Eosinophilic esophagitis signs symptoms are a critical focus for understanding this often-misunderstood condition. This comprehensive guide explores the various facets of the disease, from its underlying mechanisms to the diverse range of symptoms experienced by patients across different age groups. We’ll delve into the common gastrointestinal and extra-intestinal manifestations, alongside diagnostic procedures and management strategies.
This in-depth look at eosinophilic esophagitis signs and symptoms will equip readers with a better understanding of this condition, empowering them with knowledge to discuss it with healthcare professionals. We’ll examine how symptoms vary across different stages of the disease and different demographics, highlighting the unique challenges faced by patients of all ages.
Introduction to Eosinophilic Esophagitis (EoE)
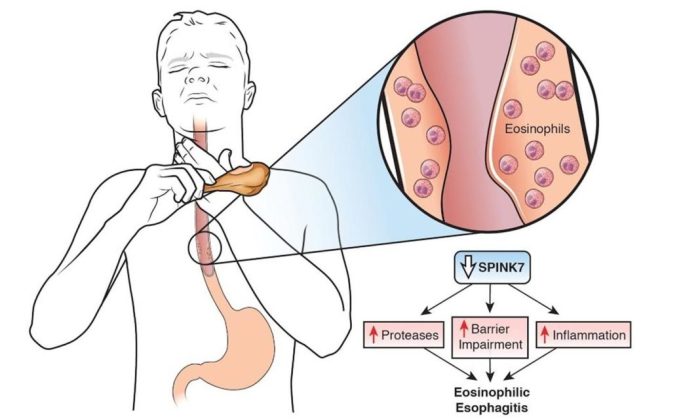
Eosinophilic esophagitis (EoE) is a chronic inflammatory condition of the esophagus, characterized by an abnormal immune response that leads to the accumulation of eosinophils, a type of white blood cell, within the esophageal tissue. This buildup of eosinophils causes inflammation and damage to the esophageal lining, impairing its function and often leading to difficulty swallowing and other digestive issues.
Understanding the underlying mechanisms and triggers of EoE is crucial for effective diagnosis and management.
Defining Eosinophilic Esophagitis
EoE is a chronic immune-mediated esophageal disorder. It’s characterized by the infiltration of eosinophils into the esophageal mucosa, resulting in inflammation and tissue damage. The disease can range from mild to severe, impacting the quality of life of those affected.
Mechanisms and Causes of EoE
The precise mechanisms underlying EoE are still not fully understood, but it’s believed to involve an interplay of genetic predisposition and environmental factors. An aberrant immune response, likely involving an overreaction of the immune system to certain dietary proteins, is considered a crucial factor. This immune response triggers the recruitment and activation of eosinophils, leading to inflammation and esophageal damage.
Certain food allergens, such as milk, soy, wheat, eggs, and fish, are frequently implicated.
Key Inflammatory Cells Involved
Eosinophils are the primary inflammatory cells implicated in EoE. These cells release various inflammatory mediators, contributing to the esophageal inflammation and damage. Other immune cells, including T lymphocytes, are also involved in the inflammatory cascade, further exacerbating the process. The exact interplay and relative contributions of these different immune cells are still under investigation.
Patient Demographics Affected by EoE
EoE typically affects children and young adults, although it can present at any age. Males are more commonly affected than females. The condition is more prevalent in developed countries, possibly reflecting differing dietary exposures or environmental factors. It’s important to note that the exact reasons for this demographic distribution are still being researched.
| Definition | Mechanism | Cells Involved | Demographics |
|---|---|---|---|
| Chronic inflammatory condition of the esophagus, characterized by eosinophil accumulation. | Aberrant immune response, likely triggered by dietary proteins, leading to eosinophil recruitment and activation. | Primarily eosinophils, with involvement of T lymphocytes and other immune cells. | Predominantly affects children and young adults, with a higher prevalence in males and developed countries. |
Common Signs and Symptoms
Eosinophilic esophagitis (EoE) is a chronic condition characterized by inflammation in the esophagus. This inflammation, driven by eosinophils (a type of white blood cell), can lead to a wide range of symptoms, often varying in severity and presentation depending on the individual’s age and the stage of the disease. Understanding these symptoms is crucial for early diagnosis and effective management.The symptoms of EoE can manifest in different ways, and their severity can fluctuate over time.
