How lupus is diagnosed is a multifaceted process, crucial for timely and effective treatment. This journey often begins with recognizing the subtle symptoms that might point towards lupus. Understanding the diverse range of symptoms, from fatigue to joint pain, is vital for raising awareness and prompting a visit to a healthcare professional. A thorough medical history is also a cornerstone of the diagnostic process, allowing doctors to piece together the patient’s experience and identify potential patterns.
This detailed guide will explore the various steps involved in diagnosing lupus, from initial evaluations and physical examinations to the interpretation of diagnostic tests and laboratory findings. We’ll delve into the role of imaging techniques, and the critical aspect of differential diagnosis to rule out other conditions. Finally, we’ll discuss the importance of a multidisciplinary approach, recognizing the need for collaboration among specialists.
Introduction to Lupus Diagnosis
Lupus is a chronic autoimmune disease where the body’s immune system mistakenly attacks healthy tissues and organs. This attack can manifest in various ways, making diagnosis complex and often challenging. Understanding the multifaceted nature of lupus is crucial for early detection and effective management. This involves recognizing the common symptoms, carefully reviewing medical history, and performing specific diagnostic tests.
Accurate diagnosis allows for timely treatment and improved quality of life for individuals affected by this condition.The diagnosis of lupus is not a simple process. It often involves a combination of factors, including a thorough evaluation of symptoms, a detailed medical history, physical examination, and a series of tests. The absence of a single definitive test further complicates the diagnostic process.
Instead, healthcare professionals rely on a combination of findings to reach a conclusive diagnosis.
Common Symptoms Leading to Lupus Suspicion
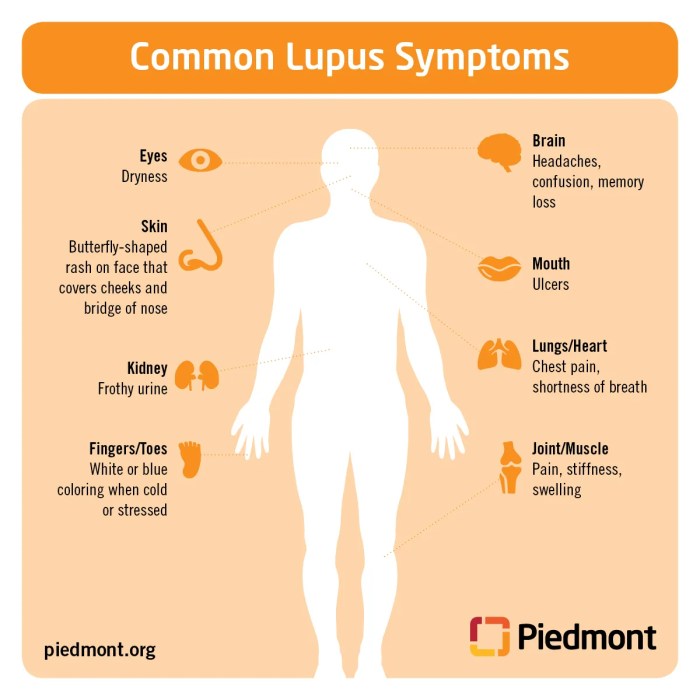
A range of symptoms can suggest the possibility of lupus. These symptoms can vary greatly in severity and frequency, making it important to consult with a healthcare professional if you experience any concerning signs. Common symptoms include fatigue, joint pain, skin rashes (such as a butterfly-shaped rash on the face), fever, and swelling in the joints. Other possible symptoms include hair loss, mouth sores, and kidney problems.
Importance of a Comprehensive Medical History
A detailed medical history is essential for diagnosing lupus. It provides context for understanding the patient’s overall health, past illnesses, and family history. This information helps to identify potential risk factors and patterns associated with lupus. Information regarding medications, previous diagnoses, and family history of autoimmune diseases can be crucial clues. A detailed account of symptoms, their duration, and any triggers can also contribute significantly to the diagnostic process.
Types of Lupus and Their Characteristics
Lupus presents in various forms, each with its unique characteristics. Understanding these variations is crucial for appropriate diagnosis and management.
Diagnosing lupus can be a bit of a puzzle, often involving a combination of physical exams, blood tests, and sometimes even a biopsy. It’s a process that can sometimes take time, much like figuring out the long-term outlook for type 2 diabetes. Factors like the severity of symptoms and the individual’s response to treatment influence the prognosis, as seen in type 2 diabetes prognosis.
