Implant for sleep apnea offers a novel approach to treating this common sleep disorder. This in-depth exploration delves into various implant types, surgical procedures, patient selection, effectiveness, benefits, risks, costs, and future innovations. We’ll uncover the intricate details of this cutting-edge treatment option.
From understanding the different implant mechanisms and comparing their effectiveness to exploring the surgical process and potential complications, this comprehensive guide provides a detailed overview. We will also investigate the factors involved in patient selection and evaluation, ensuring the procedure is tailored to individual needs. The cost and insurance considerations are also addressed, along with future advancements and ongoing research.
Types of Implants for Sleep Apnea: Implant For Sleep Apnea
Implants offer a novel approach to treating sleep apnea, a prevalent sleep disorder characterized by pauses in breathing during sleep. These devices aim to address the underlying anatomical or physiological issues contributing to these pauses, providing a long-term solution compared to CPAP therapy for some patients. While not a universal cure, they present a viable alternative for individuals who haven’t found adequate relief through other methods.These implants work by manipulating the muscles or tissues in the upper airway, thereby promoting unobstructed airflow during sleep.
The effectiveness and suitability of each type of implant vary depending on the specific cause of sleep apnea and the individual patient’s characteristics. It’s crucial to discuss potential benefits and risks with a qualified healthcare professional to determine if implant therapy is an appropriate option.
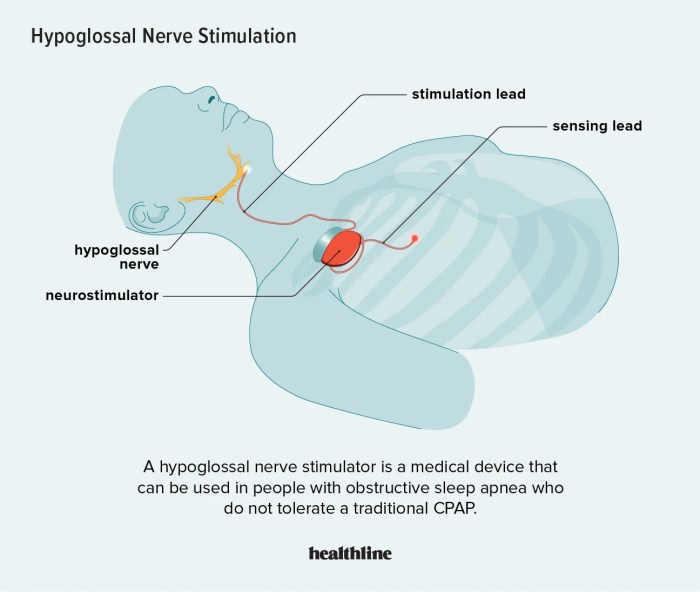
Hypoglossal Nerve Stimulators
Hypoglossal nerve stimulators are surgically implanted devices that stimulate the hypoglossal nerve, which controls the tongue’s movement. By stimulating the nerve, the device gently repositions the tongue, preventing it from collapsing into the airway during sleep. This mechanism effectively reduces or eliminates the obstructions that lead to apnea events. Examples of brands include the Inspire device, which is a popular choice.
Upper Airway Implants
Upper airway implants are designed to physically support the airway structures, preventing collapse during sleep. These devices typically involve placing a small, customized implant within the upper airway, such as the base of the tongue or the soft palate. The implant’s shape and material are carefully selected to maintain the airway’s patency. This technique can be particularly beneficial for individuals with anatomical abnormalities in the upper airway.
Specific examples of this technology remain relatively limited in the market compared to other options.
Comparison of Implant Types
| Implant Type | Mechanism of Action | Effectiveness | Side Effects | Cost |
|---|---|---|---|---|
| Hypoglossal Nerve Stimulators | Stimulates the hypoglossal nerve to reposition the tongue. | Generally considered effective in reducing apnea events and improving sleep quality for many patients. Success rates vary depending on individual cases. | Potential for discomfort, pain, or infection at the surgical site. Some patients experience speech difficulties or other side effects related to nerve stimulation. | Moderate to high, depending on the specific device and associated procedures. |
| Upper Airway Implants | Physically supports the upper airway structures, preventing collapse. | Effectiveness can vary, often depending on the specific anatomical issue. Some studies show promising results, but more long-term data is needed. | Potential for discomfort, pain, or infection at the surgical site. Implant migration or other complications are possible. | Moderate to high, similar to hypoglossal nerve stimulators, potentially influenced by implant material and complexity. |
Implant Procedure and Surgery
The surgical implantation of sleep apnea devices is a complex procedure requiring meticulous planning and execution. The specific techniques and approaches vary based on the type of implant, the patient’s anatomy, and the surgeon’s expertise. A thorough understanding of the procedure is crucial for both the patient and the medical team to ensure a safe and successful outcome.
