricuspid valve disease, affecting the valve between the right atrium and right ventricle, is less common than mitral or aortic valve disease. It can manifest as tricuspid stenosis or tricuspid regurgitation. Tricuspid stenosis restricts blood flow from the right atrium to the right ventricle. Tricuspid regurgitation occurs when the valve doesn’t close completely, allowing blood to flow back into the right atrium.
Heart disease comes in many forms, each with its own set of symptoms and risk factors. Understanding these types is crucial for prevention and treatment. Sometimes, medications like antidepressants play a role in managing risk factors. For example, comparing the similarities and differences between antidepressants like Wellbutrin and Zoloft can be helpful in understanding how they might affect overall health, including cardiovascular health.
This article explores the nuances of wellbutrin vs zoloft similarities and differences , ultimately offering valuable insights for those seeking to improve their heart health. Ultimately, learning about different types of heart disease is a vital step in maintaining a healthy lifestyle.
Infective endocarditis and certain congenital heart conditions are potential causes.
Pulmonary Valve Disease
Pulmonary valve disease, affecting the valve between the right ventricle and the pulmonary artery, is another less frequent type. It can manifest as pulmonary stenosis or pulmonary regurgitation. Pulmonary stenosis narrows the valve opening, impeding blood flow to the lungs. Pulmonary regurgitation occurs when the valve doesn’t close completely, allowing blood to leak back into the right ventricle.
Congenital heart defects are often associated with this type.
Causes and Risk Factors
Several factors can contribute to valvular heart disease. Rheumatic fever, a bacterial infection, is a significant cause, particularly for mitral valve disease. Age-related degenerative changes, high blood pressure, and atherosclerosis are common contributors. Genetic predisposition, certain medications, and infections can also play a role.
Symptoms and Diagnostic Procedures
Symptoms of valvular heart disease can vary depending on the severity and type of the condition. Common symptoms include shortness of breath, fatigue, chest pain, palpitations, and swelling in the extremities. Diagnostic procedures, including echocardiography, electrocardiography, and cardiac catheterization, help identify the specific valve abnormality and assess its impact on the heart’s function.
Treatment Options
Treatment options for valvular heart disease vary depending on the severity and type of the condition. Medical management with medications, such as diuretics and anticoagulants, can help manage symptoms. Surgical interventions, including valve repair or replacement, are often necessary for more severe cases. Minimally invasive procedures and other interventional techniques are also available, offering alternative treatment options.
Comparison of Valvular Heart Disease Types
| Valve | Stenosis | Regurgitation | Causes | Symptoms |
|---|---|---|---|---|
| Mitral | Narrowed opening | Incomplete closure | Rheumatic fever, age | Shortness of breath, fatigue |
| Aortic | Narrowed opening | Incomplete closure | Atherosclerosis, age | Chest pain, dizziness |
| Tricuspid | Narrowed opening | Incomplete closure | Infective endocarditis | Swelling in extremities |
| Pulmonary | Narrowed opening | Incomplete closure | Congenital defects | Palpitations |
Cardiomyopathy
Cardiomyopathy is a group of diseases that affect the heart muscle itself. Unlike other heart conditions that often involve the valves or blood vessels, cardiomyopathy directly impacts the heart’s ability to pump blood effectively. Understanding the different types, causes, and treatments is crucial for proper diagnosis and management.
Types of Cardiomyopathy
Cardiomyopathies are broadly categorized into three main types: hypertrophic, dilated, and restrictive. Each type presents with distinct characteristics, impacting the heart’s structure and function in unique ways.
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is characterized by an abnormally thickened heart muscle, primarily the left ventricle. This thickening can obstruct blood flow from the heart to the rest of the body. The thickening can occur in various parts of the heart, potentially leading to various degrees of obstruction.
- Causes: Genetic mutations are the most common cause of HCM, often inherited. However, acquired factors such as high blood pressure or certain medications may contribute in some cases.
- Risk Factors: Family history of HCM is a significant risk factor. Certain genetic mutations increase the likelihood of developing the condition. Age and lifestyle choices like diet and exercise habits may play a role.
- Symptoms: Symptoms can vary widely, ranging from asymptomatic cases to severe symptoms. Common symptoms include shortness of breath, chest pain, dizziness, and palpitations. Sudden cardiac death is a potential complication, particularly in young individuals.
Dilated Cardiomyopathy
Dilated cardiomyopathy (DCM) involves an enlarged heart, often with a weakened left ventricle. This weakening makes it difficult for the heart to pump blood effectively, leading to a buildup of fluid in the lungs and other parts of the body.
