Postural orthostatic tachycardia syndrome pots – Postural orthostatic tachycardia syndrome (POTS) is a complex condition that significantly impacts daily life. This in-depth look explores the intricacies of POTS, from its definition and symptoms to diagnosis, management, and the latest research. We’ll examine the diverse ways POTS manifests, impacting individuals differently, and the challenges they face. Understanding this condition is crucial for supporting those affected and fostering better awareness.
POTS is characterized by a rapid increase in heart rate when standing up from a seated or lying position. This often leads to a range of symptoms, including dizziness, lightheadedness, fatigue, and nausea. The condition can significantly impact daily activities, making simple tasks feel overwhelming. Learning about POTS, including its triggers, and various management strategies, is key to empowering those living with this often-misunderstood condition.
Defining Postural Orthostatic Tachycardia Syndrome (POTS)
Postural Orthostatic Tachycardia Syndrome (POTS) is a chronic condition characterized by an exaggerated increase in heart rate when transitioning from a lying or sitting position to a standing position. This rapid heart rate response, often accompanied by other symptoms, significantly impacts daily life. Understanding POTS involves delving into its underlying mechanisms, diagnostic criteria, and how it differs from other conditions.POTS occurs due to an imbalance in the autonomic nervous system, which regulates involuntary bodily functions like heart rate and blood pressure.
In individuals with POTS, the system’s ability to maintain adequate blood flow and blood pressure during postural changes is impaired. This results in the heart beating faster to compensate for the drop in blood pressure that occurs when standing up, leading to the characteristic symptoms.
Pathophysiology of POTS
The autonomic nervous system, composed of the sympathetic and parasympathetic branches, plays a crucial role in regulating cardiovascular function. In POTS, the sympathetic nervous system, responsible for increasing heart rate and blood pressure, is overactive, leading to the rapid heart rate response. This overactivation can be due to various factors, including impaired baroreceptor function, a reduced blood volume, or an imbalance in the neurotransmitters that control these systems.
Furthermore, there may be abnormalities in the vascular system, making blood vessels less responsive to pressure changes.
Types of POTS
While a definitive classification of POTS subtypes is still evolving, some researchers propose differentiating based on the presence of other symptoms or contributing factors. This could include POTS associated with other conditions, such as Ehlers-Danlos syndrome, mast cell activation syndrome, or specific genetic predispositions. However, the current diagnostic approach focuses on the core symptoms and response to postural changes, rather than distinct types.
Diagnostic Criteria for POTS
Diagnosis of POTS typically involves a combination of patient history, physical examination, and specific diagnostic tests. A key element is documenting a significant increase in heart rate (at least 30 bpm) within 10 minutes of standing up from a supine or seated position. This response, coupled with symptoms like dizziness, lightheadedness, and fatigue, can help clinicians differentiate POTS from other conditions.
Clinicians may also utilize tilt-table testing to assess the body’s response to postural changes, providing objective data on the heart rate response.
Comparison to Other Conditions
| Condition | Key Characteristics | Distinguishing Factors |
|---|---|---|
| Postural Orthostatic Tachycardia Syndrome (POTS) | Exaggerated heart rate increase with standing, dizziness, lightheadedness, fatigue | Specific heart rate response to postural change, often associated with autonomic dysfunction. |
| Anxiety | Excessive worry, nervousness, rapid heartbeat, sweating | POTS typically has a more pronounced postural response, and symptoms are often more persistent and linked to autonomic dysfunction. |
| Anemia | Low red blood cell count, fatigue, shortness of breath, pallor | Anemia presents with a broader range of symptoms, and the postural response is not the defining feature. |
This table highlights key distinctions between POTS and similar conditions. Careful consideration of symptoms and diagnostic testing are crucial for accurate diagnosis. The postural response, coupled with autonomic dysfunction, is a key distinguishing feature of POTS.