Surgical Procedures Involved
The surgical procedures for implanting sleep apnea devices involve precise incisions and careful manipulation of tissues to minimize trauma and maximize device effectiveness. Open and minimally invasive approaches are common, each with its own set of advantages and considerations. The selection of the surgical approach is dependent on the specific device being implanted and the patient’s individual circumstances.
Pre-operative Care
Pre-operative care is critical to ensure the patient’s well-being and optimize the surgical outcome. This involves a comprehensive medical evaluation, including blood tests, imaging studies (such as X-rays or CT scans), and discussions with the anesthesiologist. The patient should provide a complete medical history, including any allergies or previous surgeries. The pre-operative preparation aims to identify and mitigate potential risks.
The patient is often instructed to abstain from food and drink for a certain period before the surgery.
Post-operative Care
Post-operative care is essential for the patient’s recovery and to monitor for complications. This includes pain management, wound care, and close monitoring for signs of infection or bleeding. The patient will be advised on the appropriate medications and follow-up appointments. Detailed instructions regarding activity limitations and dietary restrictions will be provided to facilitate healing and prevent complications.
Post-operative care instructions are tailored to the individual patient and the specific implant procedure.
Potential Complications and Risks
Potential complications and risks associated with sleep apnea device implantation, like any surgical procedure, include infection, bleeding, nerve damage, and device malfunction. These risks are generally low with experienced surgeons and meticulous surgical techniques. Proper pre-operative evaluation and post-operative care minimize the chances of complications. Thorough discussion with the medical team about the specific risks associated with the selected procedure is crucial for informed consent.
I’ve been researching sleep apnea implants lately, and it’s fascinating how much medical technology is advancing. While exploring different treatment options, I stumbled upon the importance of immunizations in managing sickle cell disease, a condition that requires a comprehensive approach to care. Understanding the role of immunizations to care for sickle cell disease is crucial for patients, highlighting the interconnectedness of various health challenges.
Ultimately, I’m back to sleep apnea implants, and the various approaches to tackling this common condition.
Steps Involved in the Implantation Process
The implantation process is a multi-step procedure, demanding precision and expertise. Each step is crucial for ensuring the device’s functionality and the patient’s well-being.
Step-by-Step Guide
- Patient Preparation: The patient is prepared for surgery by fasting, having blood tests, and undergoing necessary imaging. This step ensures a safe and clean surgical environment. Medications and allergies are documented to facilitate the best possible patient care.
- Anesthesia: The patient receives appropriate anesthesia to ensure comfort and prevent pain during the surgical procedure. The type of anesthesia is selected based on the patient’s health and the specific procedure.
- Surgical Incision: The surgeon makes a precise incision in the designated area. The incision site is carefully chosen to minimize scarring and maximize device access.
- Device Implantation: The surgeon carefully implants the sleep apnea device according to the manufacturer’s instructions. The precise placement of the device is crucial for optimal effectiveness and minimal discomfort.
- Closure and Dressing: The incision is meticulously closed, and the surgical site is dressed to promote healing and prevent infection. Sterile techniques are used throughout this process.
- Post-operative Monitoring: The patient is closely monitored in a recovery area to observe for any complications, such as bleeding or infection. Vital signs are monitored closely.
Patient Selection and Evaluation
Choosing the right patient for an implantable sleep apnea device is crucial for maximizing treatment success and minimizing complications. Careful evaluation ensures the procedure is the best course of action and that the selected implant is the most suitable for the individual’s specific needs and medical profile. This process involves a thorough assessment of the patient’s medical history, sleep study results, and overall health to determine if the implant is the most effective and appropriate treatment option.Patient selection is not a one-size-fits-all approach.
Different implant types cater to various degrees and types of sleep apnea. Therefore, the evaluation process must consider the specific characteristics of each implant and how they align with the patient’s unique needs. This includes analyzing the potential risks and benefits of each implant in relation to the patient’s overall health.
