Diverticulitis signs symptoms and complications – Diverticulitis signs, symptoms, and complications are a significant concern for many. This comprehensive guide delves into the intricacies of this digestive condition, from its fundamental causes and anatomical location to the various symptoms, potential complications, and effective treatment strategies. We’ll explore the spectrum of symptoms, ranging from mild discomfort to severe complications, and provide a clear understanding of how to approach diagnosis and treatment.
This detailed overview aims to equip you with the knowledge to better navigate this health concern.
Understanding diverticulitis involves comprehending the structure of the colon and its role in digestion. This knowledge is crucial in recognizing the potential issues that can arise, from the initial signs of diverticulitis to the potential complications that can develop. The discussion will also compare and contrast diverticulosis with diverticulitis, highlighting the key differences and providing a clearer picture of each condition.
Introduction to Diverticulitis
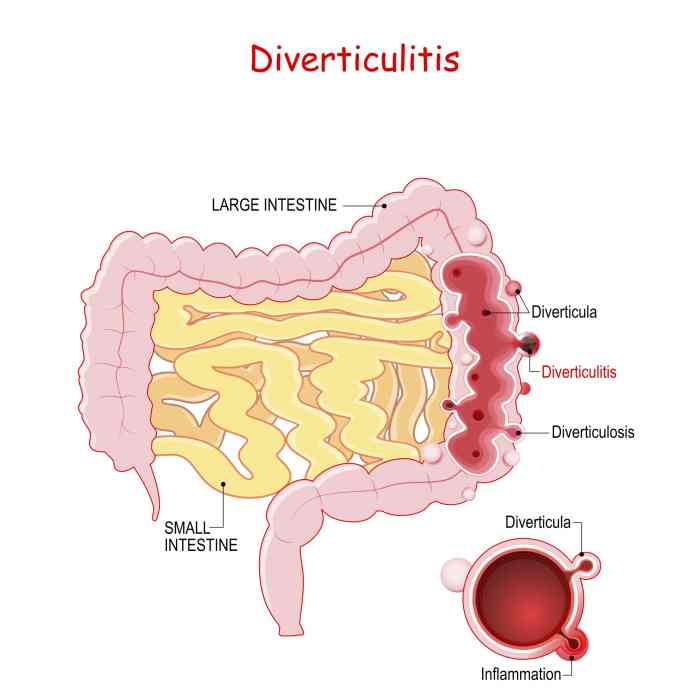
Diverticulitis is a condition characterized by inflammation and infection of small pouches (diverticula) that can form in the lining of the colon. These pouches, typically located in the sigmoid colon, are essentially outpouchings of the colon’s wall. Understanding diverticulitis involves recognizing its prevalence, risk factors, the anatomy of the colon, and the differences between diverticulosis and diverticulitis.The prevalence of diverticulitis varies geographically and increases with age.
Factors such as a low-fiber diet, smoking, and a sedentary lifestyle are associated with a higher risk of developing the condition. Understanding the structure of the digestive system, specifically the colon, is crucial to comprehend diverticulitis.
Diverticulitis can be a real pain, with symptoms like abdominal pain, fever, and changes in bowel habits. Understanding the complications is crucial, but did you know that conditions like a missing pancreas can also affect your digestive system? Learning about how to manage diverticulitis signs, symptoms, and complications is important for your overall health, and it’s worth exploring how different digestive issues relate to each other.
For example, can you live without a pancreas and other similar questions can highlight potential challenges in digestive health, which is essential when managing diverticulitis. So, understanding the bigger picture is key to managing these issues effectively.
