A complete guide to type 1 diabetes medications provides a comprehensive overview of the various treatments available for managing this condition. This detailed guide explores the fundamental role of medications, delving into different categories, from insulin to oral options and beyond. We’ll cover the mechanisms of action, potential side effects, and important considerations for choosing the right treatment plan.
Understanding the nuances of each medication type is crucial for effective management. This guide will walk you through the different insulin types, their actions, and delivery methods. It also addresses oral medications, highlighting their limitations and advantages, and discusses other medications that might be used in conjunction with insulin. Ultimately, the goal is to empower you with the knowledge needed to discuss treatment options with your healthcare provider and make informed decisions.
Introduction to Type 1 Diabetes Medications
Type 1 diabetes is an autoimmune disease where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leads to a deficiency in insulin, a hormone crucial for transporting glucose from the bloodstream into cells for energy. Without sufficient insulin, glucose builds up in the blood, causing various health complications. Effective management of type 1 diabetes requires a combination of lifestyle modifications and medications to maintain blood glucose levels within a healthy range.Medications play a fundamental role in managing type 1 diabetes.
They are essential for replacing the missing insulin, controlling blood glucose levels, and preventing long-term complications. Different types of medications are used to achieve these goals, catering to individual needs and treatment plans. Insulin therapy is a cornerstone of type 1 diabetes management, and other medications can be used to support blood glucose control and address associated conditions.
Insulin Therapies
Insulin is the primary medication for type 1 diabetes, as it is essential for regulating blood glucose levels. Different types of insulin are available, each with varying onset, peak, and duration of action. This allows for tailored insulin regimens to meet individual needs and blood glucose patterns. Rapid-acting, short-acting, intermediate-acting, and long-acting insulins are commonly used, providing flexibility in managing blood glucose fluctuations throughout the day and night.
Learning about type 1 diabetes medications can be overwhelming, but a complete guide can make it much easier to understand. While researching different treatments, I stumbled across some interesting info on managing skin conditions like keloids. For example, if you’re looking for advice on how to get rid of keloids, check out this helpful resource: how to get rid of keloids.
Ultimately, a good guide to type 1 diabetes medications will cover everything from insulin types to potential side effects, helping you make informed choices about your health.
Table of Type 1 Diabetes Medications
The following table Artikels different types of medications used in the management of type 1 diabetes. Note that this is not an exhaustive list, and specific medication choices are determined in consultation with a healthcare professional based on individual needs and circumstances.
| Medication Type | Mechanism of Action | Common Side Effects | Dosage Considerations |
|---|---|---|---|
| Rapid-acting Insulin (e.g., Lispro, Aspart) | Rapidly absorbed, mimicking the body’s natural insulin response to meals. | Hypoglycemia (low blood sugar), weight gain. | Administered shortly before meals to manage postprandial glucose spikes. Dosage is tailored to individual meal sizes and carbohydrate intake. |
| Short-acting Insulin (e.g., Regular Insulin) | Onset of action is faster than intermediate-acting insulins. | Hypoglycemia, weight gain. | Administered 30-45 minutes before meals. Dosage varies based on individual needs. |
| Intermediate-acting Insulin (e.g., NPH Insulin) | Provides a slower and more sustained release of insulin. | Hypoglycemia, weight gain. | Administered once or twice daily to provide basal insulin coverage. Dosage needs to be carefully adjusted based on individual blood glucose levels and lifestyle. |
| Long-acting Insulin (e.g., Glargine, Detemir) | Provides a constant basal level of insulin throughout the day. | Hypoglycemia, weight gain. | Administered once daily. Dosage is often adjusted based on blood glucose levels and response to the medication. |
| Injectable Glucagon | Raises blood glucose levels rapidly when hypoglycemia occurs. | Nausea, vomiting, and abdominal discomfort. | Administered via injection when severe hypoglycemia is detected. It’s important to know the proper dosage and administration technique. |
Other Medications
While insulin is the primary treatment, other medications can complement the treatment regimen to manage associated conditions or enhance blood glucose control.