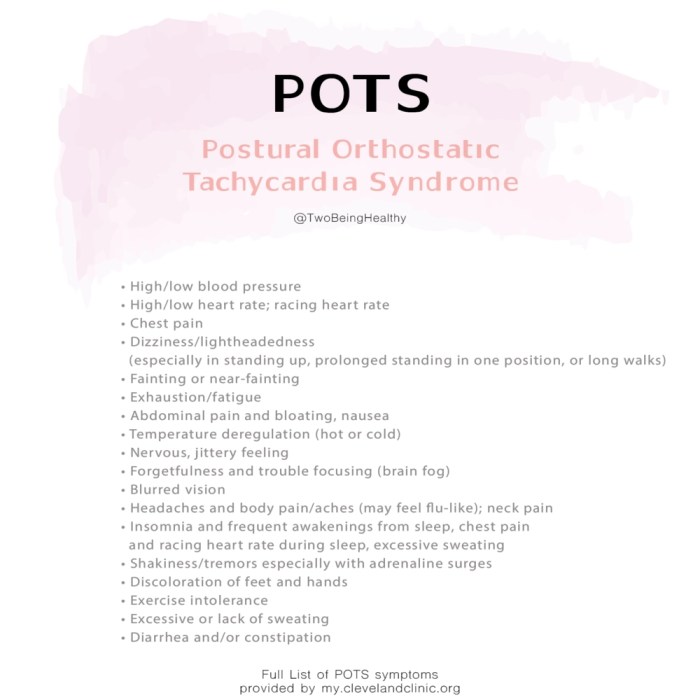
Symptoms and Manifestations
Living with Postural Orthostatic Tachycardia Syndrome (POTS) can be challenging due to its diverse and often unpredictable symptoms. Understanding the spectrum of these symptoms is crucial for effective self-management and seeking appropriate medical care. Recognizing patterns and triggers can help individuals with POTS better navigate their daily lives.The symptoms of POTS can vary significantly from person to person, making diagnosis and management sometimes difficult.
Dealing with Postural Orthostatic Tachycardia Syndrome (POTS) can be tough, and understanding the different types of joint pain is also important. For example, if you’re experiencing pain related to arthritis, it’s crucial to differentiate between osteoarthritis and rheumatoid arthritis. Knowing the difference can help you find the right treatment, as outlined in this helpful resource about osteoarthritis vs rheumatoid arthritis.
This knowledge, in turn, can better inform your POTS management strategy, as joint pain can significantly impact overall well-being.
While some individuals experience mild symptoms that only affect their daily activities, others experience severe symptoms that significantly impact their quality of life. This variability emphasizes the importance of personalized approaches to diagnosis and treatment.
Common Symptoms
The hallmark symptom of POTS is a rapid increase in heart rate (tachycardia) when standing up from a sitting or lying position. This response is exaggerated compared to healthy individuals, and is often accompanied by other symptoms. Many individuals with POTS experience a combination of symptoms, which can change over time and vary in severity.
Variability of Symptoms
Symptoms can manifest in diverse ways, influencing different aspects of daily life. Some individuals may primarily experience dizziness and lightheadedness, while others might have more pronounced fatigue and cognitive difficulties. The variability also includes the intensity and duration of the symptoms. Some individuals might experience short-lived symptoms, while others might experience prolonged episodes. Understanding these variations is key to developing individualized strategies for managing POTS.
Frequency and Severity of Symptoms (Table)
| Symptom | Frequency (Percentage of POTS Patients) | Severity (Mild/Moderate/Severe) |
|---|---|---|
| Orthostatic tachycardia | 90-95% | Moderate to Severe |
| Lightheadedness/Dizziness | 80-90% | Mild to Moderate |
| Fatigue | 70-80% | Moderate to Severe |
| Headache | 60-70% | Mild to Moderate |
| Nausea | 50-60% | Mild to Moderate |
| Blurry vision | 40-50% | Mild to Moderate |
| Abdominal pain | 30-40% | Mild to Moderate |
| Palpitations | 30-40% | Mild to Moderate |
Note: This table provides a general overview and individual experiences may vary.
Long-Term Effects on Daily Life
The long-term effects of POTS can significantly impact daily activities. Individuals may experience limitations in their ability to participate in work, school, social activities, and exercise. The impact can extend to reduced productivity, decreased quality of life, and increased reliance on others for support. These impacts can affect emotional well-being and mental health.
Triggers for POTS Symptoms (Table)
| Trigger | Description |
|---|---|
| Dehydration | Reduced fluid intake can worsen POTS symptoms. |
| Heat Exposure | High temperatures can exacerbate symptoms. |
| Standing for Prolonged Periods | Maintaining an upright position for extended durations often triggers symptoms. |
| Sudden Position Changes | Rapid shifts from lying to standing can cause immediate symptoms. |
| Stress | Emotional stress can significantly worsen POTS symptoms. |
| Exercise | Physical activity, even moderate exercise, can sometimes trigger symptoms. |
| Food Intolerances | Certain foods can exacerbate symptoms in some individuals. |
Note: This is not an exhaustive list, and individual triggers may vary.
