Staph infection vs MRSA sets the stage for a crucial discussion about bacterial infections. We’ll explore the differences between these two types of staph infections, delving into their symptoms, treatment, and the factors that contribute to their development. Understanding the nuances of staph infections, and the more dangerous MRSA, is essential for anyone looking to protect themselves and their loved ones.
This comprehensive guide provides a detailed comparison of staphylococcus aureus infections, including the common skin infections, pneumonia, and bloodstream infections. It also specifically explores the more problematic methicillin-resistant Staphylococcus aureus (MRSA), its resistance mechanisms, and its increased health impact. The differences in symptoms, treatment approaches, and diagnostic methods are Artikeld, emphasizing the importance of accurate identification and timely intervention.
We’ll also discuss prevention strategies, risk factors, and the potential complications of delayed or inadequate treatment.
Introduction to Staph Infections and MRSA
Staphylococcus aureus, commonly known as staph, is a type of bacteria commonly found on the skin and in the nasal passages of humans. While many staph infections are relatively harmless and resolve on their own, some strains can cause serious illness. Understanding the different types of staph infections, including the particularly problematic methicillin-resistant Staphylococcus aureus (MRSA), is crucial for effective prevention and treatment.Staph infections range from minor skin irritations to life-threatening conditions.
Recognizing the symptoms and seeking appropriate medical attention promptly is vital for managing these infections effectively. This understanding is essential for individuals and healthcare providers to effectively prevent and treat staph infections.
Types of Staph Infections
Staph bacteria can cause a variety of infections, impacting different parts of the body. Understanding the specific type of infection aids in appropriate diagnosis and treatment.
- Skin infections (e.g., boils, abscesses, impetigo): These are often localized infections, appearing as pus-filled lesions on the skin. Prompt treatment is key to prevent further spread and complications.
- Pneumonia: Staph pneumonia is a serious lung infection, often requiring hospitalization and aggressive antibiotic therapy. The infection can manifest with symptoms such as fever, cough, and difficulty breathing.
- Bloodstream infections (bacteremia): If staph bacteria enter the bloodstream, it can lead to a life-threatening condition known as sepsis. Rapid diagnosis and treatment are critical to prevent organ damage and death.
- Bone and joint infections (osteomyelitis): Staph bacteria can infect bones and joints, leading to severe pain, swelling, and potentially long-term complications. Prompt treatment is necessary to prevent permanent damage.
- Other infections: Staph infections can also affect other parts of the body, including the heart, brain, and urinary tract. These infections often necessitate intensive medical care.
Methicillin-Resistant Staphylococcus aureus (MRSA)
Methicillin-resistant Staphylococcus aureus (MRSA) is a strain of staph bacteria that has developed resistance to many commonly used antibiotics, including methicillin. This resistance significantly impacts treatment options and poses a significant public health concern.MRSA infections can range from mild skin infections to severe, life-threatening conditions. Its resistance to antibiotics necessitates the use of alternative, often more expensive and less effective, medications.
Antibiotic Resistance Mechanisms, Staph infection vs mrsa
Staph bacteria develop resistance to antibiotics through various mechanisms, including:
- Mutations in genes that encode antibiotic targets:
- These mutations can alter the structure of proteins that antibiotics interact with, making the antibiotics less effective.
- Production of enzymes that inactivate antibiotics:
- Certain bacteria produce enzymes that break down or modify antibiotics, rendering them ineffective.
- Efflux pumps that remove antibiotics from the bacterial cells:
- These pumps actively transport antibiotics out of the bacterial cells, preventing them from reaching their targets.
Prevalence and Public Health Impact
Staph infections, including MRSA, pose a significant public health burden globally. Factors such as healthcare settings, community spread, and personal hygiene play a role in the prevalence of these infections.
- Healthcare-associated MRSA (HA-MRSA): Hospitals and other healthcare facilities can serve as breeding grounds for HA-MRSA, often due to compromised immune systems and frequent exposure to medical devices. This can spread among patients and healthcare workers.