- Metformin: This oral medication is sometimes used in combination with insulin therapy. It reduces glucose production in the liver and improves insulin sensitivity. It is not commonly used in type 1 diabetes as it doesn’t directly replace the insulin deficiency. It is more often used in type 2 diabetes.
- Sodium-Glucose Cotransporter 2 (SGLT2) inhibitors: These medications work by preventing the kidneys from reabsorbing glucose, leading to increased glucose excretion in the urine. These can help to lower blood glucose levels, but they are not typically the first choice in type 1 diabetes.
Insulin Medications
Insulin is the cornerstone of type 1 diabetes management. It’s crucial for regulating blood glucose levels and preventing serious complications. Understanding the various types of insulin, their actions, and delivery methods is vital for effective self-management.
Types of Insulin
Different types of insulin are designed to mimic the natural release of insulin in the body. They vary in their onset, peak, and duration of action, allowing for personalized treatment plans.
- Rapid-acting insulin: This type of insulin works quickly, mimicking the body’s natural response to a meal. It’s typically administered just before or during a meal to control the blood sugar rise after eating. Examples include lispro (Humalog), aspart (NovoLog), and glulisine (Apidra). These insulins have a very fast onset, reaching peak effectiveness within 15-30 minutes and lasting about 3-5 hours.
- Short-acting insulin: Regular insulin, also known as short-acting insulin, is another common type. It starts working within 30 minutes to an hour, reaches peak action in 2-4 hours, and lasts for about 6-8 hours. This type is often used before meals to cover the expected rise in blood glucose.
- Intermediate-acting insulin: This type of insulin is designed for longer-lasting blood glucose control. It begins to work within 1-2 hours, peaks in 4-12 hours, and remains effective for about 16-24 hours. Examples include NPH (Humulin N, Novolin N). These insulins are suitable for providing basal insulin coverage.
- Long-acting insulin: Long-acting insulin provides a steady, consistent release of insulin throughout the day. It has a gradual onset, with peak action typically not seen, and a very long duration of action, often lasting up to 24 hours. Examples include glargine (Lantus), detemir (Levemir). This type is typically administered once daily to maintain blood glucose control between meals and overnight.
- Combination insulin: These insulins combine two or more types of insulin in a single injection. This can simplify treatment and potentially improve blood glucose control, particularly in individuals with more complex or fluctuating blood glucose needs. Examples include premixed insulins containing rapid-acting and intermediate-acting insulin.
Mechanism of Action
All insulin types work by binding to insulin receptors on cells throughout the body. This binding triggers a cascade of events that facilitate glucose uptake from the bloodstream into the cells. Glucose is then used for energy or stored as glycogen for later use. The different types vary in how quickly they reach their maximum effect and how long they remain active.
Comparison of Insulin Types
| Insulin Type | Onset (minutes) | Peak (hours) | Duration (hours) | Typical Use Cases | Potential Side Effects |
|---|---|---|---|---|---|
| Rapid-acting | 15-30 | 1-2 | 3-5 | Mealtime coverage | Hypoglycemia (low blood sugar), weight gain |
| Short-acting | 30-60 | 2-4 | 6-8 | Mealtime coverage | Hypoglycemia, weight gain |
| Intermediate-acting | 1-2 | 4-12 | 16-24 | Basal coverage | Hypoglycemia, weight gain, localized reactions at injection site |
| Long-acting | 1-4 | No pronounced peak | 24-36 | Basal coverage, once-daily administration | Hypoglycemia, weight gain |
| Combination | Variable | Variable | Variable | Mealtime and basal coverage | Hypoglycemia, weight gain |
Insulin Delivery Systems
Different methods exist for delivering insulin, each with its own advantages and disadvantages. The choice of delivery system is often a personal one, tailored to individual needs and preferences.