Anatomy of the Colon and its Role in Digestion
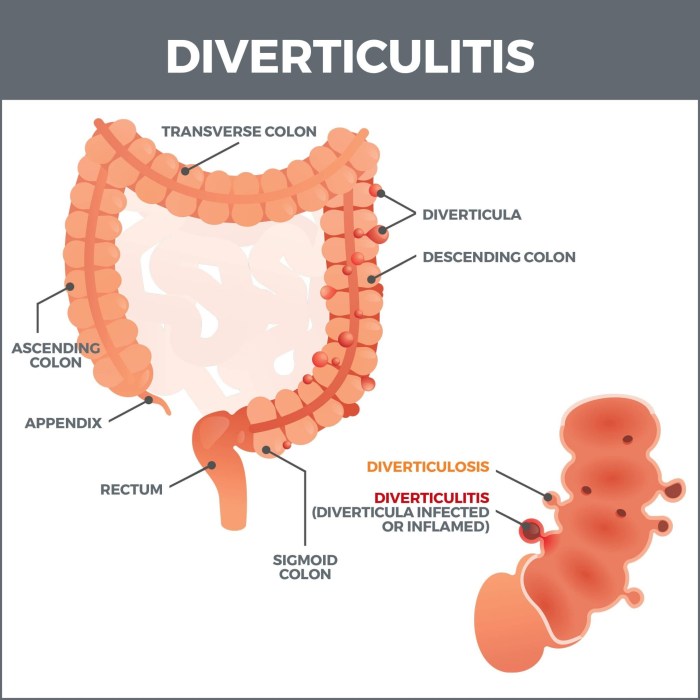
The colon, a vital part of the large intestine, is responsible for absorbing water and electrolytes from the digested food, forming and storing feces. It’s a muscular tube approximately 5 feet long, extending from the small intestine to the rectum. The colon is further subdivided into sections: the ascending colon, transverse colon, descending colon, and sigmoid colon. The sigmoid colon, located at the lower left quadrant of the abdomen, is where diverticula are most frequently found.
Infographic: Location of Diverticula
Imagine a simplified drawing of the large intestine, resembling a curved tube. The sigmoid colon, the S-shaped portion at the lower end of the large intestine, is highlighted. Small, balloon-like protrusions, the diverticula, are depicted emerging from the inner wall of the sigmoid colon. The drawing clearly shows the location of these pouches within the colon’s lining.
This graphic emphasizes the specific area of the colon where diverticula tend to form.
Diverticulosis vs. Diverticulitis
This table compares the key differences between diverticulosis and diverticulitis, highlighting the presence or absence of inflammation and infection.
| Characteristic | Diverticulosis | Diverticulitis |
|---|---|---|
| Definition | Presence of diverticula in the colon’s wall, without inflammation or infection. | Inflammation and infection of one or more diverticula. |
| Symptoms | Typically asymptomatic; may cause mild discomfort or bloating. | Often presents with abdominal pain, fever, nausea, and changes in bowel habits. |
| Complications | Rare complications include bleeding. | Potential complications include abscesses, fistulas, bowel obstruction, and perforation. |
| Treatment | Often managed with dietary adjustments. | Usually requires antibiotics and, in some cases, surgery. |
Signs and Symptoms of Diverticulitis
Diverticulitis, an inflammation of the diverticula (small pouches that can form in the digestive tract), often presents with a range of symptoms. Understanding these signs is crucial for prompt diagnosis and treatment. Recognizing the patterns of acute and chronic diverticulitis, as well as the variations based on location, can significantly aid in proper medical care.Identifying the specific symptoms and their severity can help distinguish between simple digestive issues and a more serious condition.
This understanding allows for quicker intervention, preventing potential complications. The symptoms can be influenced by various factors, including the location of the infection and the presence of any associated complications.
Common Signs and Symptoms of Acute Diverticulitis
Acute diverticulitis is characterized by a sudden onset of symptoms, often requiring immediate medical attention. Common symptoms include lower abdominal pain, typically located in the lower left quadrant, but it can also occur in other areas. This pain is often described as cramping, throbbing, or a constant ache.
Comparison of Acute and Chronic Diverticulitis Symptoms
Acute diverticulitis, as mentioned, presents with sudden, intense symptoms, whereas chronic diverticulitis symptoms tend to be less severe and more intermittent. The pain in chronic diverticulitis might be milder and occur less frequently. Chronic diverticulitis often includes a history of recurrent, milder symptoms.
Symptoms Based on Infection Location
The location of the infected diverticulum can influence the specific symptoms experienced. For instance, if the infection is in the sigmoid colon (the lower part of the large intestine), pain is often concentrated in the lower left abdomen. In contrast, diverticulitis in other parts of the large intestine might manifest with pain in a different quadrant of the abdomen.