- Community-associated MRSA (CA-MRSA): CA-MRSA strains are prevalent in the community, affecting individuals with no known healthcare exposure. These strains are often more aggressive and can cause serious infections, especially in young adults.
The increasing prevalence of antibiotic resistance, particularly in MRSA, underscores the importance of responsible antibiotic use and the development of new strategies to combat these infections.
Comparing Staph Infections and MRSA
Staphylococcus aureus, commonly known as staph, is a bacteria frequently found on the skin and in the nose. While most staph infections are relatively harmless and easily treatable, some strains, like methicillin-resistant Staphylococcus aureus (MRSA), pose a greater health risk due to their resistance to common antibiotics. Understanding the differences between these infections is crucial for proper diagnosis and treatment.Distinguishing between staph infections and MRSA is vital for appropriate medical intervention.
Differences lie not only in the severity but also in the treatment approaches, emphasizing the need for accurate diagnosis. This comparison will delineate the symptomatic variations, treatment protocols, and diagnostic methodologies.
Symptoms of Staph and MRSA Infections
Staph infections often manifest as localized skin infections, like boils, pimples, or abscesses. These lesions can appear red, swollen, and painful, often with pus. In contrast, MRSA infections can also cause skin lesions but may exhibit more severe symptoms, including deeper tissue infections and potentially life-threatening complications like pneumonia or bloodstream infections. The severity of symptoms depends on the site of infection and the individual’s immune response.
Treatment Approaches for Staph and MRSA Infections
Treatment for staph infections usually involves topical antibiotics and drainage of abscesses. For less severe cases, oral antibiotics might be sufficient. However, MRSA infections require more aggressive treatment. Due to the resistance of MRSA to many common antibiotics, healthcare professionals typically prescribe specific antibiotics effective against this strain. Often, intravenous antibiotics are used for more severe cases.
Diagnostic Methods for Staph and MRSA Infections
Diagnosis often begins with a physical examination to identify the affected area and observe symptoms. Cultures of the infected site are crucial to identify the causative bacteria and determine whether it is staph or MRSA. Laboratory tests, like Gram stains, further help to differentiate between different types of bacteria. Molecular tests can also be used to confirm the presence of MRSA and determine its susceptibility to specific antibiotics.
Isolation and Culture of Staphylococcus and MRSA Strains
Proper isolation and culture techniques are vital to identify the specific bacterial strain causing the infection. These methods involve collecting samples from the infected area and culturing them in a controlled laboratory environment. Specific growth media and incubation conditions are used to promote the growth of the bacteria. Further testing can determine if the isolated strain is MRSA.
Antibiotics Used in Treating Staph and MRSA Infections
Various antibiotics are effective against staph infections, including penicillin-like antibiotics. However, MRSA resistance to these common antibiotics necessitates the use of alternative antibiotics, such as vancomycin, linezolid, or daptomycin. The choice of antibiotic depends on the severity of the infection, the patient’s overall health, and the specific MRSA strain. The precise antibiotic selection is often guided by susceptibility testing, which identifies the antibiotics that effectively target the specific MRSA strain.
Comparison Table
| Characteristic | Staph Infection | MRSA Infection |
|---|---|---|
| Incubation Period | Generally 2-5 days | Generally 2-5 days |
| Symptoms | Localized skin infections (boils, abscesses, pimples); redness, swelling, pain, pus | Similar to staph infections, but potential for more severe and disseminated infections (pneumonia, bloodstream infections); deeper tissue involvement, potentially more severe inflammation. |
| Treatment Options | Topical antibiotics, incision and drainage of abscesses, oral antibiotics | Specific antibiotics effective against MRSA (vancomycin, linezolid, daptomycin), potentially intravenous administration; often more aggressive and prolonged treatment. |
Risk Factors and Prevention
Staph infections and MRSA, while often treatable, can become serious health concerns if left untreated. Understanding the factors that increase risk and implementing preventative measures are crucial for reducing the incidence of these infections. This section delves into the specific risk factors and Artikels practical strategies for individuals and healthcare settings to mitigate the risk of acquiring and spreading these bacteria.