| Delivery System | Description | Advantages | Disadvantages |
|---|---|---|---|
| Insulin Pens | Pre-filled pens that allow for precise dosage control. | Easy to use, discreet, and often less messy than syringes. | Can be more expensive in the long run, may require special training. |
| Insulin Pumps | Continuous subcutaneous insulin infusion devices. | More accurate insulin delivery, allows for more flexible meal timing, and potentially better blood glucose control. | Requires more technical knowledge and responsibility, potential for device malfunction. |
| Syringes | Traditional method of insulin administration. | Cost-effective. | Requires precise measurement, potentially more difficult to control dosage, and can be more time-consuming. |
Oral Medications
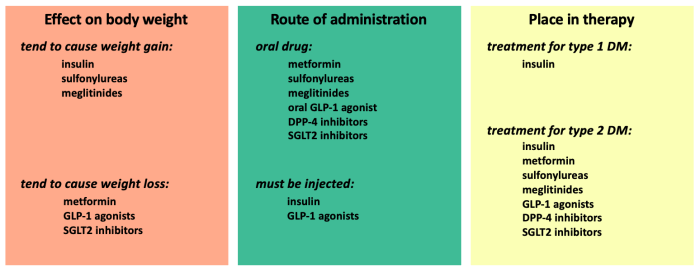
Oral medications play a crucial role in managing blood glucose levels in individuals with type 1 diabetes, though they are not a primary treatment. They are often used in conjunction with insulin therapy to fine-tune glucose control and improve overall management. The effectiveness of these medications can vary greatly from person to person, and their use requires careful consideration of individual needs and potential side effects.Oral medications are not a replacement for insulin in type 1 diabetes.
Insulin is essential for managing glucose production and utilization, and oral medications primarily work to improve the efficiency of insulin action or reduce glucose production. They cannot completely compensate for the absence of insulin production.
Oral Medications Used in Type 1 Diabetes
There are currently no FDA-approved oral medications specifically for use in type 1 diabetes. This is because the fundamental characteristic of type 1 diabetes is the complete or near-complete absence of insulin production by the pancreas. Oral medications typically target specific mechanisms related to insulin sensitivity or glucose production. Their use in type 1 diabetes is often considered an adjunct therapy to insulin.
Mechanism of Action
The limited oral medications used in type 1 diabetes typically work by enhancing insulin sensitivity in tissues, or by influencing how the liver releases glucose into the bloodstream. Metformin, for instance, is an oral medication that can improve insulin sensitivity in some individuals, but it does not directly replace insulin.
Limitations and Considerations
Oral medications in type 1 diabetes have limitations. They do not replace the crucial role of insulin, which is necessary for glucose uptake into cells. Their effectiveness can vary significantly, and they may not be sufficient to achieve optimal glucose control in all individuals. Careful monitoring and adjustment of insulin doses are critical when using oral medications alongside insulin therapy.
Advantages and Disadvantages of Oral Medications
Advantages of oral medications in type 1 diabetes are typically modest compared to their role in type 2 diabetes. Their use can sometimes improve insulin sensitivity, potentially lowering the required insulin dose, which may translate into improved blood glucose control and reduced risk of complications. However, this is not a universal benefit. Disadvantages include the potential for side effects, the need for frequent monitoring, and the fact that they do not address the fundamental deficiency of insulin production.
Summary Table
| Medication | Mechanism of Action | Effectiveness in Type 1 | Potential Side Effects |
|---|---|---|---|
| Metformin | Improves insulin sensitivity | May modestly improve glucose control in some cases, but not a primary treatment. | Gastrointestinal issues (nausea, diarrhea) are common. |
| SGLT2 Inhibitors | Reduce glucose reabsorption in the kidneys | Limited role; may not be effective in all individuals and should be used with caution. | Increased risk of urinary tract infections and ketoacidosis (especially if used alone without insulin) |
| DPP-4 Inhibitors | Increase incretin hormones to stimulate insulin release | Limited role; may not be effective in all individuals and should be used with caution. | Potential for mild gastrointestinal upset. |
Other Medications
Beyond insulin and oral medications, various other drugs can be incorporated into a Type 1 diabetes management plan. These additions often address specific complications or symptoms that may arise alongside the condition, or enhance the overall effectiveness of the primary treatment regimen. Careful consideration of potential benefits and risks is crucial when adding any medication to a patient’s existing treatment plan.
Additional Medications for Blood Pressure and Cholesterol
High blood pressure and high cholesterol are common comorbidities associated with Type 1 diabetes. These conditions increase the risk of cardiovascular complications, a major concern for individuals with diabetes. Therefore, medications to manage these conditions are often prescribed alongside insulin or oral medications to reduce this risk.