Some individuals experience mild discomfort, while others have significant symptoms that impact their daily lives. The spectrum of severity is influenced by the degree of esophageal inflammation and the involvement of other organs.
Symptoms Across Different Age Groups
The presentation of EoE can differ significantly between infants, children, and adults. Factors such as developmental stage and the ability to communicate symptoms can affect how the condition is recognized.
- Infants often display feeding difficulties, such as refusing to eat, or frequent spitting up or vomiting. They might also exhibit irritability or weight loss, and sometimes experience esophageal narrowing that leads to food getting stuck. These symptoms can be challenging to distinguish from other common infant issues.
- Children might experience more noticeable symptoms like pain with swallowing (dysphagia), food getting stuck in the throat, or recurrent chest pain. They may also complain of nausea or vomiting, especially after meals. Their ability to articulate their discomfort plays a crucial role in diagnosis.
- Adults frequently report difficulty swallowing, often describing a feeling of food getting stuck in the chest or throat. They might also experience heartburn, chest pain, or abdominal pain. These symptoms can be easily mistaken for other digestive disorders, delaying diagnosis. Chronic cough and/or regurgitation can also be seen in adults.
Symptom Comparison Across Age Groups
| Symptom | Description | Typical Presentation in Age Group |
|---|---|---|
| Feeding Difficulties | Refusal to eat, frequent spitting up, vomiting | Infants |
| Food Getting Stuck | Difficulty swallowing; sensation of food lodging in the throat | Children, Adults |
| Pain with Swallowing (Dysphagia) | Discomfort or pain while swallowing | Children, Adults |
| Heartburn | Burning sensation in the chest | Adults |
| Chest Pain | Pain in the chest area | Children, Adults |
| Abdominal Pain | Pain in the abdomen | Children, Adults |
| Nausea/Vomiting | Upset stomach; expulsion of stomach contents | Children, Adults |
| Weight Loss | Unintentional decrease in body weight | Infants, Children |
| Irritability | Increased fussiness or restlessness | Infants |
| Chronic Cough | Persistent cough, lasting for more than 8 weeks | Adults |
| Regurgitation | Bringing up undigested food | Infants, Adults |
Gastrointestinal Manifestations
Eosinophilic esophagitis (EoE) often presents with a range of gastrointestinal symptoms, extending beyond the esophagus. Understanding these manifestations is crucial for accurate diagnosis and effective management. These symptoms can vary significantly in severity and presentation, making recognition challenging at times.The primary hallmark of EoE is inflammation within the gastrointestinal tract. This inflammation, driven by eosinophils, can impact various parts of the digestive system, leading to a constellation of symptoms.
Eosinophilic esophagitis can manifest with a range of symptoms, from difficulty swallowing to chest pain. While exploring dietary remedies, it’s worth noting the potential benefits of incorporating cranberries into your diet. A good resource for understanding the nutritional value of cranberries, including their potential health advantages, can be found at cranberry nutrition and benefits. However, remember that while cranberries might offer some health perks, they shouldn’t replace necessary medical treatment for eosinophilic esophagitis.
These symptoms, while sometimes subtle, can significantly impact a patient’s quality of life.
Common Gastrointestinal Symptoms
Gastrointestinal symptoms associated with EoE can be quite diverse. Patients may experience recurrent dysphagia (difficulty swallowing), a sensation of food sticking in the throat, or chest pain. Other common symptoms include abdominal pain, nausea, vomiting, and even unintentional weight loss. The presence and severity of these symptoms can fluctuate over time, and some individuals may only experience symptoms intermittently.
Typical Endoscopic Findings in EoE
Upper endoscopy is a critical diagnostic tool for EoE. During this procedure, the physician visualizes the lining of the esophagus, stomach, and duodenum. Typical findings in EoE patients include esophageal narrowing (strictures), which may appear as a “pipe-like” constriction, along with mucosal irregularities. The lining may appear red, swollen, or have a corrugated appearance, reflecting the underlying inflammatory process.
In some cases, small white bumps (papules) or linear furrows (grooves) might be observed.
Associated Gastrointestinal Issues
EoE is not always isolated to the esophagus. Frequently, patients with EoE may also experience symptoms related to other parts of the gastrointestinal tract. These may include gastritis, duodenitis, or even small intestinal issues. In some instances, there may be overlap in symptoms, making diagnosis more complex. These associated issues further highlight the multifaceted nature of EoE.