Factors Increasing Risk of Staph Infections
Several factors contribute to an individual’s susceptibility to staph infections and MRSA. These include compromised immune systems, chronic health conditions, and certain behaviors. A weakened immune response makes it harder for the body to fight off bacterial infections.
Factors Increasing Risk of MRSA
MRSA, a strain of Staphylococcus aureus resistant to many common antibiotics, poses a particular threat. The risk factors for MRSA often overlap with those for standard staph infections but also include specific factors like prolonged hospital stays, exposure to individuals with MRSA, and contact with contaminated surfaces.
While researching staph infection versus MRSA, I stumbled upon the fascinating topic of primary ovarian insufficiency. This condition, a potential cause of fertility issues, often goes undiagnosed. Understanding the complexities of staph infection vs MRSA requires careful consideration of potential underlying health conditions, like the ones associated with what is primary ovarian insufficiency. It’s important to remember that a thorough understanding of the nuances of each infection is crucial for appropriate treatment and management.
Prevention Strategies for Individuals
Maintaining good hygiene is fundamental in preventing staph infections and MRSA. Regular handwashing with soap and water, particularly after using the restroom, touching animals, or being in public areas, is crucial. Avoiding sharing personal items like towels, razors, and clothing can also significantly reduce the risk of transmission. Maintaining proper wound care is vital to prevent infection, including keeping wounds clean and covered.
Individuals with open wounds or skin conditions should take extra precautions to avoid contamination.
Ever wondered about the difference between staph and MRSA infections? It’s a serious topic, and while I’m no doctor, I’ve learned that a balanced diet plays a crucial role in overall health, impacting your body’s ability to fight off infections. For example, what happens to your body when you eat a protein bar every day could potentially affect your immune system, potentially making you more susceptible to infections like staph or MRSA.
Understanding how your daily choices impact your well-being is key to staying healthy.
Preventative Measures for Healthcare Workers
Healthcare workers are at a higher risk due to frequent exposure to patients and potentially contaminated environments. Strict adherence to hand hygiene protocols, appropriate use of personal protective equipment (PPE), and proper sterilization of equipment are essential. Training on recognizing and isolating potential cases of MRSA is critical to preventing outbreaks. Healthcare facilities should implement stringent infection control protocols and maintain meticulous hygiene standards to safeguard staff and patients.
Preventative Measures for Athletes
Athletes, particularly those participating in contact sports, are susceptible to skin infections. Proper hygiene, including regular showering and thorough handwashing after practice or competition, is important. Maintaining clean athletic equipment and ensuring that wounds are properly treated and covered can prevent contamination. Using protective gear during contact sports can reduce the risk of skin injuries that could become infected.
Hygiene Practices for Preventing Spread
Maintaining good hygiene practices is paramount in preventing the spread of both staph and MRSA. Regular handwashing, the proper use of disinfectants, and careful handling of contaminated items are key to reducing transmission. Practicing meticulous hygiene in shared spaces and environments like gyms, locker rooms, and communal areas is essential to minimize the risk of infection.
Preventing Spread in Healthcare Settings
Healthcare facilities should implement rigorous infection control protocols. This includes thorough cleaning and disinfection of surfaces, proper disposal of contaminated materials, and prompt isolation of individuals with suspected infections. Strict adherence to protocols by all staff, including hand hygiene practices and the use of appropriate PPE, is critical. Regular audits and evaluations of infection control measures are vital for continuous improvement.
Importance of Proper Wound Care
Proper wound care is essential in preventing staph and MRSA infections. Cleaning wounds thoroughly, using appropriate dressings, and keeping the area clean and dry are crucial steps. Prompt medical attention for any wound that shows signs of infection is essential. Prompt and appropriate treatment of any injuries or wounds will minimize the risk of complications and infection.