Diagnosis and Evaluation
Navigating the path to a POTS diagnosis can feel like a maze, but understanding the process is crucial for effective management. A thorough evaluation combines a detailed medical history, physical examination, and various diagnostic tests to pinpoint the specific cause and severity of symptoms. This multifaceted approach allows healthcare professionals to tailor treatment plans to individual needs.The diagnostic journey for POTS hinges on careful consideration of the patient’s symptoms, medical history, and physical examination findings.
Blood tests and specific postural testing provide valuable data to support the diagnosis. The core objective is to confirm the characteristic heart rate response to postural changes. This process, when done correctly, aids in differentiating POTS from other conditions that share similar symptoms.
Medical History
A comprehensive medical history is fundamental to diagnosing POTS. The clinician meticulously gathers information about the onset, duration, and frequency of symptoms. This includes details about triggers (e.g., stress, dehydration, or specific activities) and associated symptoms (e.g., dizziness, fatigue, or abdominal pain). A detailed history of past illnesses, medications, and family history of similar conditions further enhances the diagnostic process.
Dealing with Postural Orthostatic Tachycardia Syndrome (POTS) can be tough, especially when everyday tasks become challenging. For example, some people with POTS also experience difficulties with showering, similar to those with chronic fatigue syndrome, as detailed in this informative article on problems showering chronic fatigue syndrome. The dizziness and lightheadedness associated with POTS can make even simple activities like getting in and out of the shower potentially dangerous.
Fortunately, there are strategies to manage these issues, and understanding the specific challenges can be key to improving your quality of life with POTS.
This historical context is crucial in differentiating POTS from other conditions with overlapping symptoms.
Physical Examination
The physical examination is a vital part of the evaluation. It involves assessing vital signs, including blood pressure and heart rate in both supine (lying down) and standing positions. The clinician also evaluates for other relevant symptoms such as postural dizziness, orthostatic hypotension, or signs of autonomic dysfunction. The examination aims to identify any physical characteristics that might suggest a contributing factor to POTS or other underlying conditions.
Blood Tests and Other Diagnostic Tools
Blood tests are frequently used to rule out other potential conditions. These tests can help evaluate for anemia, thyroid dysfunction, or infections that might mimic POTS symptoms. Electrocardiograms (ECGs) and other cardiac assessments help exclude structural heart abnormalities or other cardiac conditions. These tests, when combined with the medical history and physical examination, provide a comprehensive picture of the patient’s overall health.
Postural Assessment
Monitoring the heart rate response to changes in posture is crucial in diagnosing POTS. The standard protocol involves measuring heart rate in a supine position, followed by a period of standing. The increase in heart rate (typically exceeding 30 beats per minute) in response to standing, coupled with other symptoms, strongly suggests POTS. This precise monitoring is key to confirming the presence of POTS.
Diagnostic Tests and Implications
| Diagnostic Test | Implications |
|---|---|
| Medical History Review | Provides context for symptoms, identifies potential triggers, and rules out other conditions. |
| Physical Examination | Evaluates vital signs, identifies physical characteristics, and assesses for associated symptoms. |
| Blood Tests (CBC, Thyroid Function, etc.) | Excludes other potential conditions that may mimic POTS symptoms. |
| Electrocardiogram (ECG) | Rules out structural heart abnormalities or other cardiac conditions. |
| Postural Assessment (Standing Test) | Evaluates heart rate response to postural changes, providing a key indicator for POTS. A significant increase in heart rate upon standing, often exceeding 30 bpm, supports the diagnosis. |
Management and Treatment
Navigating Postural Orthostatic Tachycardia Syndrome (POTS) often feels like a maze. Finding the right path to relief involves understanding the diverse strategies available and tailoring a plan that works best for your individual needs. This often requires a combination of lifestyle adjustments, medication, and potentially, therapies.
Lifestyle Modifications
Lifestyle modifications play a crucial role in managing POTS symptoms. These adjustments, often simple yet powerful, can significantly impact overall well-being and symptom severity. A personalized approach is key, recognizing that what works for one person might not be as effective for another.