Symptoms Associated with Diverticulitis Complications
Complications of diverticulitis, such as abscess formation or fistula development, can manifest with distinct symptoms. For example, a palpable mass in the abdomen might indicate an abscess. Fever, chills, and nausea are also common signs associated with complications.
Table of Diverticulitis Symptoms
| Symptom | Severity | Potential Causes |
|---|---|---|
| Lower abdominal pain (LLQ most common) | Moderate to severe, often cramping or throbbing | Inflammation of diverticula, infection, obstruction |
| Fever | Mild to high | Infection, complications (e.g., abscess) |
| Nausea and vomiting | Mild to moderate | Inflammation, infection, complications |
| Chills | Mild to moderate | Infection, complications |
| Change in bowel habits (e.g., diarrhea or constipation) | Mild to moderate | Inflammation, obstruction |
| Loss of appetite | Mild to moderate | Inflammation, infection, pain |
| Tenderness to the touch in the abdomen | Moderate to severe | Inflammation, infection, complications |
Complications of Diverticulitis
Diverticulitis, while often manageable, can lead to serious complications if left untreated or if the condition becomes severe. Understanding these potential complications is crucial for individuals at risk and healthcare providers to ensure timely intervention and prevent further health problems. Early recognition and appropriate management are key to minimizing the impact of these complications.
Potential Complications
Diverticulitis complications range from mild to severe, requiring varying degrees of medical attention. Recognizing these potential complications is essential for effective management and minimizing the risk of long-term health consequences. The severity and likelihood of complications depend on several factors, including the extent of the infection, individual health status, and promptness of treatment.
- Abscess Formation: A localized collection of pus can develop at the site of the diverticulitis. This can be a result of the infection spreading and becoming walled off. Abscesses can cause significant pain, fever, and tenderness in the abdomen. The likelihood of abscess formation is moderate to high, especially in individuals with poorly controlled inflammation or delayed treatment.
Management typically involves drainage of the abscess, either surgically or through percutaneous drainage, guided by imaging studies. Prompt diagnosis and treatment are vital to prevent the spread of infection and complications like sepsis.
- Fistula Formation: A fistula is an abnormal connection between two organs or between an organ and the skin. In diverticulitis, a fistula can develop between the colon and another organ, such as the bladder or vagina, or even the skin. Fistulas can cause significant drainage and discomfort, along with potential infection. The likelihood of fistula formation is moderate, often associated with recurrent or severe diverticulitis episodes.
Management can range from conservative measures like antibiotics and dietary changes to surgical intervention, depending on the location and severity of the fistula. Preventing recurrence involves managing underlying diverticulitis effectively and addressing any contributing factors.
- Sepsis: A life-threatening systemic inflammatory response to an infection. In diverticulitis, severe infection can lead to sepsis, characterized by high fever, rapid heart rate, low blood pressure, and altered mental status. The likelihood of sepsis is high, particularly with severe diverticulitis or delayed treatment. Sepsis requires immediate medical attention, including aggressive fluid resuscitation, antibiotics, and intensive care support.
Prompt diagnosis and intervention are crucial to save lives.
- Bowel Perforation: A rupture in the colon wall can occur due to severe inflammation or pressure. This can lead to the leakage of intestinal contents into the abdominal cavity, causing peritonitis, a serious inflammation of the lining of the abdomen. The likelihood of perforation is moderate to high in cases of untreated or severe diverticulitis. Management typically involves emergency surgery to repair the perforation and control infection.
Preventing perforation is paramount, emphasizing timely intervention and aggressive management of the diverticulitis.
- Obstruction: Inflammation can cause narrowing or blockage of the colon, hindering the passage of stool. This can lead to severe pain, nausea, vomiting, and abdominal distension. The likelihood of obstruction is moderate, often occurring with recurrent diverticulitis. Management can include intravenous fluids, bowel rest, and potentially surgical intervention to restore bowel function. Proactive management of diverticulitis can reduce the risk of obstruction.