Table of Risk Factors and Severity
| Risk Factor | Severity | Explanation |
|---|---|---|
| Compromised Immune System | High | Weakened immune response makes the body less able to fight off infections. |
| Chronic Health Conditions (e.g., diabetes, HIV) | Medium | Chronic conditions can impair healing and increase susceptibility. |
| Prolonged Hospital Stays | High | Increased exposure to contaminated environments and weakened immune response. |
| Sharing Personal Items | Low | Increased risk of direct transmission through contact. |
| Poor Hygiene Practices | Medium | Lack of handwashing and other hygiene practices increases risk of infection. |
Diagnosis and Treatment: Staph Infection Vs Mrsa
Identifying and treating staph infections and MRSA requires a precise approach. Accurate diagnosis is crucial for selecting the appropriate treatment and preventing complications. Different diagnostic tools and treatment protocols exist, reflecting the varying severity and nature of the infections.
Diagnostic Procedures
Staphylococcus aureus (staph) and methicillin-resistant Staphylococcus aureus (MRSA) infections are diagnosed through a combination of clinical evaluation and laboratory tests. A healthcare professional will consider the patient’s symptoms, medical history, and the site of infection. Physical examination helps pinpoint the location and extent of the infection.
- Culture and Sensitivity Testing: A crucial step in diagnosis involves obtaining a sample from the infected site. This sample is cultured in a laboratory to identify the presence of staph or MRSA. Sensitivity testing determines which antibiotics are effective against the specific strain. This targeted approach minimizes the risk of ineffective treatment.
- Imaging Studies: X-rays, CT scans, or MRIs might be used to visualize the infection site and assess its extent, especially for deeper infections like those in the bones or joints. This can help determine the appropriate treatment strategy.
- Complete Blood Count (CBC): A CBC can reveal signs of inflammation or infection in the body, aiding in the diagnosis and monitoring of the infection’s progression. Elevated white blood cell counts, for example, suggest an active infection.
Treatment Protocols
Treatment for staph and MRSA infections varies depending on the severity and location of the infection. Early intervention is key to minimizing complications and ensuring a successful recovery.
- Staphylococcus aureus (Staph) Infections: Often, mild staph infections respond well to topical treatments and oral antibiotics, such as penicillin-based drugs. More severe infections may require intravenous antibiotics, administered directly into a vein. The choice of antibiotic is determined by the results of the sensitivity test.
- Methicillin-Resistant Staphylococcus aureus (MRSA) Infections: MRSA infections often require stronger antibiotics, sometimes multiple drugs, and longer treatment durations. Healthcare professionals carefully consider the patient’s history, the severity of the infection, and the results of sensitivity tests when selecting the appropriate antibiotics.
Role of Antibiotics
Antibiotics play a vital role in combating staph and MRSA infections by killing or inhibiting the growth of bacteria. However, overuse and inappropriate use can lead to antibiotic resistance.
“Appropriate antibiotic selection is crucial for effective treatment and preventing the development of resistant strains.”
- Antibiotic Selection: Choosing the correct antibiotic is based on the results of the culture and sensitivity tests. This ensures the drug is effective against the specific bacteria causing the infection. Overuse or misuse of antibiotics can lead to the development of antibiotic-resistant bacteria, which can pose a significant health challenge in the future.
- Duration of Treatment: The duration of antibiotic treatment is determined by the severity of the infection and the patient’s response to treatment. Completing the full course of antibiotics as prescribed is essential for eradicating the infection and preventing recurrence.
Importance of Following Treatment
Adherence to the prescribed treatment plan is essential for successful outcomes. Skipping doses or prematurely stopping treatment can lead to the infection persisting or worsening.