Ultimately, a doctor will piece together the information to reach a diagnosis, considering symptoms and test results. This process is important for both effective treatment and management.
| Type | Symptoms | Diagnostic Tests | Treatment Options |
|---|---|---|---|
| Systemic Lupus Erythematosus (SLE) | Fatigue, joint pain, skin rashes, fever, kidney problems, and neurological issues. | Antinuclear antibody (ANA) test, complete blood count (CBC), urinalysis, kidney function tests, and sometimes biopsies. | Medication to suppress the immune system (immunosuppressants), pain relievers, and management of organ involvement. |
| Drug-induced Lupus | Symptoms resembling SLE, but triggered by certain medications. | ANA testing, and identification of the triggering medication. | Discontinuing the triggering medication, use of alternative medications, and management of symptoms. |
| Cutaneous Lupus | Skin rashes, often triggered by sunlight exposure. | Skin biopsy, ANA testing. | Topical corticosteroids, sun protection, and potentially immunosuppressants in severe cases. |
| Neonatal Lupus | Rare condition affecting newborns of mothers with lupus. | Testing of the newborn’s blood and tissues. | Monitoring and treatment of the newborn’s specific symptoms. |
Initial Evaluation and Physical Examination
The journey to a lupus diagnosis often begins with a thorough evaluation by a physician, focusing on a patient’s medical history and physical presentation. This initial assessment helps narrow down potential causes for the symptoms and identify potential red flags suggestive of lupus. A detailed physical examination plays a critical role in this process, providing valuable clues that might not be apparent from a review of symptoms alone.
Initial Steps in Evaluation
Physicians typically begin by taking a comprehensive medical history, including details about the patient’s symptoms, their duration, and any relevant family history of autoimmune diseases. They will also inquire about lifestyle factors, medications, and any recent infections or illnesses. This initial information helps in formulating a hypothesis about possible underlying conditions.
Importance of a Thorough Physical Examination
A physical examination is crucial for detecting subtle signs and symptoms that might be associated with lupus. A thorough examination of the skin, joints, and other organ systems can uncover physical manifestations that could suggest the presence of lupus or other conditions with similar presentations. These physical findings, when combined with the patient’s history, can aid in making a more informed diagnostic decision.
Specific Physical Exam Findings
Certain physical exam findings can point towards lupus, although they are not exclusive to the disease. These findings may include skin rashes, such as a malar rash (a butterfly-shaped rash across the cheeks and nose), discoid lupus lesions (coin-shaped lesions), or photosensitivity. Joint swelling, tenderness, or pain, especially in multiple joints, can also be indicative. Additionally, evidence of inflammation in other organ systems, such as the kidneys, lungs, or heart, might be detected through specific tests during the examination.
Table of Potential Physical Exam Findings
| Finding | Description | Potential Relevance to Lupus | Differential Diagnoses |
|---|---|---|---|
| Malar rash | Butterfly-shaped rash across the cheeks and nose, often with redness and scaling | Highly suggestive of systemic lupus erythematosus (SLE). | Rosacea, contact dermatitis, allergic reactions |
| Discoid lupus lesions | Red, raised, coin-shaped lesions on the skin, often with scarring | Suggestive of cutaneous lupus erythematosus. | Seborrheic dermatitis, psoriasis, eczema |
| Photosensitivity | Skin rash or other reactions triggered by exposure to sunlight | Common in lupus patients, especially those with malar rash. | Certain medications, porphyria, other skin conditions |
| Joint swelling and pain | Swelling, tenderness, and pain in multiple joints, often symmetric | Possible symptom of lupus-related arthritis. | Rheumatoid arthritis, osteoarthritis, gout |
| Pericarditis | Inflammation of the pericardium (the sac surrounding the heart), characterized by chest pain | Possible cardiac involvement in lupus. | Myocardial infarction, angina, chest wall pain |
| Proteinuria | Presence of protein in the urine | Suggestive of lupus nephritis (kidney involvement). | Glomerulonephritis, other kidney disorders |
Diagnostic Tests
Pinpointing lupus can be a detective work, requiring a combination of clues from various tests. A thorough understanding of the diagnostic process is crucial, as it helps healthcare providers to narrow down the possibilities and accurately diagnose the condition. The diagnostic journey often involves several steps, each contributing a piece to the puzzle.
Common Diagnostic Tests
A battery of tests is employed to identify lupus. These tests help determine if the symptoms are indicative of lupus, and whether there are any accompanying complications. These tests, when interpreted correctly, provide valuable insights into the body’s response to the disease.