- Causes: Causes of DCM are diverse and can include infections (viral myocarditis), alcohol abuse, certain medications, and genetic predispositions. Metabolic disorders, such as hemochromatosis, can also contribute.
- Risk Factors: A history of heart infections, alcohol misuse, certain medical conditions, and a family history of DCM increase the risk. Certain medications, exposure to toxins, and nutritional deficiencies can also play a role.
- Symptoms: Symptoms may be subtle at first and can range from fatigue and shortness of breath to edema (swelling) in the legs and ankles. Heart failure is a significant concern in DCM, often requiring specialized management.
Restrictive Cardiomyopathy
Restrictive cardiomyopathy (RCM) is characterized by a stiffening of the heart muscle, restricting its ability to fill with blood. This stiffening hinders the heart’s capacity to accommodate the incoming blood volume.
- Causes: RCM can stem from various underlying conditions, including amyloidosis (protein buildup), sarcoidosis (inflammatory disease), and hemochromatosis. In some cases, the cause remains unknown.
- Risk Factors: Individuals with a history of certain inflammatory conditions, genetic disorders, or specific medical conditions may be at increased risk of developing RCM.
- Symptoms: Symptoms of RCM often mimic other heart conditions. Shortness of breath, fatigue, and swelling in the extremities are common. Heart failure may develop gradually.
Diagnostic Methods
Diagnosis of cardiomyopathy involves a combination of physical examinations, electrocardiograms (ECGs), echocardiograms, cardiac MRI, and blood tests. These methods provide valuable information about the heart’s structure and function.
Treatment Options
Treatment for cardiomyopathy varies depending on the type and severity of the condition. It often includes medication, lifestyle modifications, and, in severe cases, heart transplantation.
Understanding the various types of heart disease is crucial for preventative care. Learning to recognize and address passive aggressive behavior can also play a significant role in overall health, impacting stress levels and potentially reducing the risk factors for heart conditions. For example, mastering strategies for dealing with passive-aggression can improve your emotional well-being, which in turn, contributes to better heart health.
Knowing the types of heart disease and proactively managing your emotional health are both key to maintaining a healthy heart. addressing passive aggressive behavior can be a vital step in this process.
- Medications: Medications can help manage symptoms, such as heart failure, and slow the progression of the disease. Beta-blockers, ACE inhibitors, and diuretics are commonly used.
- Lifestyle Changes: Lifestyle changes, including a healthy diet, regular exercise, and weight management, can significantly improve outcomes and reduce symptoms. Smoking cessation and avoiding excessive alcohol consumption are also crucial.
- Heart Transplantation: In cases of severe heart failure, heart transplantation may be considered as a last resort. The success rate of this procedure is significant but requires careful evaluation and consideration.
Characteristics of Cardiomyopathy Types
| Cardiomyopathy Type | Characteristics | Typical Presentation |
|---|---|---|
| Hypertrophic | Thickened heart muscle, often the left ventricle | Shortness of breath, chest pain, dizziness, palpitations, potential sudden cardiac death |
| Dilated | Enlarged heart, weakened left ventricle | Fatigue, shortness of breath, edema, heart failure |
| Restrictive | Stiffened heart muscle, restricts filling | Shortness of breath, fatigue, swelling, heart failure |
Arrhythmias
Arrhythmias, or irregular heartbeats, are a common heart condition affecting millions globally. They occur when the heart’s electrical system malfunctions, disrupting the normal rhythm of contractions. This disruption can range from a slight irregularity to a life-threatening condition, depending on the type and severity of the arrhythmia. Understanding the different types, causes, and treatments is crucial for effective management and prevention.
Types of Arrhythmias
Arrhythmias are broadly categorized based on their origin in the heart’s electrical conduction system and the rate and regularity of the heartbeat. This classification allows for targeted diagnosis and treatment strategies. Common types include atrial fibrillation, supraventricular tachycardia, and ventricular tachycardia, each with unique characteristics.
Atrial Fibrillation
Atrial fibrillation (AFib) is characterized by rapid, irregular electrical signals originating in the atria. These erratic signals disrupt the normal coordination of atrial and ventricular contractions, leading to a quivering or irregular heartbeat. Causes of AFib can include underlying heart conditions like coronary artery disease, high blood pressure, and heart valve problems. Symptoms can vary widely, ranging from palpitations and shortness of breath to chest pain and dizziness.
Diagnosis often involves electrocardiograms (ECGs) and Holter monitoring to capture heart rhythm patterns over time. Treatment options include medications to control heart rate and rhythm, procedures such as catheter ablation to destroy the abnormal electrical pathways, and sometimes the implantation of pacemakers.