Table of Typical Endoscopic Findings in EoE
| Endoscopic Finding | Description | Frequency |
|---|---|---|
| Esophageal Strictures | Narrowing of the esophageal lumen, often appearing “pipe-like” or constricted | High |
| Mucosal Irregularities | Uneven or bumpy appearance of the esophageal mucosa | High |
| Erythema (Redness) | Inflammation causing redness of the esophageal mucosa | Moderate |
| Edema (Swelling) | Inflammation leading to swelling of the esophageal mucosa | Moderate |
| Corrugated Mucosa | Wrinkled or folded appearance of the esophageal lining | Moderate |
| Papules (Small White Bumps) | Small, raised, white lesions on the esophageal mucosa | Variable |
| Linear Furrows (Grooves) | Long, shallow grooves or furrows in the esophageal lining | Variable |
Extra-Gastrointestinal Symptoms
Beyond the esophagus, eosinophilic esophagitis (EoE) can manifest in various ways throughout the body. These extra-intestinal symptoms are often less prominent than the gastrointestinal ones, but can significantly impact a patient’s overall well-being and quality of life. Understanding these symptoms is crucial for comprehensive diagnosis and management of EoE.
Possible Mechanisms of Extra-intestinal Symptoms
The underlying inflammatory process characteristic of EoE isn’t confined to the esophagus. The immune system’s response, triggered by eosinophils, can extend to other tissues and organs, leading to a range of extra-intestinal symptoms. This systemic inflammation may result from the release of inflammatory mediators or the migration of eosinophils to affected areas. The precise mechanisms connecting esophageal inflammation to extra-intestinal symptoms are still under investigation, but a strong link is evident in many cases.
Common Extra-intestinal Issues in EoE Patients
EoE isn’t solely a digestive disorder. Patients frequently experience a constellation of symptoms beyond the gastrointestinal tract. These symptoms vary in severity and presentation, but some common issues include skin conditions, allergic reactions, and respiratory problems. The prevalence of these extra-intestinal symptoms varies among patients.
Summary of Potential Extra-intestinal Symptoms
| Symptom | Potential Relationship to EoE | Frequency |
|---|---|---|
| Skin Conditions (e.g., eczema, atopic dermatitis) | Increased eosinophil activity and systemic inflammation. Often present in individuals with atopic predisposition. | Common |
| Allergic Rhinitis | Shared immune system response, particularly involving mast cells and eosinophils. | Common |
| Asthma | Similar immune mechanisms as in allergic rhinitis. Inflammation in the airways may be a direct result of eosinophil infiltration. | Common |
| Dental problems (e.g., enamel erosion) | Possible connection to frequent regurgitation or acid reflux, often associated with EoE. | Less common, but potentially linked |
| Neurological symptoms (e.g., headache, fatigue) | Inflammation and associated systemic effects could affect neurological function. May be related to nutrient deficiencies or other complications. | Variable, less frequently reported |
| Anal fissures | Chronic inflammation and irritation from gastrointestinal issues might contribute to anal fissures in some cases. | Rare, but possible |
| Other allergic manifestations (e.g., food allergies, urticaria) | Shared immune system involvement. Individuals with EoE often have other allergies. | Common, as part of atopic predisposition |
Diagnostic Procedures
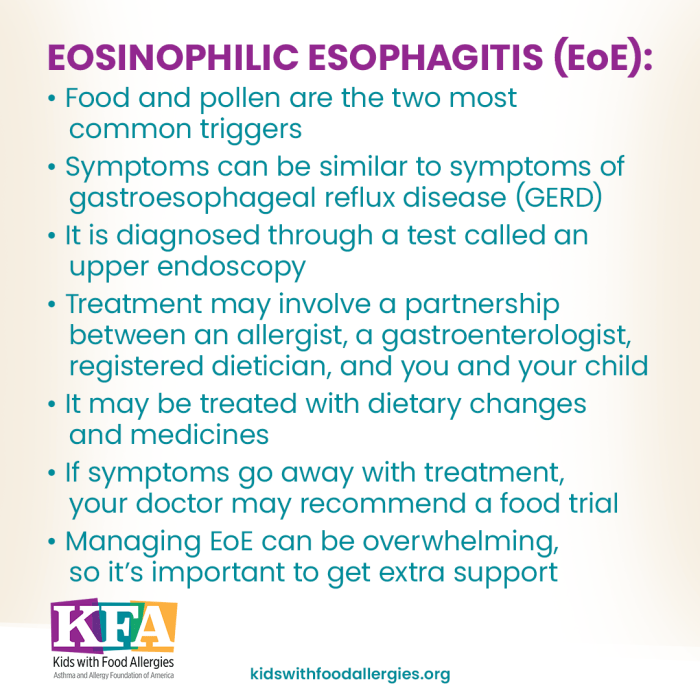
Pinpointing eosinophilic esophagitis (EoE) requires a meticulous approach that combines various diagnostic tools. It’s crucial to differentiate EoE from other esophageal conditions to ensure the most appropriate treatment plan. The diagnostic process often involves a series of steps, culminating in a definitive diagnosis.