Blood Tests
Blood tests are fundamental in lupus diagnosis. They assess various aspects of the immune system and identify markers associated with the disease. These tests are often the first line of investigation.
- Antinuclear Antibody (ANA) test: This test detects antibodies that attack the body’s own tissues. A positive ANA result suggests an autoimmune response, a hallmark of lupus. However, a positive ANA doesn’t definitively diagnose lupus, as it can also be present in other autoimmune conditions. Further testing is necessary to confirm the diagnosis.
- Anti-dsDNA test: This test looks for antibodies targeting double-stranded DNA. A positive anti-dsDNA result is a strong indicator of lupus. Its presence is often more specific for lupus compared to ANA.
- Complement levels: Complement proteins are part of the immune system. In lupus, these proteins can be depleted. Low levels of complement proteins suggest lupus activity.
- Complete Blood Count (CBC): This test evaluates different blood cell types, including red blood cells, white blood cells, and platelets. A CBC can reveal signs of anemia, low white blood cell counts (leukopenia), or low platelet counts (thrombocytopenia), which are sometimes associated with lupus.
- Erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP): These tests measure inflammation in the body. Elevated ESR and CRP levels often indicate inflammation, which can be present in lupus.
Other Tests
While blood tests are crucial, other investigations may be necessary to evaluate the impact of lupus on different organ systems.
- Urinalysis: This test examines the urine for abnormalities, such as protein or blood, which might indicate kidney involvement in lupus.
- Kidney Biopsy: If kidney involvement is suspected, a kidney biopsy can provide a more detailed assessment of the kidney tissue and help determine the extent of the damage.
- Immunological tests: These tests can further evaluate the immune system to look for specific antibodies or other markers associated with lupus. These tests can include tests for anti-Smith (anti-Sm) antibodies, antiphospholipid antibodies (aPL), and others.
Diagnostic Test Summary
| Test | Purpose | Procedure | Expected Results |
|---|---|---|---|
| Antinuclear Antibody (ANA) | Detects antibodies attacking the body’s own tissues. | Blood sample analysis. | Positive result indicates an autoimmune response, but further tests are needed. |
| Anti-dsDNA | Identifies antibodies targeting double-stranded DNA. | Blood sample analysis. | Positive result is a strong indicator of lupus, but not definitive. |
| Complement levels | Evaluates complement proteins in the immune system. | Blood sample analysis. | Low levels suggest lupus activity. |
| Complete Blood Count (CBC) | Assesses blood cell counts. | Blood sample analysis. | May reveal anemia, leukopenia, or thrombocytopenia. |
| Erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP) | Measures inflammation in the body. | Blood sample analysis. | Elevated levels often indicate inflammation, which may be associated with lupus. |
| Urinalysis | Evaluates urine for abnormalities indicating kidney involvement. | Urine sample analysis. | Presence of protein or blood may suggest kidney problems. |
| Kidney Biopsy | Detailed assessment of kidney tissue. | Tissue sample analysis. | Evaluates the extent of kidney damage if involvement is suspected. |
Laboratory Tests
Laboratory tests play a crucial role in diagnosing lupus. They help identify specific antibodies and markers associated with the disease, complementing the clinical evaluation and physical examination. These tests are essential for confirming a lupus diagnosis, monitoring disease activity, and assessing treatment effectiveness. A comprehensive approach to laboratory testing, combined with clinical information, significantly increases the accuracy of the diagnosis.
Diagnosing lupus involves a combination of medical history, physical exams, and blood tests. It’s a complex process, and sometimes tricky to pinpoint. While researching different holistic approaches, I stumbled upon some interesting information about how CBD oil might help manage diabetes symptoms. Learning more about potential treatments like cbd oil for diabetes is a fascinating avenue for exploring alternative solutions.
Ultimately, though, the standard diagnostic process for lupus remains crucial.
Role of Laboratory Tests in Lupus Diagnosis
Lupus diagnosis often involves a panel of laboratory tests to detect specific antibodies and markers. These tests are not definitive on their own, but when combined with clinical findings, they can provide valuable evidence for the presence of lupus. Blood tests are particularly helpful in identifying these markers and antibodies.
Specific Blood Tests for Lupus-Related Antibodies and Markers
A variety of blood tests can help detect lupus-related antibodies and markers. These include tests for antinuclear antibodies (ANA), anti-double-stranded DNA (anti-dsDNA), and other autoantibodies. Complement levels are also measured.