Criteria for Patient Selection
A comprehensive evaluation process is essential to identify patients who will benefit most from implant procedures. This involves considering several key factors to ensure a positive outcome. The following table Artikels the key criteria and their weighting, which are used to assess a patient’s suitability. These criteria are not exhaustive but provide a framework for assessing patients.
| Criterion | Description | Weighting |
|---|---|---|
| Sleep Study Results | Comprehensive sleep studies, including polysomnography (PSG), are fundamental for evaluating the severity and type of sleep apnea. Results should demonstrate the presence and severity of apnea-hypopnea events (AHI), oxygen desaturation levels, and other relevant parameters. The study should specifically identify the patient’s specific sleep apnea characteristics, including the predominant type (obstructive, central, or mixed). | High (40%) |
| Medical History | A detailed medical history, including a review of current medications, allergies, previous surgeries, and underlying medical conditions (e.g., cardiovascular disease, neurological disorders), is essential. This information helps to identify potential risks and complications associated with the implant procedure. A history of complications with previous treatments for sleep apnea is also important to assess. | Medium (30%) |
| Patient Factors | Patient factors like age, overall health status, compliance with medical recommendations, and motivation for treatment play a vital role in determining success. Patients must understand the long-term commitment and responsibility associated with implant procedures and be motivated to follow all instructions. Also, patients must be psychologically fit and ready for the procedure. | Medium (20%) |
| Implant Suitability | Assessment of the specific implant type’s suitability for the patient’s condition and anatomical characteristics is crucial. This includes considering the size, shape, and design of the implant and how it aligns with the patient’s airway anatomy. | High (10%) |
Pre-operative Assessments
Pre-operative assessments are critical for determining the suitability of an implant procedure for a specific patient. These assessments include physical examinations, imaging studies (e.g., CT scans or MRI scans), and consultations with specialists to evaluate the patient’s overall health status and ensure that the procedure is appropriate. These steps help to identify potential complications and risks, and allow for adjustments or alternative treatment options if necessary.
I’ve been researching sleep apnea implants lately, and it’s fascinating how advanced the technology is getting. However, it got me thinking about the complexities of other health issues. Sometimes, conditions like type 2 diabetes can surprisingly transition into type 1 type 2 diabetes turn into type 1 , which highlights the intricate ways our bodies can malfunction.
Ultimately, though, the implant for sleep apnea seems like a very promising solution for those struggling with this common issue.
Evaluation of Implant Effectiveness
Evaluating the effectiveness of a particular implant for a specific patient involves ongoing monitoring and follow-up. Post-operative sleep studies are crucial for determining the impact of the implant on sleep apnea parameters. Measurements of AHI, oxygen saturation, and other relevant indicators are essential for evaluating the implant’s efficacy. The patient’s subjective experience and reported sleep quality are also important factors in assessing the overall effectiveness of the treatment.
Regular follow-up appointments and patient feedback are vital for ensuring that the implant is providing the desired therapeutic benefit.
Effectiveness and Outcomes
Implants for sleep apnea offer a potential pathway to improved sleep quality and overall health. Understanding their effectiveness, long-term outcomes, and potential pitfalls is crucial for informed decision-making. This section delves into the successes and challenges associated with these innovative treatments.The efficacy of implant-based sleep apnea therapies varies depending on the specific implant type, patient characteristics, and adherence to post-operative care instructions.
While not a one-size-fits-all solution, these treatments can deliver significant improvements in sleep quality and related health issues for suitable candidates.
Overview of Implant Effectiveness
The effectiveness of implants for sleep apnea treatment is generally positive, with many patients experiencing significant improvements in sleep quality and daytime function. Factors influencing success include the specific implant type, the severity of sleep apnea, and the patient’s overall health. Clinical studies and patient testimonials provide evidence of positive outcomes, but individual responses may vary.
Long-Term Outcomes and Benefits
Long-term benefits of implant use for sleep apnea include improved sleep quality, reduced daytime sleepiness, and a decrease in the severity of associated health complications. Studies suggest that sustained adherence to treatment protocols can maintain these benefits over time. Improved cardiovascular health, reduced blood pressure, and improved cognitive function are often observed in patients with successful implant integration.
Furthermore, patients often report increased energy levels and improved overall quality of life.
Potential for Implant Failure and Management
Implant failure, although less common, is a possibility. Potential causes for failure include device malfunction, infection, or adverse reactions to the implant material. Proper post-operative care and regular follow-up appointments are crucial to identify and address any potential issues promptly. If implant failure occurs, alternative treatment options can be explored, including more traditional therapies or different types of implants.
Comparison of Implant Success Rates
Success rates for different implant types vary depending on the specific implant design, patient characteristics, and the severity of sleep apnea. Detailed data on comparative success rates is available from published studies, and these studies are often referenced in discussions about the various implant types. Thorough evaluation of each patient’s needs and the specific implant’s characteristics will lead to a more accurate prediction of success.