Supraventricular Tachycardia
Supraventricular tachycardia (SVT) is a rapid heart rate originating above the ventricles, specifically in the atria or the electrical pathways connecting the atria to the ventricles. Common causes include stress, caffeine, alcohol, and certain medical conditions. Symptoms often include palpitations, a pounding heart, shortness of breath, and anxiety. Diagnosis relies on ECGs and other diagnostic tools to identify the rapid heart rhythm and its origin.
Treatment options may include medications to slow the heart rate, vagal maneuvers (like carotid sinus massage), and procedures like catheter ablation to eliminate the abnormal electrical pathway.
Ventricular Tachycardia
Ventricular tachycardia (VT) is a rapid heart rhythm originating in the ventricles. This can be a dangerous condition as the ventricles may not have sufficient time to fill with blood before contracting, potentially reducing cardiac output. Causes of VT can include heart disease, electrolyte imbalances, and certain medications. Symptoms include palpitations, lightheadedness, chest pain, shortness of breath, and even loss of consciousness.
Diagnosis is usually made through ECGs, and other diagnostic tools, including Holter monitoring, may be employed. Treatment options range from medications to control the heart rate and rhythm to procedures like catheter ablation or implantable cardioverter-defibrillators (ICDs) to restore a normal rhythm.
Lifestyle Influences on Arrhythmias
Several lifestyle factors can influence the occurrence of arrhythmias. Maintaining a healthy weight, regular exercise, and a balanced diet are crucial. Smoking cessation and limiting alcohol and caffeine consumption are also important. Stress management techniques, like meditation and yoga, can play a vital role in minimizing the risk of arrhythmias.
Arrhythmia Categorization Table
| Type of Arrhythmia | Origin | Characteristics |
|---|---|---|
| Atrial Fibrillation | Atria | Rapid, irregular heartbeat; quivering atria |
| Supraventricular Tachycardia | Above ventricles (atria or AV node) | Rapid, regular heartbeat; originating above the ventricles |
| Ventricular Tachycardia | Ventricles | Rapid, regular heartbeat; originating in the ventricles |
Congenital Heart Defects
Congenital heart defects (CHDs) are structural abnormalities in the heart that are present at birth. These conditions can range from mild, requiring no intervention, to severe, needing immediate surgical repair. Understanding these defects is crucial for early diagnosis and appropriate treatment, often impacting a child’s quality of life.
Types of Congenital Heart Defects
Congenital heart defects encompass a wide spectrum of structural abnormalities. They can involve the heart valves, chambers, or major blood vessels connected to the heart. These abnormalities can lead to various physiological consequences, depending on the specific defect. Some defects affect the flow of blood through the heart, causing it to become overworked or inadequately oxygenated. Others impact the structure of the heart, potentially compromising its ability to pump blood efficiently.
Causes and Risk Factors
While the exact cause of most congenital heart defects remains unknown, certain factors are associated with an increased risk. Genetic predispositions play a role, with some families having a higher likelihood of CHDs. Maternal factors, such as infections during pregnancy (e.g., rubella) or certain medications, are also recognized risk factors. Maternal diabetes, and exposure to certain environmental toxins during pregnancy are also known to potentially increase the risk.
Diagnostic Methods
Early detection is critical for successful management of CHDs. Prenatal screening, such as ultrasound during pregnancy, can identify some defects. After birth, various diagnostic tools are used, including:
- Echocardiography: This non-invasive technique uses sound waves to create images of the heart, allowing visualization of its structure and function. It’s a cornerstone in CHD diagnosis, providing detailed information about the size, shape, and movement of heart structures.
- Electrocardiography (ECG): This procedure records the electrical activity of the heart, helping assess the heart’s rhythm and potentially identify abnormal electrical conduction patterns, a crucial aspect in the evaluation of heart defects.
- Cardiac Catheterization: In more complex cases, a thin tube (catheter) is inserted into a blood vessel and guided to the heart. This procedure allows direct visualization of the heart’s structures, measurement of pressures, and collection of blood samples. It provides critical information for planning surgical interventions.
- Chest X-rays: This imaging method provides a general view of the heart’s size and position in the chest, helping identify possible enlargement or abnormalities in its shape.
Treatment Options
Treatment approaches for CHDs vary greatly, depending on the severity and type of defect. Interventions can range from simple medication management to complex surgical procedures.
- Infancy: In some cases, immediate intervention is necessary during infancy to correct critical defects. These interventions may include cardiac catheterization procedures or open-heart surgery. These procedures often involve patching holes in the heart, repairing narrowed vessels, or replacing faulty valves.