Interpretation of Abnormal Laboratory Findings
The interpretation of laboratory results is crucial in lupus diagnosis. A positive ANA test alone does not confirm lupus, as it can be found in other autoimmune conditions. The presence of other antibodies, such as anti-dsDNA, along with clinical symptoms, strongly suggests lupus. Complement levels, which are proteins that help fight infection, can also be reduced in lupus, reflecting disease activity.
The specific pattern of antibodies and markers, and their levels, together with clinical information, provide a more comprehensive picture.
Examples of Specific Lab Results Suggesting Lupus
A patient with a history of fatigue, joint pain, and a positive ANA test with a high titer of anti-dsDNA antibodies is a strong indication of lupus. Similarly, a patient exhibiting skin rashes, kidney involvement, and a decreased complement level further supports the suspicion of lupus. The combination of these factors and their levels strongly suggests lupus.
Laboratory Tests for Lupus Diagnosis: A Detailed Table
| Test | Purpose | Expected Lupus Results | Potential False Results |
|---|---|---|---|
| Antinuclear Antibodies (ANA) | Detects antibodies attacking the cell’s nucleus. | Positive; often present in various patterns, including speckled, homogenous, and nucleolar. High titers suggest increased disease activity. | Positive in other autoimmune diseases, infections, and even healthy individuals. False negatives can occur due to low antibody levels or specific testing methodologies. |
| Anti-double-stranded DNA (anti-dsDNA) | Detects antibodies attacking double-stranded DNA. | Positive, often elevated in active lupus, especially when associated with kidney involvement. | Can be present in other autoimmune diseases, and in some cases, may be negative even in patients with lupus. |
| Complement Levels (C3, C4) | Evaluates the levels of proteins in the complement system, which plays a role in immune function. | Decreased levels, often associated with active lupus and disease flares. | Low levels can be found in other conditions, such as infections or liver diseases. |
| Erythrocyte Sedimentation Rate (ESR) | Measures the rate at which red blood cells settle in a sample of blood. | Increased ESR, indicative of inflammation. | High ESR can be present in various inflammatory conditions. |
Imaging Techniques: How Lupus Is Diagnosed
While blood tests and physical examinations are crucial in lupus diagnosis, imaging techniques can offer valuable insights into potential organ involvement and associated conditions. They are not typically the primary diagnostic tool for lupus, but they can help confirm suspected issues or rule out other conditions. Understanding the role of imaging in lupus diagnosis is essential for a comprehensive evaluation.
Role of Imaging in Lupus Diagnosis
Imaging techniques, such as X-rays, ultrasounds, and CT scans, are used to visualize internal structures and assess organ function and health. These techniques can reveal signs of inflammation, damage, or abnormalities in organs that might be affected by lupus, such as the kidneys, lungs, or joints. They can also help distinguish lupus-related symptoms from other potential causes. For instance, imaging can aid in differentiating between lupus nephritis (kidney inflammation) and other kidney conditions.
Types of Imaging Used
Various imaging techniques provide different levels of detail and information. Understanding the capabilities of each technique is crucial in selecting the most appropriate imaging modality for a given situation.
- X-rays: X-rays are relatively inexpensive and readily available. They provide basic images of bones and internal organs, revealing structural abnormalities and bone erosion, which are sometimes associated with lupus. X-rays are particularly useful in evaluating joint involvement, identifying potential fractures, or assessing the extent of lung inflammation. For instance, they can show the presence of inflammation or swelling in joints, helping diagnose inflammatory arthritis that might be linked to lupus.
- Ultrasounds: Ultrasound imaging uses sound waves to create images of internal organs. It is particularly useful for assessing soft tissues, such as the kidneys, heart, and joints, and detecting inflammation or fluid buildup. In lupus, ultrasound can evaluate the kidneys to identify signs of lupus nephritis, assess joint swelling, or check for fluid accumulation in the heart. For example, the presence of abnormal echoes or fluid collections in the kidneys can be indicative of lupus nephritis.
- CT Scans: CT scans use X-rays to create detailed cross-sectional images of the body. They offer more detailed visualization than X-rays, allowing for the evaluation of internal structures and organs in greater depth. In lupus, CT scans can be used to evaluate lung involvement, identify complications in the abdomen, or assess the extent of inflammation in the kidneys. For example, a CT scan of the lungs may reveal signs of inflammation or scarring in patients with lupus-related lung involvement.