Ever wondered about staph infection versus MRSA? It’s a tricky comparison, and sometimes, pushing your body to its limits, like running in the cold weather here , can actually make you more susceptible. Understanding the different factors involved in both infections is crucial for staying healthy, especially during challenging activities. Knowing the risks helps you make informed decisions about your health and safety, making staph infection vs MRSA less of a mystery.
- Adherence to Treatment: Taking antibiotics as directed, including the frequency and duration, is crucial. Regular follow-up appointments allow healthcare professionals to monitor the patient’s progress and adjust the treatment plan as needed.
- Monitoring Symptoms: Close monitoring of symptoms during treatment is essential. If symptoms worsen or new symptoms emerge, contacting a healthcare professional promptly is important.
Step-by-Step Guide to Managing a Staph Infection
A step-by-step guide to managing a staph infection includes prompt medical attention, adherence to treatment, and proper hygiene practices.
- Seek immediate medical attention if you suspect a staph infection.
- Follow the prescribed antibiotic treatment regimen diligently.
- Practice good hygiene to prevent the spread of infection.
- Report any worsening symptoms to your healthcare provider.
Potential Complications of Delayed or Inadequate Treatment
Delayed or inadequate treatment of staph and MRSA infections can lead to several complications.
- Sepsis: A life-threatening condition where the body’s response to infection spirals out of control.
- Abscess Formation: Pus-filled pockets of infection that require surgical drainage.
- Bone or Joint Infections (Osteomyelitis): Serious infections that can lead to permanent damage.
- Spread of Infection: The infection can spread to other parts of the body.
Flowchart of Diagnosis and Treatment
[A flowchart illustrating the diagnosis and treatment process would be visually represented here, but I am unable to create visual content.]
Complications and Long-Term Effects
Staph infections and, particularly, MRSA, can lead to a range of complications, some of which can significantly impact a person’s quality of life. Understanding these potential outcomes is crucial for proactive management and timely intervention. Untreated or inadequately treated infections can have lasting consequences, necessitating vigilance and prompt medical attention.While most staph infections resolve with appropriate treatment, some individuals may experience more severe complications, including those affecting various organs and systems.
These complications can range from localized skin issues to life-threatening systemic conditions. The severity of these complications depends on several factors, including the type of infection, the individual’s overall health, and the promptness and effectiveness of treatment.
Potential Complications of Staph Infections
Staph infections, if left untreated or improperly managed, can lead to various complications, ranging from localized skin problems to more severe systemic issues. The potential complications can impact different body systems, leading to significant health consequences.
- Skin and Soft Tissue Infections: Abscesses, cellulitis, and impetigo are common skin and soft tissue infections caused by staph. These infections can spread, causing deeper tissue damage and requiring surgical intervention. Prompt treatment is essential to prevent the spread and to avoid more severe complications.
- Sepsis: In severe cases, staph infections can progress to sepsis, a life-threatening condition where the body’s response to infection causes damage to its own tissues and organs. Early diagnosis and aggressive treatment are crucial for managing sepsis effectively.
- Endocarditis: Staphylococcus aureus can infect the inner lining of the heart (endocardium), leading to endocarditis. This can cause heart valve damage and potentially life-threatening complications.
- Osteomyelitis: Bone infection (osteomyelitis) can result from staph spreading to the bones. This can cause severe pain, swelling, and potential bone damage, requiring extensive treatment and potentially long-term rehabilitation.
- Pneumonia: Staphylococcus can cause pneumonia, an infection of the lungs, especially in individuals with weakened immune systems. This can cause significant respiratory distress and require hospitalization.
Long-Term Effects of Untreated or Inadequately Treated Infections
Untreated or inadequately treated staph and MRSA infections can lead to lasting consequences, requiring ongoing medical care and impacting daily life. The specific long-term effects depend on the severity and location of the infection.
- Chronic Pain and Discomfort: Localized infections, particularly those in joints or bones, can result in chronic pain and discomfort, limiting mobility and daily activities. Rehabilitation and pain management strategies are often necessary to improve quality of life.