- Hydration is paramount. Adequate fluid intake, especially water, is essential to maintain blood volume and support circulatory function. Carrying a water bottle and setting reminders can help ensure consistent hydration throughout the day. Aim for specific fluid intake recommendations based on individual needs, often tailored by healthcare professionals.
- Dietary strategies can also be helpful. A balanced diet, rich in nutrients and electrolytes, can support overall health and counteract potential imbalances. Specific dietary considerations might include increasing salt intake to maintain blood volume, particularly if recommended by a doctor.
- Gradual movements are recommended. Avoid sudden changes in posture. Rising slowly, taking breaks, and avoiding prolonged standing can significantly mitigate symptoms. Incorporating frequent rest periods into daily routines is often necessary.
- Stress management is important. Stress can exacerbate POTS symptoms. Practices like mindfulness, meditation, and deep breathing exercises can help manage stress levels and improve overall well-being.
- Sleep hygiene is crucial. Prioritizing quality sleep helps the body recover and function optimally. Establishing a consistent sleep schedule and creating a relaxing bedtime routine can greatly improve sleep quality.
Medication
Medication plays a significant role in treating POTS, often acting as a supplementary approach to lifestyle modifications. The specific medications and dosages will depend on the individual’s specific needs and symptoms.
- Medications like fludrocortisone acetate can help maintain blood volume and blood pressure. This medication works by promoting sodium retention and influencing blood vessel function. Careful monitoring is crucial to ensure appropriate dosage and prevent potential side effects.
- Beta-blockers, sometimes used in POTS management, help slow the heart rate and reduce the rapid heart rate response that occurs when standing. This can improve symptoms like lightheadedness and dizziness.
- Other medications may be prescribed to address specific symptoms. These may include treatments for anxiety or other co-occurring conditions that can impact POTS.
Therapeutic Approaches
Several therapeutic approaches can support POTS management. These strategies aim to improve overall well-being and address the underlying mechanisms of the syndrome.
- Physical therapy can be highly beneficial. Exercises tailored to improve cardiovascular fitness and posture can help enhance circulation and mitigate symptoms.
- Cognitive behavioral therapy (CBT) can help manage the psychological impact of living with POTS. This therapy can address anxiety and related issues, which can influence symptoms.
- Education and support groups are crucial for understanding the condition and managing it effectively. These resources provide valuable insights, practical tips, and a sense of community.
Summary of Treatment Options
| Treatment Option | Description | Effectiveness |
|---|---|---|
| Lifestyle Modifications | Dietary changes, hydration, gradual movements, stress management, sleep hygiene | Generally effective for symptom management, often a cornerstone of treatment |
| Medications | Fludrocortisone, beta-blockers, others | Can effectively reduce symptoms like tachycardia and dizziness, but individual responses vary |
| Physical Therapy | Exercises to improve circulation and posture | Helpful for improving cardiovascular fitness and managing symptoms |
| Cognitive Behavioral Therapy (CBT) | Addressing psychological impact of POTS | Can help manage anxiety and stress, leading to symptom reduction |
Impact on Daily Life
Living with Postural Orthostatic Tachycardia Syndrome (POTS) significantly impacts daily life, affecting everything from simple tasks to complex social interactions. The fluctuating symptoms, including dizziness, fatigue, and rapid heart rate, can make even routine activities feel challenging. Understanding these effects is crucial for developing effective coping strategies and seeking appropriate support.The unpredictable nature of POTS symptoms can lead to feelings of frustration, anxiety, and isolation.
This can have a profound impact on mental well-being, making it important to address both the physical and emotional aspects of the condition. Strategies for self-management and support networks become essential tools in navigating the challenges of daily life with POTS.
Impact on Daily Activities
Managing everyday tasks can be a significant struggle for individuals with POTS. Simple activities like walking, standing, or even sitting for prolonged periods can trigger symptoms. This can lead to limitations in participation in various activities, impacting social interactions, work, and school performance. Individuals may experience a reduction in physical endurance and stamina, affecting their ability to engage in activities they once enjoyed.
Impact on Social Interactions
Social situations can be challenging for people with POTS. The unpredictable nature of symptoms can lead to feelings of anxiety and self-consciousness. Concerns about triggering symptoms or appearing unwell can impact social interactions and potentially lead to feelings of isolation. Many individuals with POTS report difficulty maintaining friendships and romantic relationships due to the fluctuating symptoms and limitations in physical activity.