Risk Factors for Complications
Several factors increase the risk of complications from diverticulitis. These include the severity of the initial infection, pre-existing medical conditions, and delayed or inadequate treatment. Factors like advanced age, a compromised immune system, and inadequate fluid intake also contribute to a higher risk.
Management Strategies, Diverticulitis signs symptoms and complications
The management of diverticulitis complications varies depending on the specific complication and its severity. This often involves a combination of medical interventions, including intravenous fluids, antibiotics, pain management, and sometimes surgical procedures. Early diagnosis and prompt treatment are essential to minimize the risk of severe complications.
Prevention Strategies
Preventing diverticulitis complications hinges on proactive measures to manage the underlying condition. A high-fiber diet, adequate hydration, and maintaining a healthy weight can help prevent diverticulitis flare-ups. Regular check-ups with a healthcare provider can also help detect and manage diverticulitis early, reducing the risk of complications.
Severity and Treatment Approach
| Severity Level | Complication | Treatment Approach |
|---|---|---|
| Mild | Abscess (small), mild fistula | Antibiotics, drainage (percutaneous or surgical), close monitoring |
| Moderate | Moderate fistula, bowel obstruction, recurrent diverticulitis | Antibiotics, bowel rest, pain management, possible surgical intervention |
| Severe | Sepsis, bowel perforation, large abscess | Emergency surgery, intensive care, aggressive antibiotic therapy, fluid resuscitation |
Diagnosis of Diverticulitis
Pinpointing diverticulitis relies on a combination of patient history, physical examination, and diagnostic imaging. A thorough understanding of the potential symptoms and their presentation is crucial for accurate diagnosis and timely treatment. The goal is to distinguish diverticulitis from other conditions that can mimic its symptoms, ensuring the right course of action for the patient.
Diagnostic Methods
A variety of methods contribute to the diagnosis of diverticulitis. These methods aim to confirm the presence of inflammation in the diverticula, assess the extent of the inflammation, and rule out other possible causes for the patient’s symptoms. Careful consideration of all available information leads to an accurate diagnosis.
Role of Imaging Techniques
Imaging plays a vital role in confirming the diagnosis of diverticulitis. Advanced imaging techniques, such as CT scans, allow healthcare professionals to visualize the affected area and identify any complications. These images offer detailed information about the presence, extent, and location of inflammation, assisting in the development of an appropriate treatment plan.
Summary of Diagnostic Tests and Procedures
Several diagnostic tests and procedures are used in the diagnosis of diverticulitis. These include:
- History and Physical Examination: A detailed medical history, including a description of the patient’s symptoms, and a physical examination, including assessment of vital signs and abdominal tenderness, provide valuable initial information. This information helps to identify potential risk factors and symptoms consistent with diverticulitis.
- Blood Tests: Complete blood count (CBC) and inflammatory markers (e.g., C-reactive protein, erythrocyte sedimentation rate) can help assess the presence of infection and inflammation. Elevated levels of these markers may indicate an active inflammatory process.
- CT Scan: A computed tomography (CT) scan is often the gold standard imaging modality for diagnosing diverticulitis. It provides detailed cross-sectional images of the abdomen, enabling visualization of the colon and surrounding structures. Contrast material is frequently used to enhance the visualization of the affected area, highlighting any inflammation or complications such as abscesses or fistulas.
- Ultrasound: Ultrasound is a less commonly used imaging technique for diagnosing diverticulitis. While it is useful in some cases, it often does not provide the same level of detail as CT scans in assessing the extent of inflammation or identifying complications.
Typical Clinical Presentation of Suspected Diverticulitis
A patient with suspected diverticulitis often presents with a combination of symptoms. These symptoms may include:
- Abdominal pain: Often localized to the lower left quadrant of the abdomen, the pain may be sharp, cramping, or a dull ache.
- Fever: A rise in body temperature is a common sign of infection, which is often present in cases of diverticulitis.
- Nausea and vomiting: These symptoms may accompany the abdominal pain and fever, indicating the body’s response to the inflammation.
- Changes in bowel habits: Patients may experience altered bowel movements, including constipation, diarrhea, or a change in stool consistency.