- Scarring and Disfigurement: Deep skin infections can lead to significant scarring and disfigurement, impacting self-esteem and requiring reconstructive procedures in some cases. Appropriate wound care and monitoring are crucial to minimizing scarring.
- Physical Disability: In severe cases, complications like osteomyelitis or joint infections can lead to permanent physical disability, impacting mobility and independence. Early diagnosis and intervention are vital to mitigate potential long-term effects.
- Weakened Immune System: Severe infections can compromise the immune system, making the individual more susceptible to future infections and other health problems.
- Increased Risk of Recurrence: Individuals with a history of staph infections may have a higher risk of recurrence. Continued vigilance and preventive measures are necessary to avoid further infections.
Importance of Seeking Medical Attention
Prompt medical attention is essential for managing staph and MRSA infections effectively and minimizing the risk of complications. Persistent symptoms, even seemingly minor ones, should not be ignored. Seeking professional medical advice allows for early diagnosis and treatment, which is crucial for preventing the progression to more severe outcomes. Delaying treatment can worsen the infection and increase the likelihood of long-term consequences.
Managing Long-Term Effects
Managing long-term effects often requires a multidisciplinary approach, involving healthcare professionals specializing in various fields. Rehabilitation, physical therapy, and psychological support may be necessary to address the physical and emotional impact of complications.
- Regular Follow-up Care: Maintaining regular follow-up appointments with healthcare providers is essential for monitoring the condition and adjusting treatment plans as needed.
- Physical Therapy: Physical therapy can help improve mobility and function for individuals with chronic pain or limited movement due to complications.
- Support Groups: Support groups can provide valuable emotional support and practical advice for individuals and their families coping with long-term effects of staph or MRSA infections.
- Psychological Support: Addressing the emotional and psychological impact of infections and complications through counseling or therapy is important for well-being.
Staph Infection vs. MRSA
Staphylococcus aureus, commonly known as staph, is a bacteria often found on the skin and in the nose. While many staph infections are harmless and resolve on their own, some can lead to more serious complications. Methicillin-resistant Staphylococcus aureus (MRSA) is a type of staph that’s resistant to many common antibiotics, making treatment more challenging. Understanding the differences between typical staph infections and MRSA is crucial for effective diagnosis and management.
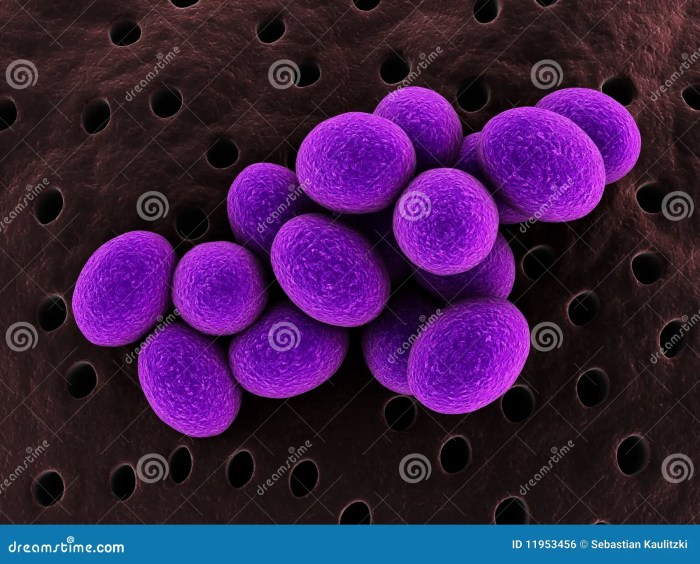
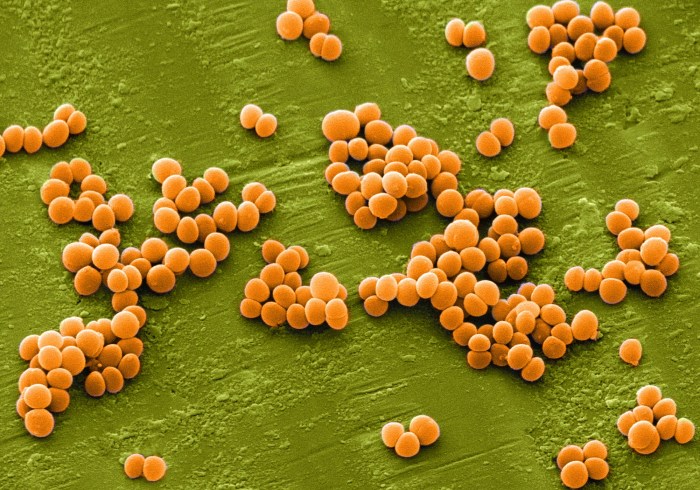
Visual Representation of Differences
Visual representation can greatly assist in distinguishing between typical staph and MRSA infections. A typical staph infection might manifest as a localized, red, swollen area on the skin, potentially with pus. MRSA infections, however, may exhibit similar initial symptoms, but can progress more aggressively, potentially forming larger, deeper lesions, or abscesses, and possibly exhibiting more severe inflammation. The progression of symptoms and the response to treatment can also differ significantly.