Impact on Work and School, Postural orthostatic tachycardia syndrome pots
POTS can significantly affect work and school performance. The unpredictable nature of symptoms can make it difficult to maintain consistent attendance, focus, and productivity. Missed work or school days, as well as decreased cognitive function, can lead to performance issues and difficulties in keeping up with academic or professional demands. Employers and educational institutions may require adjustments to accommodate the needs of individuals with POTS.
Examples include flexible work schedules, modified assignments, or accessible work environments.
Impact on Relationships
Relationships with family and friends can be strained by the challenges of living with POTS. The unpredictable nature of symptoms, along with the need for adjustments in daily routines, can place stress on relationships. It’s crucial for individuals with POTS and their loved ones to communicate openly and understand the condition. Open communication and support are key for maintaining healthy relationships.
Dealing with postural orthostatic tachycardia syndrome (POTS) can be tough, especially when you’re trying to pinpoint the cause of your symptoms. Sometimes, seemingly unrelated factors can play a role, like reactions to common household items. For instance, laundry detergent allergies can manifest in ways that mimic POTS symptoms, so understanding the signs and treatment options for such allergies is crucial.
Checking out this resource on laundry detergent allergies signs symptoms and treatment might help you identify if this could be contributing to your POTS experience. Ultimately, a thorough understanding of your triggers is key to effectively managing POTS.
Importance of Self-Management Strategies
Self-management strategies are crucial for individuals with POTS to maintain a good quality of life. These strategies involve proactive steps to manage symptoms, prevent triggers, and improve overall well-being. Developing personalized routines and strategies to address specific needs is essential. Examples include hydration, pacing activities, and stress management techniques. Utilizing a combination of approaches, including medication, lifestyle adjustments, and support systems, allows for effective self-management.
Common Daily Challenges
| Category | Common Daily Challenges |
|---|---|
| Physical | Fatigue, dizziness, lightheadedness, orthostatic intolerance, rapid heart rate, chest pain, headaches, nausea, abdominal pain, and difficulty concentrating. |
| Emotional | Anxiety, depression, frustration, feelings of isolation, low self-esteem, and difficulty managing social interactions. |
| Practical | Missed work or school days, difficulty with daily tasks, need for accommodations, limitations in physical activity, and difficulty traveling. |
Research and Future Directions: Postural Orthostatic Tachycardia Syndrome Pots
Understanding Postural Orthostatic Tachycardia Syndrome (POTS) is crucial for developing effective treatments and improving the lives of those affected. Current research is actively exploring various avenues to enhance diagnostic accuracy, refine therapeutic approaches, and ultimately, find a cure for this complex condition.
Current Research Areas
Researchers are focusing on several key areas to advance our understanding of POTS. These investigations involve examining the underlying mechanisms of autonomic dysfunction, identifying specific biomarkers for early detection, and exploring novel therapeutic strategies.
Promising Research Directions for Diagnosis
The quest for improved diagnostic tools is a high priority. Researchers are investigating non-invasive techniques that can accurately identify POTS patients early in the course of the illness. This includes exploring new blood markers that may reflect the underlying pathophysiological mechanisms. These biomarkers could provide a more objective assessment, reducing reliance on subjective symptoms, potentially leading to earlier intervention and better management.
Promising Research Directions for Treatment
Several promising avenues are being explored for improving POTS treatment. These approaches range from addressing the autonomic nervous system dysfunction to exploring therapies targeting the underlying pathophysiology of the condition. Some approaches focus on medications to modulate autonomic function, while others investigate novel therapies like targeted immune interventions. The long-term goal is to develop personalized treatment plans that address the unique needs of each patient.
Knowledge Gaps in Understanding POTS
Despite significant advancements, several knowledge gaps persist in our understanding of POTS. These include a lack of definitive biomarkers, the varying severity of the condition, and the complex interplay of genetic and environmental factors. Further research into the precise mechanisms underlying autonomic dysfunction and the identification of individual risk factors are needed to develop more effective interventions.
Potential for New Therapeutic Approaches
The potential for novel therapeutic approaches is substantial. The development of new medications that directly target specific aspects of autonomic dysfunction holds significant promise. Furthermore, advancements in gene therapy and regenerative medicine offer potential avenues for treating the root cause of POTS. These approaches, while still in the early stages, could revolutionize POTS treatment in the future.