Expected Improvements in Sleep Quality, Daytime Alertness, and Overall Health
Patients often experience noticeable improvements in sleep quality, characterized by reduced apnea events, improved sleep duration, and a more restful sleep. Daytime alertness is typically enhanced, reducing fatigue and improving concentration and cognitive function. Overall health benefits may include reduced blood pressure, improved cardiovascular function, and a decrease in the frequency of sleep apnea-related complications. Examples of such positive outcomes include improved quality of life and reduced reliance on medications for related conditions.
Benefits and Risks of Implantation
Implant procedures for sleep apnea offer a potential solution for individuals struggling with this condition. However, like any medical intervention, they come with inherent advantages and disadvantages. Understanding these aspects is crucial for patients considering this option and for healthcare professionals guiding them through the decision-making process.The benefits of these implants extend beyond simply improving sleep quality. They aim to address the underlying cause of sleep apnea, leading to potential improvements in overall health and well-being.
Conversely, potential risks and complications require careful consideration and thorough evaluation. The choice of an implant procedure is a personal one, carefully weighing the advantages against the potential drawbacks.
So, I’ve been researching sleep apnea implants lately, and it’s fascinating how much they can help. But it got me thinking about the positive effects of regular sauna use, which could potentially be a complementary therapy. Studies show it can improve cardiovascular health and reduce inflammation, both of which might indirectly support the effectiveness of the sleep apnea implant.
Overall, the research on sleep apnea implants is promising, and I’m excited to see how it progresses.
Advantages of Implantation
Surgical implants for sleep apnea aim to address the root cause of the disorder, offering the potential for long-term solutions. This differs from CPAP therapy, which treats symptoms but not the underlying anatomical issue. The advantages are multifaceted, impacting sleep quality, cardiovascular health, and overall well-being. By addressing the physical obstruction, implants can improve the quality of sleep, leading to increased energy levels, better cognitive function, and reduced daytime sleepiness.
Potential Risks and Side Effects
Any surgical procedure carries inherent risks, and implant procedures for sleep apnea are no exception. Potential complications include infection, bleeding, adverse reactions to anesthesia, and damage to surrounding tissues. Proper patient selection and meticulous surgical technique are essential to minimize these risks. Thorough pre-operative evaluations, including medical history reviews and assessments of patient risk factors, are critical.
Potential Benefits for Patient Quality of Life
Improved sleep quality is a primary benefit, leading to increased daytime alertness, reduced fatigue, and enhanced cognitive function. Furthermore, the resolution of sleep apnea symptoms can positively impact cardiovascular health. Studies have shown a correlation between sleep apnea and an increased risk of hypertension and other cardiovascular diseases. Resolution of these symptoms could translate to a reduced risk of these complications.
Potential Complications After Implant Procedures
Post-operative complications may arise, including infection at the implant site, bleeding, and discomfort. These complications can be managed with appropriate medical intervention. The need for follow-up care, including regular check-ups and adjustments to the implant, is also important. Patient adherence to post-operative instructions is critical for successful outcomes.
Comparison of Implant Types
| Implant Type | Benefits | Risks |
|---|---|---|
| Example Implant 1 (e.g., genioglossus advancement) | Potentially effective long-term solution for structural abnormalities, improved airway patency. | Potential for nerve damage, limited jaw movement, and discomfort during recovery. |
| Example Implant 2 (e.g., palatal implants) | May offer a minimally invasive approach for specific cases, targeted treatment. | Potential for implant rejection, infection, and limited long-term effectiveness depending on the patient’s anatomy. |
Cost and Insurance Coverage

Deciding on any medical procedure, especially one as involved as an implant for sleep apnea, necessitates careful consideration of the financial implications. Understanding the costs and potential insurance coverage is crucial for making an informed decision. This section delves into the financial aspects of this treatment option, enabling patients to anticipate and prepare for the expenses involved.
Costs Associated with Implant Procedures, Implant for sleep apnea
The total cost of an implant procedure encompasses various elements. Surgery is a significant expense, factoring in the operating room fees, anesthesia, and the surgeon’s fees. The cost of the implant itself varies depending on the specific device and its features. Follow-up care, including consultations, monitoring appointments, and potential adjustments or revisions, also contributes to the overall expenditure.