- Childhood and Adolescence: As children grow, ongoing monitoring and management are crucial. Some children may require multiple surgeries or interventions to address the progression of the defect. Carefully monitored growth and development are essential, ensuring appropriate physical activity and nutritional support.
- Adulthood: Adults with CHDs often require ongoing medical care to manage potential complications. This care may involve regular check-ups, medication adjustments, and interventions as needed. For example, adults with certain CHDs might need specialized cardiac consultations to address long-term consequences.
Common Types of Congenital Heart Defects
| Defect Type | Typical Presentation |
|---|---|
| Ventricular Septal Defect (VSD) | A hole between the two lower chambers of the heart, potentially causing increased blood flow to the lungs. Symptoms can range from none to significant, depending on the size of the defect. |
| Atrial Septal Defect (ASD) | A hole between the two upper chambers of the heart. Usually asymptomatic in milder forms, potentially leading to increased blood flow to the lungs and an enlarged right atrium. |
| Tetralogy of Fallot | A combination of four defects: a ventricular septal defect, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy. Symptoms often include bluish skin coloration (cyanosis), shortness of breath, and difficulty feeding in infants. |
| Patent Ductus Arteriosus (PDA) | A blood vessel connecting the aorta and pulmonary artery remains open after birth. It can lead to increased blood flow to the lungs and potentially increased workload on the heart. Symptoms may vary from mild to severe. |
Heart Failure
Heart failure is a complex condition where the heart is unable to pump enough blood to meet the body’s needs. This can lead to a buildup of fluid in the lungs and other tissues, causing shortness of breath, fatigue, and swelling. Understanding the different types of heart failure and their management is crucial for effective patient care.
Types of Heart Failure
Heart failure is broadly categorized into systolic and diastolic heart failure, each with distinct characteristics. These differences lie in how the heart contracts and relaxes during the pumping cycle.
Systolic Heart Failure
Systolic heart failure occurs when the heart’s ventricles are unable to contract effectively. This reduced pumping ability results in a decreased stroke volume, meaning less blood is ejected with each beat. Causes of systolic heart failure often include coronary artery disease (CAD), high blood pressure, and previous heart attacks. Risk factors encompass smoking, obesity, diabetes, and a family history of heart conditions.
Symptoms can include shortness of breath, especially with exertion, fatigue, and swelling in the legs and ankles.
Diastolic Heart Failure
Diastolic heart failure, conversely, involves an inability of the ventricles to relax and fill properly. Although the heart may pump adequately, it doesn’t fill with enough blood before each beat. Causes include high blood pressure, aging, and certain medications. Risk factors frequently overlap with those for systolic heart failure, such as obesity, diabetes, and a family history of heart conditions.
Symptoms of diastolic heart failure often mirror those of systolic heart failure, such as shortness of breath, fatigue, and swelling, but may also include irregular heartbeats or chest pain.
Diagnostic Methods for Heart Failure
Diagnosing heart failure involves a combination of methods. Physical examinations, including listening to the heart with a stethoscope, provide initial clues. Electrocardiograms (ECGs) can reveal electrical activity abnormalities. Echocardiograms offer detailed images of the heart’s structure and function, allowing assessment of ejection fraction and ventricular filling pressures. Blood tests can help evaluate kidney function and detect elevated levels of certain hormones associated with heart failure.
Other imaging techniques, such as chest X-rays and cardiac catheterizations, may also be used in specific cases.
Treatment Options for Heart Failure
Treatment for heart failure is multifaceted and aims to improve symptoms, slow disease progression, and enhance quality of life. Medications play a central role, including ACE inhibitors, beta-blockers, and diuretics. Lifestyle changes are crucial, emphasizing a balanced diet, regular exercise, and weight management. In some cases, device therapies, such as implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy devices (CRTs), may be necessary to help regulate heart rhythm or improve pumping efficiency.
Stages of Heart Failure and Management Strategies
Heart failure is often categorized into stages based on the severity of the condition. Early stages may involve lifestyle modifications and medication. As the disease progresses, more intensive interventions, including device therapies, may become necessary. A multidisciplinary approach involving cardiologists, nurses, and other healthcare professionals is vital to optimize patient management and tailor treatment plans to individual needs and disease progression.
Ongoing monitoring and adjustments to the treatment plan are essential to manage the condition effectively.