Diagnostic Methods
Several methods aid in identifying EoE. These methods vary in their invasiveness and provide different levels of detail. Some are non-invasive, while others require a direct examination of the esophagus’s lining.
Role of Upper Endoscopy
Upper endoscopy is a pivotal procedure in the diagnostic pathway. It allows physicians to visualize the esophageal lining directly. During this procedure, a flexible tube with a camera at the end (endoscope) is passed down the throat. This provides a detailed view of the esophagus, enabling the detection of structural abnormalities. A skilled gastroenterologist can observe the presence of inflammation, strictures (narrowing), or other signs suggestive of EoE.
Furthermore, the visualization helps exclude other potential causes of esophageal symptoms.
Importance of Esophageal Biopsies
Esophageal biopsies are indispensable in confirming the diagnosis of EoE. They involve taking small tissue samples from the esophagus’s lining. These samples are then examined under a microscope by a pathologist. The microscopic examination focuses on the presence and concentration of eosinophils, the type of white blood cell characteristically elevated in EoE.
Differentiating EoE from Other Conditions
Biopsies are crucial for distinguishing EoE from other conditions that can cause similar symptoms. For instance, the presence of a significant number of eosinophils (typically 15 or more eosinophils per high-power field) strongly suggests EoE. Other conditions might exhibit eosinophils, but at lower counts or in different patterns. Careful microscopic analysis helps to differentiate EoE from conditions like gastroesophageal reflux disease (GERD), infections, or even allergic reactions.
Steps in a Diagnostic Procedure
- Patient History and Physical Examination: A thorough review of the patient’s symptoms, medical history, and family history is vital. The physical examination can reveal other signs that might suggest an underlying condition. This initial assessment helps to narrow down potential causes and prioritize diagnostic tests.
- Upper Endoscopy: This procedure allows visualization of the esophagus’s lining. The physician observes the presence of inflammation, strictures, or other abnormalities that could indicate EoE.
- Esophageal Biopsies: Tissue samples are taken from different areas of the esophagus to evaluate the presence and density of eosinophils. A pathologist analyzes these biopsies under a microscope.
- Histological Analysis: The pathologist examines the tissue samples for the presence and count of eosinophils. The characteristic presence of 15 or more eosinophils per high-power field is a strong indicator of EoE. This helps differentiate EoE from other conditions.
- Exclusion of Other Conditions: Further tests, such as pH monitoring, may be performed to rule out other conditions, such as GERD. This comprehensive approach ensures the diagnosis is accurate and targeted.
Illustrative Case Studies
Understanding eosinophilic esophagitis (EoE) often requires looking at real-life examples. These case studies, while hypothetical, illustrate common presentations and symptoms of EoE in various age groups. This allows us to better grasp the potential range of experiences and challenges faced by individuals with this condition.
Adult Case Study: Mr. Johnson, Eosinophilic esophagitis signs symptoms
Mr. Johnson, a 35-year-old male, presented to his gastroenterologist with a history of progressive dysphagia (difficulty swallowing) over the past year. He described intermittent chest pain, particularly after meals, often accompanied by a feeling of food getting stuck in his chest. He also reported frequent episodes of heartburn, though he wasn’t consuming a large amount of spicy or acidic food.
Mr. Johnson also experienced occasional nausea and vomiting, which he found alarming. He noted a significant reduction in his ability to consume larger meals. His symptoms were not consistently related to specific foods, but he often experienced symptoms after eating anything.
- Symptoms included progressive dysphagia, intermittent chest pain after meals, heartburn, occasional nausea, and vomiting. The dysphagia was a key symptom, indicating difficulty in moving food through the esophagus.