- ACE Inhibitors and ARBs: These medications are frequently used to lower blood pressure. They help relax blood vessels, improving blood flow and reducing pressure. Examples include lisinopril and valsartan. Potential side effects include dizziness, lightheadedness, and a persistent cough (more common with ACE inhibitors). Interactions with other medications, such as potassium-sparing diuretics, should be carefully monitored.
- Statins: These drugs are widely used to lower cholesterol levels. They work by inhibiting the production of cholesterol in the liver. Examples include atorvastatin and simvastatin. Potential side effects include muscle pain and liver problems. Interactions with other medications, particularly those affecting liver function, should be carefully monitored.
Medications for Diabetic Neuropathy
Diabetic neuropathy, a common complication of diabetes, can cause nerve damage leading to pain, numbness, or tingling. Certain medications can help manage these symptoms.
- Antidepressants (e.g., duloxetine): These medications can reduce nerve pain and improve overall well-being. Duloxetine, for instance, is often prescribed for its effectiveness in managing neuropathic pain. Potential side effects include nausea, drowsiness, and sexual dysfunction. It’s important to discuss potential interactions with other medications, particularly those affecting serotonin levels.
- Anticonvulsants (e.g., pregabalin): These medications are sometimes used to manage nerve pain, often associated with diabetic neuropathy. Pregabalin can be effective in reducing nerve pain, but potential side effects include dizziness, swelling, and weight gain. Interactions with other medications, including those that affect the central nervous system, should be carefully considered.
Other Medications for Specific Symptoms
Other medications might be used to address specific symptoms or complications associated with Type 1 diabetes. This includes, but is not limited to, medications for gastroparesis, kidney problems, or depression. The rationale behind these additions depends on the specific needs of the individual.
| Medication Category | Use Cases | Potential Side Effects | Interactions |
|---|---|---|---|
| Gastroparesis Medications | Slowing gastric emptying to improve digestion and absorption of food | Nausea, vomiting, constipation, abdominal pain | Can interact with medications that affect gastric motility or absorption |
| Kidney Disease Medications | Managing kidney function and preventing further damage | Potential electrolyte imbalances, nausea, fatigue | Can interact with other blood pressure medications or diuretics |
| Anti-anxiety/Mood Stabilizers | Managing anxiety or depression, common comorbidities with Type 1 diabetes | Drowsiness, dizziness, weight gain | Potential interactions with other medications, including insulin |
Medication Selection and Considerations
Choosing the right diabetes medications is a crucial aspect of managing type 1 diabetes effectively. It’s a personalized journey, and the best approach depends on various factors unique to each individual. Understanding these factors, along with the role of the healthcare team, empowers individuals to make informed decisions about their treatment plan.Selecting appropriate medications involves more than just considering the available options.
Looking for a complete guide to type 1 diabetes medications? It’s a complex topic, but understanding the different options is crucial. For example, if you’re also dealing with skin conditions like dry skin or atopic dermatitis, you might want to check out ask an expert dry skin or atopic dermatitis for some helpful advice. Ultimately, a comprehensive understanding of your specific needs is key when managing type 1 diabetes.
It necessitates a holistic approach, taking into account individual needs, preferences, and lifestyle. The goal is to achieve optimal blood glucose control while minimizing potential side effects and improving overall quality of life. The healthcare team plays a vital role in this process.
Factors Influencing Medication Choice
Individual factors significantly impact medication selection. These include age, lifestyle, other health conditions, and personal preferences. For example, a young, active individual may have different needs than an older adult with additional health concerns. The complexity of the patient’s situation, their daily routines, and their personal preferences all influence the selection process.
Patient Needs and Preferences
Understanding patient needs and preferences is paramount in medication selection. Patients should actively participate in the decision-making process. Open communication with the healthcare team about their lifestyle, dietary habits, and activity levels is essential. This allows for the development of a treatment plan that aligns with their personal goals and expectations. This collaborative approach ensures that the chosen medications support their overall well-being.