Peripheral Artery Disease (PAD): Types Of Heart Disease
Peripheral artery disease (PAD) is a condition that affects the blood vessels outside of the heart and brain. It’s characterized by a narrowing of the arteries, reducing blood flow to the limbs, most commonly the legs and feet. While often overlooked, PAD can significantly impact a person’s quality of life and, if left untreated, can lead to serious complications.
Understanding its causes, symptoms, and treatment is crucial for early detection and effective management.
Causes of PAD
PAD primarily develops due to atherosclerosis, a buildup of plaque in the artery walls. This plaque is composed of cholesterol, fats, and other substances, which gradually narrow the arteries. Factors such as high blood pressure, high cholesterol, smoking, diabetes, and a family history of cardiovascular disease increase the risk of atherosclerosis and PAD. Uncontrolled diabetes, in particular, accelerates the process of atherosclerosis and is a significant risk factor for PAD.
Symptoms of PAD
Symptoms of PAD often begin subtly, making early detection challenging. Common symptoms include pain, cramping, numbness, or tingling in the legs and feet, especially during exercise. This pain, often described as claudication, typically subsides with rest. Other potential symptoms include skin changes such as discoloration, hair loss, or sores on the legs and feet that heal slowly.
In severe cases, PAD can lead to critical limb ischemia, a serious condition that can result in pain, ulcers, and even gangrene, requiring possible amputation.
Diagnostic Methods for PAD
Diagnosing PAD involves a combination of physical examinations and diagnostic tests. A physical exam may reveal reduced or absent pulses in the legs and feet, along with skin changes characteristic of PAD. Diagnostic tests include ankle-brachial index (ABI) measurements, which compare blood pressure in the arms and ankles. An abnormal ABI suggests a narrowing of the arteries.
Other tests such as angiography (a procedure that uses X-rays and a contrast dye to visualize the arteries) and ultrasound can also be used to confirm the diagnosis and assess the extent of the blockage.
Risk Factors for PAD, Types of heart disease
Several factors significantly increase the risk of developing PAD. These include smoking, high blood pressure, high cholesterol, diabetes, obesity, a family history of cardiovascular disease, and age. Maintaining a healthy weight, managing blood sugar levels, and quitting smoking are vital for reducing the risk of PAD.
Impact of PAD on Overall Health
PAD can significantly impact overall health, affecting mobility, quality of life, and increasing the risk of other cardiovascular events. The pain and limitations associated with PAD can restrict daily activities and lead to depression or anxiety. PAD also increases the risk of heart attack, stroke, and other cardiovascular diseases. Prolonged poor blood flow can damage tissues and organs, increasing the risk of infections and other health complications.
Treatment Options for PAD
Treatment options for PAD aim to improve blood flow, manage risk factors, and prevent complications. Lifestyle modifications such as regular exercise, a healthy diet, and smoking cessation are crucial for managing PAD. Medications, including blood thinners and cholesterol-lowering drugs, may be prescribed to improve blood flow and control risk factors. In some cases, procedures such as angioplasty (widening of the arteries) or bypass surgery may be necessary to restore blood flow.
Regular monitoring of blood pressure, blood sugar, and cholesterol levels is essential to control the disease and prevent future complications.
Importance of Regular Monitoring and Follow-up Care
Regular monitoring and follow-up care are essential for managing PAD effectively. This includes regular checkups with a healthcare professional to monitor symptoms, assess blood flow, and adjust treatment plans as needed. Close monitoring helps detect any progression of the disease and allows for prompt intervention to prevent serious complications. Following prescribed medications and lifestyle recommendations is crucial for long-term management and improving overall health outcomes.
Comparison of PAD with Other Cardiovascular Conditions
| Characteristic | Peripheral Artery Disease (PAD) | Coronary Artery Disease (CAD) | Valvular Heart Disease | Congenital Heart Defects |
|---|---|---|---|---|
| Location of affected vessels | Arteries outside the heart | Coronary arteries (heart) | Heart valves | Heart structures present at birth |
| Symptoms | Leg pain, cramping, numbness, skin changes | Chest pain, shortness of breath, fatigue | Heart murmur, shortness of breath, fatigue | Depends on the defect, cyanosis, shortness of breath |
| Causes | Atherosclerosis | Atherosclerosis | Valve damage or malformation | Genetic or environmental factors |
Last Word
In conclusion, this comprehensive overview highlights the diverse range of heart conditions. From the common to the less frequent, each type demands a unique approach to diagnosis and treatment. Early detection, a healthy lifestyle, and adherence to medical advice are paramount in mitigating the risk and managing these diseases. We hope this information provides a foundation for understanding heart health and encourages proactive steps towards a healthier future.