Information Derived from Each Technique
Each imaging technique provides specific information relevant to lupus diagnosis. X-rays reveal bone and joint abnormalities, while ultrasounds offer detailed views of soft tissues and organs, and CT scans provide a more comprehensive view of the internal structures.
Diagnosing lupus isn’t straightforward; it often involves a combination of physical exams, blood tests, and sometimes even a biopsy. Considering the potential for overlapping symptoms with other conditions, like issues related to IUD use in nulliparous women, iud use in nulliparous women can sometimes be a factor in the diagnostic process. Ultimately, a rheumatologist plays a crucial role in confirming the diagnosis and outlining a tailored treatment plan.
How Imaging Findings Support or Refute a Lupus Diagnosis, How lupus is diagnosed
Imaging findings can either support or refute a lupus diagnosis, depending on the specific findings and their correlation with other clinical features. For example, if a patient presents with joint pain and X-rays show erosive changes, this would support a diagnosis of lupus-related arthritis. Conversely, if a patient with suspected lupus has normal imaging results, it might suggest an alternative diagnosis.
Imaging findings should be interpreted in conjunction with other diagnostic tests and clinical history.
Table of Imaging Techniques in Lupus Diagnosis
| Technique | Application in Lupus Diagnosis | Typical Findings | Limitations |
|---|---|---|---|
| X-rays | Evaluating joint involvement, bone erosion, assessing lung inflammation | Joint swelling, bone erosion, possible fractures, evidence of inflammation in the lungs | Limited soft tissue visualization, less detailed than other modalities |
| Ultrasound | Assessing kidneys, heart, and joints for inflammation, fluid buildup, or abnormalities | Inflammation, fluid buildup, abnormal echoes in the kidneys, joint swelling | Limited penetration depth, may not detect deep-seated abnormalities |
| CT Scan | Evaluating lung involvement, abdominal complications, kidney inflammation | Lung inflammation, abdominal abnormalities, kidney swelling, inflammation | Higher radiation exposure compared to other techniques, more expensive |
Differential Diagnosis

Diagnosing lupus involves a crucial step: ruling out other conditions that might mimic its symptoms. This process, known as differential diagnosis, is essential for accurate treatment and management. It’s a careful comparison of the patient’s presentation with various other potential illnesses to pinpoint the exact cause of their symptoms. Failure to properly distinguish lupus from similar conditions can lead to inappropriate treatment and delayed access to the right care.
Importance of Ruling Out Mimicking Conditions
Accurately distinguishing lupus from other conditions is vital for proper management and treatment. Symptoms like fatigue, joint pain, and skin rashes can overlap significantly with various other diseases. Mistaking lupus for another condition can result in delayed or inappropriate treatment, impacting the patient’s overall well-being and potentially worsening the condition. A thorough differential diagnosis helps identify the correct underlying cause, leading to effective and targeted interventions.
Comparison of Lupus with Other Conditions
Lupus symptoms can closely resemble those of other autoimmune disorders, connective tissue diseases, and even infections. For instance, inflammatory arthritis, similar to lupus arthritis, can manifest with joint pain and swelling. The fatigue associated with lupus can also overlap with chronic fatigue syndrome or other medical conditions. Skin rashes characteristic of lupus can also be seen in other dermatological disorders.
This overlap highlights the necessity of comprehensive testing to definitively identify lupus.
Examples of Conditions in Differential Diagnosis
Several conditions share overlapping symptoms with lupus. These include rheumatoid arthritis, systemic sclerosis (scleroderma), Sjögren’s syndrome, and certain infections. Each condition has unique characteristics that, when considered in conjunction with a thorough clinical evaluation and laboratory tests, help distinguish it from lupus. Additionally, certain medications can induce symptoms mimicking lupus.
Methods for Distinguishing Lupus from Other Conditions
Distinguishing lupus from other conditions requires a multi-faceted approach. This includes a comprehensive medical history, physical examination, and a battery of laboratory and imaging tests. Careful consideration of the patient’s symptoms, their duration, and associated factors is crucial. The presence of specific autoantibodies, such as anti-dsDNA antibodies, is often helpful in diagnosing lupus. Furthermore, imaging techniques, such as X-rays or MRIs, can help evaluate the extent of organ involvement.