I’m diving deep into a complete guide to type 1 diabetes medications, which is a crucial resource for anyone managing this condition. While researching different treatment options, I stumbled upon an interesting question: are 3-month allergy shots safe? This article delves into the safety and effectiveness of this approach, and it’s definitely worth a read. Ultimately, understanding the various medications and treatment options available for type 1 diabetes remains my primary focus.
Role of the Healthcare Team
The healthcare team, including doctors, nurses, and dietitians, plays a crucial role in guiding medication choices. Their expertise helps in evaluating individual needs and tailoring a personalized treatment plan. They provide guidance on potential side effects and offer support throughout the medication journey. This comprehensive approach ensures that the chosen medications are both effective and safe.
Questions to Ask Your Healthcare Provider
Patients should actively engage in discussions with their healthcare providers about medication choices. This involves asking pertinent questions to ensure a clear understanding of the recommended regimen. Some important questions include:
- What are the potential side effects of each medication?
- How will this medication affect my daily routine and lifestyle?
- What are the long-term implications of each medication choice?
- How will this medication interact with any other medications I’m currently taking?
- What are the alternatives if one medication doesn’t work well?
Medication Regimen Comparison
A table illustrating different medication regimens tailored to various patient profiles can aid in understanding the diverse options available:
| Patient Profile | Medication Regimen | Considerations |
|---|---|---|
| Young, active individual with stable blood glucose levels | Basal-bolus insulin regimen with continuous glucose monitoring (CGM) | Provides flexibility for lifestyle, but requires consistent monitoring and adjustment |
| Older adult with comorbidities and stable blood glucose levels | Simplified insulin regimen with frequent blood glucose monitoring | Reduces complexity and potential side effects, but requires close monitoring for changes |
| Individual with frequent blood glucose fluctuations and a busy lifestyle | Premixed insulin injections with close monitoring | Offers convenience, but requires meticulous blood glucose monitoring and adjustment |
| Individual with a history of hypoglycemia | Lower-dose insulin regimen with frequent blood glucose monitoring | Reduces risk of hypoglycemia, but requires consistent monitoring |
Potential Side Effects and Interactions

Navigating the world of Type 1 diabetes medications can feel like a balancing act. While these medications are crucial for managing blood sugar, understanding potential side effects and interactions is equally important. This section delves into the possible downsides and highlights the importance of proactive monitoring and open communication with your healthcare provider.
Common Side Effects of Different Medications
Different diabetes medications can produce a range of side effects. Understanding these potential issues empowers you to recognize them and promptly address them with your doctor. Some common side effects can include gastrointestinal issues, changes in appetite, or fluctuations in blood pressure. It’s crucial to note that the specific side effects and their severity can vary significantly based on the individual and the medication.
- Insulin: Common side effects of insulin include hypoglycemia (low blood sugar), weight gain, and allergic reactions. Hypoglycemia can manifest as shakiness, sweating, and dizziness. Proper dosage adjustments and consistent monitoring are essential.
- Oral Medications: Some oral medications may cause gastrointestinal upset, such as nausea, vomiting, or diarrhea. Others might lead to changes in appetite or weight. Consistent monitoring of blood glucose levels is crucial when starting or adjusting oral medications.
Importance of Monitoring for Side Effects
Regular monitoring is vital for detecting and managing any side effects promptly. This proactive approach ensures that any potential issues are addressed early, preventing them from escalating. Regular check-ups with your healthcare provider are critical for evaluating the effectiveness of the treatment and identifying any emerging side effects.
- Regular Blood Glucose Checks: Frequent blood glucose monitoring allows for early detection of hypoglycemia or hyperglycemia (high blood sugar), both of which can be signs of medication side effects.
- Symptom Awareness: Pay close attention to any unusual symptoms that may emerge after starting or adjusting medications. Documenting these symptoms and their severity can aid in discussions with your doctor.
Potential Interactions with Other Medications or Supplements
Certain medications and supplements can interact with Type 1 diabetes medications, potentially altering their effectiveness or increasing the risk of side effects. Always inform your doctor about all medications and supplements you are taking to avoid potential interactions.