Comparison of Diagnostic Imaging Techniques
The following table compares and contrasts different diagnostic imaging techniques for diverticulitis:
| Imaging Technique | Advantages | Disadvantages |
|---|---|---|
| CT Scan | High resolution, detailed images of the colon and surrounding structures; can identify complications like abscesses and fistulas; widely available. | Exposure to ionizing radiation; contrast material may cause allergic reactions in some patients; more expensive than ultrasound. |
| Ultrasound | Non-invasive; does not involve ionizing radiation; relatively inexpensive. | Lower resolution images; may not adequately visualize all structures; less sensitive for identifying complications compared to CT. |
Treatment Options for Diverticulitis
Diverticulitis, an inflammation of the pouches in the colon, requires careful management. Effective treatment hinges on the severity of the infection and the individual patient’s overall health. Early intervention and appropriate treatment choices are crucial for preventing complications and promoting recovery.
Diverticulitis can be a real pain, with symptoms like abdominal pain, fever, and changes in bowel habits. It’s important to understand the signs and potential complications, like infections or bowel blockages. While we’re on the topic of digestive issues, have you ever wondered if a drink like whiskey might help with a cold? The question of whether or not alcohol is beneficial for colds is a fascinating one, and if you’d like to know more about the supposed benefits of alcohol for colds, you can check out this interesting article on does whiskey help a cold.
Ultimately, seeking professional medical advice is crucial for managing diverticulitis symptoms and preventing further complications.
Medications for Managing Diverticulitis
Medications play a vital role in treating diverticulitis, particularly in cases of mild to moderate inflammation. Antibiotics are often prescribed to combat the bacterial infection. These medications aim to reduce inflammation and prevent further complications. Specific antibiotics and their dosages are tailored to the individual patient’s needs. For example, a common approach involves a course of oral antibiotics, like metronidazole or ciprofloxacin, to clear the infection.
Pain relievers, such as ibuprofen or acetaminophen, can help manage discomfort. Dietary modifications, including a clear liquid diet, may also be recommended to allow the bowel to rest and heal.
Surgical Options for Severe Cases
Surgical intervention becomes necessary in cases of severe diverticulitis, complications like abscesses or fistulas, or recurrent episodes. The choice of surgical procedure depends on the specific situation and the extent of the damage to the colon. Surgical options can range from minimally invasive procedures, like laparoscopic surgery, to open surgeries. Laparoscopic surgery typically involves smaller incisions, leading to less post-operative pain and a quicker recovery.
However, open surgery may be necessary for more extensive procedures or complex cases.
Recovery Process and Expected Outcomes
The recovery process following treatment for diverticulitis varies based on the severity of the condition and the chosen treatment approach. Patients undergoing medical management typically experience a return to normal activities within a few days to a couple of weeks. Surgical intervention often necessitates a longer recovery period, with patients typically needing several weeks or even months to fully recover.
In general, complete recovery is possible for most individuals with appropriate medical care.
Comparison of Treatment Options
The effectiveness and side effects of different treatment approaches for diverticulitis vary. Medications are generally effective for mild cases, minimizing the need for surgery. However, in severe cases, surgical intervention might be the only option to resolve the issue. The choice of treatment depends on the individual patient’s condition and the judgment of the medical professional. Surgical options offer a definitive solution for severe cases but carry a higher risk of complications, such as infection or bleeding.
Medication-based treatment has fewer risks but may not always be sufficient. For example, if a patient experiences a recurring infection or an abscess, surgery might be required to address the underlying cause and prevent future complications.
Summary Table of Treatment Options
| Treatment Option | Effectiveness | Potential Side Effects | Suitable for |
|---|---|---|---|
| Medications (Antibiotics, Pain Relievers) | Effective for mild-moderate cases | Possible allergic reactions, gastrointestinal upset | Patients with uncomplicated diverticulitis |
| Laparoscopic Surgery | Effective for severe cases, complications | Infection, bleeding, pain, longer recovery time | Patients with abscesses, fistulas, or recurrent episodes |
| Open Surgery | Definitive solution for severe cases | Increased risk of infection, bleeding, pain, longer recovery time | Patients with extensive damage or complex cases |
Prevention and Management Strategies
Diverticulitis, while often manageable, can be prevented or its impact lessened through proactive measures. Understanding the factors that contribute to its development and implementing strategies to mitigate these risks are key to improving overall health and well-being. This section delves into preventive measures, dietary recommendations, lifestyle adjustments, and the critical role of follow-up care in managing diverticulitis.A proactive approach is essential for preventing diverticulitis or reducing its severity.