Comparison Table
| Condition | Symptoms | Diagnostic Tests | Treatment |
|---|---|---|---|
| Lupus | Fatigue, joint pain, skin rashes, fever, kidney problems, inflammation | Antinuclear antibody (ANA) test, Anti-dsDNA antibody test, complement levels, urinalysis, kidney biopsy | Immunosuppressants, corticosteroids, pain relievers |
| Rheumatoid Arthritis | Joint pain, stiffness, swelling, fatigue | Rheumatoid factor (RF) test, anti-CCP antibody test, X-rays | NSAIDs, disease-modifying antirheumatic drugs (DMARDs) |
| Systemic Sclerosis (Scleroderma) | Skin tightening, Raynaud’s phenomenon, joint pain, fatigue | Skin biopsy, ANA test, anti-centromere antibodies, anti-topoisomerase antibodies | Symptomatic treatment, medications to manage symptoms |
Additional Diagnostic Considerations
Beyond the initial evaluation and laboratory tests, a thorough understanding of the patient’s history, symptoms, and physical examination findings plays a crucial role in diagnosing lupus. This holistic approach helps differentiate lupus from other conditions with overlapping symptoms and ensures accurate and timely treatment. A crucial aspect of this process is the involvement of multiple specialists, each contributing their expertise to create a comprehensive picture of the patient’s condition.
Importance of Patient History and Symptom Analysis
A detailed patient history, meticulously collected, is invaluable in identifying patterns and potential triggers of lupus symptoms. This includes not only the onset and duration of symptoms but also relevant past medical history, family history of autoimmune diseases, environmental exposures, and lifestyle factors. A thorough symptom analysis, evaluating the specific nature, location, and severity of symptoms, provides further insights into the potential underlying cause.
For example, persistent fatigue, joint pain, and rashes, when coupled with a history of photosensitivity, strongly suggest the possibility of lupus.
Influence of Physical Examination
A comprehensive physical examination is essential to evaluate the extent and distribution of lupus manifestations. This includes checking for characteristic skin lesions, such as malar rash or discoid lupus, and assessing joint involvement, including swelling, tenderness, and range of motion limitations. The presence of specific findings, such as lymphadenopathy or splenomegaly, can also aid in differentiating lupus from other conditions.
Physical examination findings, in conjunction with patient history, often provide a valuable initial indication of the potential diagnosis.
Need for Multidisciplinary Evaluation
Lupus is a complex autoimmune disease that can affect various organ systems. A multidisciplinary approach, involving specialists from different fields, is often necessary to manage the multifaceted nature of the condition. This approach allows for a comprehensive evaluation of the patient’s needs, ensures that all potential complications are addressed, and promotes the most effective treatment strategy.
Involvement of Different Specialists
Managing a lupus patient often requires the collaboration of several specialists. Each specialist brings unique expertise, enabling a more comprehensive understanding of the patient’s condition and facilitating tailored treatment plans. The involvement of rheumatologists, dermatologists, nephrologists, neurologists, and cardiologists, among others, is frequently necessary depending on the specific manifestations of the disease.
| Specialist | Expertise | Role in Diagnosis | Example Procedures |
|---|---|---|---|
| Rheumatologist | Autoimmune diseases, musculoskeletal disorders | Initial evaluation, diagnosis confirmation, management of systemic manifestations | Physical exam, blood tests, imaging studies, disease activity assessments |
| Dermatologist | Skin conditions | Evaluation of skin rashes, lesions, and photosensitivity | Skin biopsies, dermatological examinations |
| Nephrologist | Kidney diseases | Assessment of kidney involvement, management of lupus nephritis | Renal biopsies, blood tests (e.g., creatinine, proteinuria), monitoring kidney function |
| Neurologist | Nervous system disorders | Evaluation of neurological symptoms, management of lupus-related neurological complications | Neurological examinations, nerve conduction studies, brain imaging |
| Cardiologist | Heart conditions | Assessment of heart involvement, management of cardiovascular complications | Electrocardiograms (ECGs), echocardiograms, cardiac catheterizations |
Closing Notes
Diagnosing lupus requires a comprehensive approach, blending patient history, physical examinations, and a variety of diagnostic tests. Understanding the multifaceted nature of lupus and the role of different specialists is essential for successful management. This guide provides a thorough overview of the process, empowering readers with the knowledge to better understand this complex autoimmune disease. By recognizing the interconnectedness of these elements, patients and healthcare providers can navigate the diagnostic journey more effectively, ultimately leading to earlier intervention and improved outcomes.