- Symptoms were not consistently associated with specific food triggers.
- The combination of dysphagia, chest pain, and heartburn, along with a reduced ability to consume large meals, pointed towards a potential esophageal issue like EoE.
Pediatric Case Study: Lily
Lily, a 4-year-old female, was brought to her pediatrician by her parents due to persistent feeding difficulties. She was experiencing significant discomfort during meals and often refused to eat certain foods. Lily’s parents reported frequent vomiting, especially after consuming dairy products and certain fruits. She displayed signs of malnutrition, with a noticeable decrease in weight and a delay in growth.
Her pediatrician noticed that Lily had a history of eczema, which might suggest a link to other allergic conditions.
- Lily’s symptoms included persistent feeding difficulties, discomfort during meals, and refusal to eat certain foods.
- Symptoms were often triggered by specific food groups, such as dairy products and certain fruits, indicating a potential food allergy.
- The combination of feeding difficulties, vomiting, and signs of malnutrition in a child with a history of eczema raised suspicion of a possible allergic disorder such as EoE.
- The history of eczema further suggested a potential link between allergic disorders and gastrointestinal symptoms.
Differential Diagnoses
Navigating the world of digestive issues can be tricky, especially when symptoms mimic those of eosinophilic esophagitis (EoE). Many conditions share overlapping characteristics, making accurate diagnosis crucial. Differentiating EoE from similar conditions relies on a thorough evaluation of symptoms, medical history, and diagnostic tests.Understanding the conditions that can be confused with EoE is vital for appropriate treatment. This section will explore the common differential diagnoses, comparing their key features to those of EoE, and highlighting the diagnostic methods used to distinguish them.
Conditions Often Mistaken for EoE
Several conditions can present with symptoms similar to EoE, including gastroesophageal reflux disease (GERD), infectious esophagitis, and other inflammatory esophageal disorders. Recognizing the subtle differences between these conditions is critical for an accurate diagnosis.
Comparison of Key Features
The following table provides a concise comparison of EoE with other potential diagnoses. Each condition’s key features and distinguishing factors are highlighted to aid in differentiating them.
| Condition | Key Features | Differentiating Factors |
|---|---|---|
| Eosinophilic Esophagitis (EoE) | Chronic inflammation of the esophagus, characterized by a high number of eosinophils (a type of white blood cell). Symptoms include dysphagia (difficulty swallowing), food impaction, heartburn, and abdominal pain. | Elevated eosinophil counts in esophageal biopsies are a hallmark. Symptoms often worsen with specific foods. Response to medication varies. |
| Gastroesophageal Reflux Disease (GERD) | Chronic backflow of stomach acid into the esophagus. Symptoms include heartburn, regurgitation, and chest pain. | Acid reflux is a major factor. Symptoms are often relieved by antacids or proton pump inhibitors. Esophageal biopsies typically do not show eosinophilia. |
| Infectious Esophagitis | Inflammation of the esophagus caused by viral, bacterial, or fungal infections. Symptoms may include difficulty swallowing, pain with swallowing, and fever. | Presence of infection (viral, bacterial, or fungal) can be identified by specific tests (e.g., cultures, PCR). Symptoms often correlate with other systemic infections. |
| Other Inflammatory Esophageal Disorders | Conditions like graft-versus-host disease (GVHD) or autoimmune conditions can cause esophageal inflammation. | History of transplant or immune-related disorders is critical. Symptoms might be more widespread and correlate with other systemic symptoms. Diagnostic tests will be tailored to the suspected cause. |
Diagnostic Tests in Differential Diagnosis
A crucial aspect of differentiating EoE from other conditions involves specific diagnostic tests. These tests help to confirm the presence and severity of the condition. Endoscopy with esophageal biopsies is a cornerstone of diagnosis, enabling visualization of the esophageal lining and assessment of eosinophil levels. Furthermore, pH monitoring, esophageal manometry, and allergy testing can provide valuable insights into the underlying causes and characteristics of the condition.
Eosinophilic esophagitis can manifest with symptoms like difficulty swallowing and food getting stuck. While focusing on healthy eating is crucial, exploring the potential benefits of certain foods, like grapes, for weight loss is also important. For instance, are grapes good for weight loss a topic that can influence your dietary choices. Ultimately, managing eosinophilic esophagitis often requires a personalized approach, which includes careful consideration of a healthy diet.