Factors Affecting the Overall Cost
Several factors influence the total cost of implant procedures. The complexity of the surgery, the specific type of implant selected, and the patient’s specific needs, such as the need for additional procedures or specialized care, impact the final price. Geographic location can also play a role, as costs may differ between regions. Finally, the extent of post-operative care needed may also influence the total cost.
Procedures for Seeking Insurance Coverage
Navigating insurance coverage for implant procedures requires a proactive approach. Patients should meticulously review their insurance policy documents, specifically looking for coverage of surgical procedures, medical devices, and follow-up care. Pre-authorization is often necessary for procedures not routinely covered. Consulting with the insurance provider to confirm coverage and potential out-of-pocket expenses is crucial. Patients should also request a pre-authorization form from the insurance provider well in advance of the procedure.
Examples of Insurance Policies Covering Implant Procedures
Many insurance plans, especially those encompassing comprehensive medical coverage, may cover some or all of the costs associated with sleep apnea implants. However, specific coverage varies greatly between plans. Some plans might cover the implant itself, while others may only cover the surgical procedure. Examples of insurance policies that might cover implant procedures include plans with a broad scope of medical benefits, including those that provide extensive coverage for surgical procedures and medical devices.
Determining Financial Implications
Assessing the financial implications of choosing an implant for sleep apnea treatment requires careful budgeting and planning. Patients should obtain pre-authorization from their insurance company to understand the extent of coverage and associated costs. It’s prudent to request an itemized breakdown of all potential expenses, including surgery, implants, and follow-up care. This enables patients to make a well-informed decision, taking into account both the medical benefits and the financial burden.
Estimating potential out-of-pocket expenses is essential for financial planning.
Future Trends and Innovations
The field of sleep apnea treatment is constantly evolving, driven by ongoing research and a desire for more effective and minimally invasive solutions. Advancements in implant technology promise to revolutionize care, potentially leading to improved outcomes and quality of life for patients. This exploration delves into emerging trends and innovations in implant technology for sleep apnea, focusing on potential future advancements in implant design and surgical techniques, examples of new implant technologies being researched, and ongoing research studies.Technological advancements are paving the way for more precise and personalized approaches to sleep apnea treatment.
The focus on improved implant design, along with the development of sophisticated surgical techniques, is poised to significantly impact patient care. These innovations are expected to address current limitations, ultimately enhancing the efficacy and safety of implant-based therapies.
Emerging Implant Designs
Research is actively exploring innovative implant designs that address limitations of current devices. These advancements aim to enhance comfort, reduce the risk of complications, and improve treatment efficacy. Examples include the development of more biocompatible materials, advanced micro-pump technologies for drug delivery, and sophisticated sensors for real-time monitoring of airway pressure. Furthermore, the design is becoming increasingly focused on personalization to optimize individual treatment.
Surgical Techniques
Minimally invasive surgical techniques are also advancing, leading to less invasive procedures and faster recovery times. These procedures focus on improving precision and accuracy during implantation, which could translate into improved outcomes and reduced post-operative discomfort. For example, advancements in robotic surgery could potentially improve the accuracy and precision of implant placement, minimizing the risk of complications.
New Implant Technologies
Several promising new implant technologies are currently under research and development. These technologies aim to improve the effectiveness of existing treatments and address limitations in current options. One area of interest is the development of implantable devices that combine pressure support with drug delivery, potentially enhancing the effectiveness of treatment for specific types of sleep apnea.
Ongoing Research Studies
Several ongoing research studies are exploring the use of implants for sleep apnea treatment. These studies are evaluating the safety and effectiveness of various implant designs, assessing long-term outcomes, and comparing them to existing treatment options. For example, some studies are evaluating the efficacy of specific types of implants in patients with specific types of sleep apnea, such as those with obstructive sleep apnea and those with central sleep apnea.
Potential Improvements in Treatment Options
New research will potentially improve treatment options for sleep apnea in several ways. Improved implant designs and surgical techniques will likely lead to more effective and personalized treatments. The incorporation of real-time monitoring and drug delivery systems could provide more precise and targeted interventions, addressing individual patient needs more effectively. This approach would be especially valuable in managing complex cases, potentially leading to more satisfactory treatment outcomes.
Last Point
In conclusion, implant for sleep apnea presents a promising treatment option for individuals struggling with this debilitating condition. While the surgical procedures and potential risks need careful consideration, the potential benefits, such as improved sleep quality and overall health, make it an attractive choice for suitable patients. Further research and technological advancements are continuously refining these procedures, promising even more effective and less invasive solutions in the future.