- Examples of Interactions: Some medications that may interact with diabetes medications include certain blood pressure medications, diuretics, and some over-the-counter pain relievers. For example, certain blood pressure medications can increase the risk of hypoglycemia if taken with insulin. Similarly, some supplements can affect blood sugar levels, potentially requiring adjustments to your diabetes medication regimen.
- Importance of Disclosure: Full disclosure of all medications and supplements is crucial. This ensures your healthcare provider can assess potential interactions and adjust your treatment plan accordingly.
Table of Potential Side Effects and Management Strategies
This table provides a summary of potential side effects and suggests management strategies. Remember, this is not an exhaustive list and should not replace professional medical advice.
| Potential Side Effect | Management Strategy |
|---|---|
| Hypoglycemia | Carry glucose tablets or gels; adjust insulin dosage; monitor blood glucose levels frequently. |
| Hyperglycemia | Adjust insulin dosage; monitor blood glucose levels frequently; review diet and exercise regimen. |
| Gastrointestinal Upset | Take medication with food; consider over-the-counter antacids; adjust medication dosage as needed. |
| Allergic Reactions | Seek immediate medical attention; discontinue medication if necessary; consult with your doctor. |
| Weight Gain/Loss | Adjust insulin dosage; review diet and exercise regimen; consult with your doctor. |
Patient Education and Management: A Complete Guide To Type 1 Diabetes Medications
Empowering individuals with Type 1 diabetes involves more than just prescribing medications. Comprehensive patient education is crucial for effective self-management and achieving optimal health outcomes. This section details the vital role of education in navigating the complexities of medication use and fostering long-term adherence.
Importance of Patient Education
Thorough patient education regarding Type 1 diabetes medications is paramount. It equips individuals with the knowledge and skills necessary to make informed decisions about their care, promoting self-reliance and reducing the risk of complications. Patients who understand their medications, their potential side effects, and the importance of consistent use are better positioned to achieve and maintain glycemic control.
Key Information for Patients
A crucial aspect of patient education is providing clear and concise information about medication use. This includes details on dosage, timing, administration methods, and potential side effects. Patients should understand how their medications interact with other medications they may be taking, and be aware of signs and symptoms that warrant immediate medical attention. Specific examples include:
- Understanding Insulin Types: Explaining the different types of insulin (rapid-acting, short-acting, intermediate-acting, long-acting) and their respective functions in controlling blood glucose levels. This includes the typical timing of insulin administration relative to meals and the potential for variability in absorption and effect based on individual factors.
- Proper Injection Techniques: Demonstrating correct insulin injection techniques to minimize discomfort and ensure accurate absorption. This includes appropriate needle selection, injection site rotation, and disposal procedures.
- Recognizing Hypoglycemia and Hyperglycemia: Educating patients about the symptoms of low blood sugar (hypoglycemia) and high blood sugar (hyperglycemia), and emphasizing the importance of recognizing these symptoms early and taking appropriate action.
- Medication Interactions: Highlighting potential interactions between Type 1 diabetes medications and other medications or supplements that patients might be taking.
- Lifestyle Factors: Emphasizing the importance of lifestyle factors, such as diet, exercise, and stress management, in conjunction with medication regimens to achieve optimal blood glucose control.
Strategies for Promoting Adherence
Medication adherence is a significant challenge for many chronic conditions, including Type 1 diabetes. Strategies to enhance adherence encompass a variety of approaches, including:
- Regular follow-up appointments: Scheduling regular check-ups with healthcare providers for monitoring blood glucose levels and medication adjustments.
- Simplified medication regimens: Designing medication regimens that are as simple and manageable as possible to improve adherence.
- Support groups and resources: Connecting patients with support groups or online resources for peer-to-peer support and information sharing.
- Patient-centered communication: Encouraging open communication between patients and healthcare providers to address concerns and facilitate adjustments to the treatment plan.
Role of Self-Monitoring, A complete guide to type 1 diabetes medications
Self-monitoring plays a pivotal role in effectively managing Type 1 diabetes medications. Regular blood glucose monitoring allows patients to track their response to medications, adjust their regimen as needed, and identify patterns that might indicate a need for adjustments.
- Frequency of Monitoring: Providing guidance on the appropriate frequency of blood glucose monitoring, which can vary based on individual needs and treatment plan.