This includes recognizing and managing potential triggers.
The choice of tests will depend on the suspected condition and the patient’s symptoms.
Eosinophilic esophagitis can manifest with a range of symptoms, like difficulty swallowing and chest pain. Sometimes, these symptoms can be accompanied by gas pains, which can be incredibly uncomfortable. If you’re experiencing those, checking out some quick fixes for relieving gas pains fast might be helpful. how to relieve gas pains fast However, it’s crucial to remember that these remedies might not address the underlying cause of the esophageal inflammation.
It’s always a good idea to consult a doctor for a proper diagnosis of eosinophilic esophagitis.
Management Strategies
Eosinophilic esophagitis (EoE) requires a multi-faceted approach to management, focusing on symptom relief, esophageal healing, and preventing long-term complications. A tailored strategy is crucial, considering individual patient needs and disease severity. This involves a combination of dietary modifications, medications, and potentially endoscopic procedures. Understanding the various management strategies is key to effectively controlling EoE and improving quality of life.
Dietary Modifications in EoE
Dietary modifications play a vital role in managing EoE, particularly in the initial stages of treatment. By identifying and eliminating trigger foods, patients can significantly reduce esophageal inflammation and promote healing. This approach often involves an elimination diet, followed by a gradual reintroduction of foods to pinpoint specific allergens.
- Food Elimination Diets: A common approach involves eliminating common food allergens, such as milk, eggs, wheat, soy, peanuts, tree nuts, fish, and shellfish. This elimination period can last several weeks to months, allowing the esophagus to heal. A registered dietitian can guide patients through the process of identifying triggers and creating a safe elimination diet.
- Elemental Diets: These diets provide essential nutrients in a highly-processed form, minimizing the risk of triggering an allergic reaction. They are often used as a temporary measure to promote healing, especially in severe cases, and are often supplemented with nutritional vitamins and minerals.
- Introduction of Foods: Once the elimination diet has been in place for a suitable duration, gradual reintroduction of foods is done to determine individual triggers. This cautious reintroduction allows clinicians and patients to track which foods cause symptoms. This process is often monitored by a healthcare professional to ensure patient safety and adherence to the plan.
Medication Management in EoE
Medications can be used to reduce inflammation and improve esophageal function. The choice of medication often depends on the severity of the condition and the patient’s response to dietary modifications.
- Proton Pump Inhibitors (PPIs): These medications, such as omeprazole and lansoprazole, reduce acid production in the stomach. They can be helpful in managing reflux symptoms that are often associated with EoE. This is not a primary treatment for EoE, but rather a supportive measure.
- Topical Steroids: These medications, applied directly to the esophagus, can help reduce inflammation. They are often used in conjunction with dietary modifications and can be administered via swallowed liquid, which allows the steroid to directly impact the esophagus. Their use should be under close medical supervision to ensure safety and efficacy.
- Leukotriene Inhibitors: These medications can help reduce inflammation throughout the body, including the esophagus. They are sometimes considered when other treatments have not been sufficient. The effectiveness varies among patients.
Therapeutic Approaches to EoE
Therapeutic approaches to EoE are comprehensive, focusing on both symptomatic relief and long-term management.
- Endoscopic Treatments: In some cases, endoscopic procedures, such as dilation of the esophagus, may be necessary to widen narrowed sections. These procedures are often considered when dietary and medication approaches have not been successful in managing symptoms.
- Immunotherapy: In certain cases, immunotherapy may be an option for managing EoE. This approach involves gradually exposing the patient to the food allergens to reduce the immune system’s response. This is typically a longer-term strategy and should be discussed with an allergist or immunologist.
- Comprehensive Management Plan: A tailored approach involving dietary modifications, medication, and potentially endoscopic procedures, and monitoring is critical to effective EoE management. This comprehensive plan ensures that patients receive the most appropriate care for their specific needs.
Conclusive Thoughts: Eosinophilic Esophagitis Signs Symptoms
In conclusion, eosinophilic esophagitis signs symptoms can present in a variety of ways, affecting individuals differently based on age and other factors. Understanding these diverse presentations is crucial for accurate diagnosis and effective management. This exploration provides a solid foundation for navigating the complexities of EoE, enabling readers to approach the topic with greater awareness and confidence.