By understanding risk factors and implementing lifestyle changes, individuals can significantly decrease their likelihood of experiencing this condition. This includes not only dietary adjustments but also a focus on overall well-being.
Preventive Measures to Reduce Diverticulitis Risk
Maintaining a healthy weight, exercising regularly, and avoiding smoking are crucial steps in reducing the risk of diverticulitis. These lifestyle choices positively impact gut health and overall systemic well-being, making them integral components of a preventative strategy.
Speaking of digestive issues, diverticulitis can manifest with pain, fever, and changes in bowel habits. While the recent tuberculosis outbreak in Kansas tuberculosis outbreak in kansas highlights the importance of overall health, it’s crucial to remember that diverticulitis, a common condition, requires prompt medical attention. Severe cases can lead to complications like abscesses or fistulas, so recognizing the signs is key.
Dietary Recommendations for Managing Diverticulitis
A high-fiber diet is vital for preventing and managing diverticulitis. It promotes healthy bowel movements and reduces strain on the digestive system. A diet rich in fiber can help prevent the formation of diverticula, which are the small pouches that can become inflamed in diverticulitis.
- Increase Fiber Intake Gradually: Sudden increases in fiber intake can lead to gas and bloating. It’s best to gradually increase fiber-rich foods over time to allow the digestive system to adjust. This approach minimizes discomfort and allows the body to better utilize the increased fiber.
- Prioritize Whole Grains: Opt for whole-grain breads, cereals, and pasta over refined options. Whole grains provide more fiber and nutrients, promoting digestive health.
- Embrace Fruits and Vegetables: Include a variety of colorful fruits and vegetables in your diet. Fruits and vegetables are excellent sources of fiber and vitamins, essential for overall health.
- Choose Legumes Wisely: Legumes, such as beans, lentils, and peas, are excellent sources of fiber. However, they can cause gas in some individuals. Consider introducing them gradually into your diet.
- Limit Foods High in Refined Carbohydrates: Foods like white bread, white rice, and sugary drinks should be consumed in moderation. These foods lack the fiber needed for optimal digestive function.
Lifestyle Modifications for Diverticulitis Prevention
Maintaining a healthy weight through balanced nutrition and regular exercise can greatly reduce the risk of developing diverticulitis. Exercise promotes overall health, strengthens the body, and supports healthy digestion.
- Regular Exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Physical activity strengthens the body, improves digestion, and aids in maintaining a healthy weight.
- Manage Stress: Stress can negatively impact digestive health. Employ stress-reduction techniques such as meditation, yoga, or deep breathing exercises.
- Maintain a Healthy Weight: Obesity increases the risk of diverticulitis. Maintaining a healthy weight through a balanced diet and exercise is crucial for preventing this condition.
Follow-up Care and Monitoring
Regular checkups are essential for monitoring diverticulitis and preventing complications. This includes addressing any symptoms promptly and adhering to prescribed treatment plans.
- Regular Checkups: Schedule regular checkups with your doctor, especially if you have a history of diverticulitis or risk factors. These appointments allow for early detection of any potential issues and enable proactive management.
- Adherence to Treatment Plans: Strictly follow any prescribed medications or dietary recommendations to effectively manage diverticulitis and minimize the risk of complications.
- Prompt Symptom Reporting: Report any new or worsening symptoms to your doctor immediately. Early intervention is crucial for preventing complications and ensuring optimal health.
Dietary Recommendations for Individuals with Diverticulitis
Following a specific diet can help manage symptoms and prevent future episodes.
- Soft Foods: During an acute flare-up, a soft diet that’s easy to digest can ease discomfort. This often includes cooked fruits and vegetables, well-cooked grains, and dairy products.
- Avoid Irritating Foods: Foods like popcorn, nuts, seeds, and certain vegetables (e.g., broccoli, cabbage) can be irritating and exacerbate diverticulitis symptoms. These should be avoided or consumed in moderation during flare-ups.