Recent Breakthroughs in POTS Research (Summary Table)
| Research Area | Breakthrough Description | Significance |
|---|---|---|
| Biomarker Identification | Researchers have identified several potential blood markers that correlate with POTS severity, opening doors for earlier and more precise diagnosis. | Improved diagnostic accuracy allows for earlier intervention and personalized treatment plans. |
| Autonomic Dysfunction Mechanisms | Studies have revealed specific neural pathways and neurotransmitters involved in the autonomic dysfunction characteristic of POTS. | This knowledge provides insights into the disease’s pathophysiology, facilitating the development of targeted therapies. |
| Therapeutic Targeting | Initial trials of novel medications aimed at modulating the autonomic nervous system show promising results in reducing symptoms in some patients. | These findings suggest the potential for more effective and tailored treatments. |
Illustrative Examples
Understanding POTS requires more than just definitions and diagnoses. Real-life experiences offer invaluable insights into the challenges and triumphs of living with this condition. These examples demonstrate the variability of POTS, highlighting the diverse ways it impacts daily life and the range of management strategies that can be employed.
Hypothetical Case Study: Sarah’s Journey
Sarah, a 25-year-old woman, experiences debilitating POTS symptoms. Her symptoms typically begin within minutes of standing and include rapid heart rate, lightheadedness, and nausea. These symptoms often lead to fainting spells, especially when transitioning from sitting to standing. She frequently experiences fatigue, impacting her ability to participate in everyday activities.
Treatment Strategies in Action
Sarah’s management plan involves a multi-faceted approach. She works closely with her physician to optimize medication, such as fludrocortisone to address blood pressure regulation and beta-blockers to control tachycardia. She also implements lifestyle modifications, including gradual increases in physical activity, regular hydration, and compression stockings to reduce pooling of blood in the extremities.
Evolution of Sarah’s Condition
Sarah’s condition demonstrates the dynamic nature of POTS. Initially, her symptoms were severe, leading to frequent absences from work and social events. Through consistent adherence to her treatment plan and proactive management of triggers, her symptoms gradually improved. She now experiences less frequent episodes of lightheadedness and fainting, allowing her to maintain a more active and fulfilling lifestyle.
A Daily Routine for Someone with POTS
A typical day for Sarah might look like this:
- Morning (6:00 AM): Gradual rising, starting with a period of lying down to avoid sudden drops in blood pressure. Small sips of water and a light breakfast are consumed to prevent dehydration.
- Mid-morning (9:00 AM): Regular breaks to sit or lie down, avoiding prolonged standing. She ensures sufficient hydration and snacks throughout the day.
- Afternoon (12:00 PM): Lunch is eaten slowly and is followed by a period of rest. She might use a standing desk to avoid prolonged sitting and encourages movement.
- Evening (6:00 PM): A light dinner and relaxation exercises to help promote a good night’s sleep.
- Night (9:00 PM): Maintaining a consistent sleep schedule to support overall health and well-being.
This detailed routine helps Sarah manage her symptoms and maintain a sense of normalcy.
Illustrative Examples of Symptoms
Symptoms of POTS vary greatly, but some common examples include:
- Orthostatic Tachycardia: A rapid increase in heart rate when standing up from a seated or lying position. This might be accompanied by a sensation of lightheadedness or dizziness. A heart rate increase of more than 30 bpm is considered significant.
- Neurological Symptoms: Headaches, brain fog, and difficulty concentrating can be common. These are often connected to the circulatory and autonomic nervous system dysfunction.
- Gastrointestinal Symptoms: Abdominal pain, nausea, and bloating can also be associated with POTS, potentially due to reduced blood flow to the digestive organs.
- Fatigue: Persistent feelings of exhaustion and tiredness, often unrelated to the amount of activity performed.
- Visual Disturbances: Blurred vision, double vision, or even temporary vision loss can be experienced when blood pressure fluctuates.
Epilogue
In conclusion, postural orthostatic tachycardia syndrome (POTS) is a multifaceted condition requiring a multifaceted approach to understanding, diagnosis, and management. This post has highlighted the various facets of POTS, from its defining characteristics and symptoms to diagnostic procedures and treatment options. Ultimately, recognizing the impact of POTS on daily life and supporting individuals through self-management strategies is essential for improving their quality of life.
Future research and improved awareness are critical to enhancing our understanding and treatment of POTS.