Symptom Comparison
The following table illustrates the potential symptom differences between staph and MRSA infections:
| Symptom | Typical Staph Infection | MRSA Infection |
|---|---|---|
| Initial Lesion | Small, red, localized swelling; often with pus | Similar to staph initially, but may progress to larger, deeper lesions, abscesses, or more severe inflammation |
| Pain | Localized pain, often mild to moderate | Pain may be more intense and persistent, especially with deeper infections |
| Redness | Localized redness around the infection site | Redness may be more extensive and intense |
| Pus | May produce pus | May produce pus, but may not always be present |
| Temperature | May or may not cause fever | Fever may be more common, especially with more severe infections |
Treatment Protocol Differences
The choice of treatment depends largely on the type of infection. Typical staph infections often respond well to topical or oral antibiotics, whereas MRSA infections necessitate different, often stronger antibiotics, as well as a longer treatment course. Specific antibiotics chosen are crucial for successful treatment. The image below graphically depicts this difference. Imagine a flowchart; one branch for staph, showing topical creams or oral antibiotics, and a separate, more complex branch for MRSA, indicating the need for intravenous antibiotics and potentially surgical intervention.
Bacterial Structural Differences
Staphylococcus aureus and MRSA differ in their cell walls. Staph bacteria possess a cell wall that makes them susceptible to certain antibiotics. MRSA, however, has developed resistance mechanisms that prevent these antibiotics from effectively targeting and killing the bacteria. This resistance stems from specific genetic mutations, which alters the structure of the cell wall, making it impermeable to the action of certain antibiotics.
Bacterial Growth Cycle and Resistance Development
The growth cycle of staph bacteria involves various stages, from initial replication to forming colonies. When exposed to antibiotics, some staph bacteria may develop resistance by mutating their genes. This alteration renders the antibiotic ineffective. Over time, these resistant bacteria multiply, leading to a population primarily comprised of resistant strains. This is a key factor in the development of MRSA.
For instance, improper antibiotic use or inadequate treatment duration can accelerate the selection and spread of resistant strains. The illustration of this process would depict bacteria multiplying and those resistant to a particular antibiotic surviving and reproducing, leading to a population shift towards resistance.
Outcome Summary
In conclusion, understanding the distinctions between staph infections and MRSA is paramount. While staph infections are generally treatable, MRSA’s antibiotic resistance poses a significant challenge. This discussion highlighted the importance of proper hygiene, prompt medical attention, and understanding risk factors to prevent and effectively manage these infections. By grasping the core differences and preventative measures, we can collectively safeguard public health and improve treatment outcomes.