- Adequate Hydration: Staying well-hydrated is crucial for digestive health. Drink plenty of water throughout the day to help prevent constipation and maintain overall bodily functions.
- Limit High-Fiber Foods During Flare-Ups: While a high-fiber diet is generally beneficial, reducing fiber intake temporarily during an acute flare-up may be necessary to minimize discomfort and allow the digestive system to heal.
Patient Education and Support
Navigating a diagnosis of diverticulitis can be overwhelming. Understanding the condition, its treatment, and the importance of self-care is crucial for successful management. This section provides essential information to empower patients and facilitate a positive recovery journey.Effective management of diverticulitis relies heavily on patient understanding and active participation. By equipping patients with knowledge and support, healthcare providers can foster adherence to treatment plans and promote long-term well-being.
Importance of Patient Education
Patient education plays a vital role in managing diverticulitis effectively. A thorough understanding of the condition, including its causes, symptoms, and potential complications, empowers patients to actively participate in their care. This knowledge allows patients to recognize early warning signs, communicate effectively with their healthcare team, and make informed decisions about their treatment and lifestyle choices. Proper education also helps reduce anxiety and promotes a sense of control over the condition.
Resources for Patients
Accessing reliable information and support is essential for patients with diverticulitis. Numerous resources can provide valuable insights and guidance. Local support groups offer a platform for connecting with others who share similar experiences, providing encouragement, and exchanging practical tips. Many hospitals and healthcare organizations have patient education websites or materials available online. These resources often contain detailed information about the condition, treatment options, and lifestyle modifications.
Patient Guide to Diverticulitis
This guide aims to provide a comprehensive understanding of diverticulitis, encompassing various aspects of the condition and its management. Understanding the cause, symptoms, and complications empowers patients to actively participate in their care. Detailed information on treatment options, including dietary changes, medication, and surgical interventions, helps patients make informed decisions. Self-care strategies and pain management techniques are also included to facilitate a smoother recovery process.
Importance of Self-Care
Self-care is crucial in managing diverticulitis. Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques, can significantly impact the overall well-being of the patient. These strategies contribute to reducing inflammation, improving digestion, and promoting a faster recovery. Furthermore, a patient-centered approach that emphasizes self-care can empower individuals to take control of their health and well-being.
Strategies for Managing Pain and Discomfort
Diverticulitis can cause significant pain and discomfort. Managing these symptoms effectively is crucial for a comfortable recovery. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate mild to moderate pain. Applying heat or cold packs to the affected area may also provide relief. Adequate hydration and a balanced diet can contribute to managing pain and discomfort.
It’s essential to communicate any persistent or worsening pain to the healthcare provider.
Reliable Online Resources
Numerous reliable online resources provide valuable information for patients with diverticulitis. Reputable medical organizations, such as the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), offer detailed information and support. Furthermore, patient advocacy groups and dedicated websites offer insights into various aspects of the condition. However, it is crucial to verify the credibility of online resources and consult with a healthcare professional for personalized advice.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): The NIDDK is a trusted source of information about various digestive conditions, including diverticulitis. Their website provides detailed information about symptoms, diagnosis, treatment, and management strategies.
- Patient Advocacy Groups: Numerous patient advocacy groups focus on specific health conditions, including diverticulitis. These groups often provide support, share experiences, and offer practical tips for managing the condition.
- Reputable Medical Journals: Medical journals offer research-based information about diverticulitis and related topics. However, it is crucial to critically evaluate the information and consult with a healthcare professional for personalized advice.
Wrap-Up: Diverticulitis Signs Symptoms And Complications
In summary, diverticulitis signs, symptoms, and complications require careful attention and a proactive approach. Early diagnosis and appropriate treatment are vital in mitigating potential complications and ensuring a smoother recovery. Understanding the various symptoms, treatment options, and preventive measures is crucial for individuals seeking to manage and prevent this digestive condition effectively. This guide aims to provide a clear roadmap for navigating the complexities of diverticulitis, empowering individuals with the knowledge they need to make informed decisions about their health.