- Interpretation of Results: Educating patients on how to interpret blood glucose readings and understand how different factors, such as food intake and exercise, affect their levels.
- Troubleshooting: Providing strategies for troubleshooting issues with blood glucose control and how to communicate these issues with their healthcare provider.
Future Directions in Type 1 Diabetes Medications
The journey towards better type 1 diabetes management is constantly evolving. Current treatments, while effective, still have limitations. Researchers are actively exploring innovative approaches to improve treatment efficacy, reduce side effects, and potentially even find a cure. This exploration encompasses a wide range of strategies, from refining existing insulin delivery methods to investigating entirely new therapeutic targets.Ongoing research is focused on addressing the limitations of current treatments, such as the need for frequent insulin injections and the potential for long-term complications.
New advancements in technology and our understanding of the disease process are paving the way for more personalized and effective treatments. These advancements hold the potential to dramatically improve the lives of individuals living with type 1 diabetes.
Ongoing Research and Development in Insulin Delivery Systems
Continuous glucose monitoring (CGM) systems have significantly improved the lives of people with type 1 diabetes. However, the quest for even more accurate and convenient CGM technologies continues. Development efforts are focused on creating systems that are smaller, more discreet, and capable of providing real-time glucose readings with greater precision. These advancements aim to minimize the burden of frequent glucose checks and improve overall glucose control.
For instance, implantable CGM devices are in development, promising a more seamless and continuous monitoring experience. Further research is focused on integrating CGM data with automated insulin delivery systems.
Potential Future Trends in Medication Approaches
Several promising avenues are being explored for developing new treatments beyond insulin. These include therapies aimed at preventing or slowing the progression of beta cell destruction, potentially offering a preventive or disease-modifying approach. Also under investigation are immunomodulatory therapies, designed to regulate the immune system’s attack on beta cells. Stem cell therapies, aiming to regenerate beta cells, are also a promising area of research.
Potential Impact of New Technologies on Medication Management
Artificial intelligence (AI) is rapidly transforming healthcare, and type 1 diabetes management is no exception. AI algorithms can analyze large datasets of patient data, including CGM readings, lifestyle factors, and medication use, to predict future glucose levels and recommend personalized insulin doses. This approach allows for more dynamic and responsive insulin delivery, leading to improved glucose control and reduced risk of complications.
Further development in AI-powered diabetes management systems could potentially lead to more autonomous and personalized treatment plans.
Promising Research Areas
Several promising research areas are actively being pursued, with the potential to revolutionize type 1 diabetes management. These include:
- Development of novel insulin analogs: Researchers are exploring the creation of insulin analogs with improved properties, such as faster absorption or longer duration of action, to optimize blood glucose control.
- Immunomodulatory therapies: Studies are investigating drugs that can modulate the immune system’s response to beta cells, aiming to prevent or slow down the autoimmune attack responsible for the destruction of insulin-producing cells.
- Beta cell regeneration: Stem cell therapies are being explored as a potential means of regenerating beta cells, offering the possibility of a cure or disease-modifying approach.
Potential Future Developments in Type 1 Diabetes Medication
| Category | Description | Potential Impact |
|---|---|---|
| Insulin Delivery Systems | More advanced CGM systems, implantable sensors, and integrated AI-driven insulin pumps. | Improved glucose control, reduced hypoglycemia risk, and increased patient autonomy. |
| Disease-Modifying Therapies | Immunomodulatory drugs, stem cell therapies, and beta cell regeneration strategies. | Potential prevention or slowing of disease progression, or even a cure. |
| Personalized Medicine | AI-powered algorithms analyzing patient data for customized treatment plans. | Improved glucose control, reduced complications, and enhanced patient satisfaction. |
Final Conclusion
This comprehensive guide to type 1 diabetes medications aims to equip you with a solid understanding of the various treatment options available. By exploring the different categories of medications, their mechanisms, potential side effects, and selection considerations, you’ll gain valuable insights into managing this condition effectively. Remember, this information is for educational purposes only and should not replace professional medical advice.
Always consult with your healthcare team for personalized guidance.










