Atrial fibrillation drugs to avoid: This guide dives deep into understanding which medications can worsen AFib symptoms. We’ll explore the science behind why certain drugs exacerbate the condition, comparing and contrasting different drug classes and their potential impact on AFib patients. We’ll also look at the crucial role of patient-specific factors, including underlying health conditions, and discuss alternative treatment options to manage AFib effectively.
Understanding which medications to avoid is crucial for managing atrial fibrillation (AFib). This isn’t just about avoiding side effects; it’s about preventing the worsening of AFib symptoms and potentially improving overall health outcomes. By recognizing the potential risks and interactions of various drugs, individuals and healthcare professionals can make informed decisions to optimize AFib treatment plans.
Introduction to Atrial Fibrillation (AFib): Atrial Fibrillation Drugs To Avoid

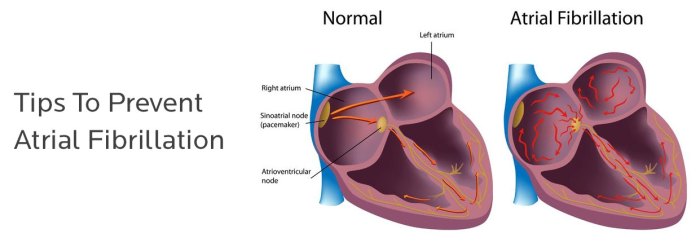
Atrial fibrillation (AFib) is a common heart rhythm disorder characterized by irregular and often rapid heartbeats. The atria, the upper chambers of the heart, quiver instead of contracting smoothly, leading to inefficient blood pumping. This irregularity can increase the risk of blood clots forming in the heart, potentially traveling to other parts of the body and causing serious complications like stroke.Understanding the causes of AFib is crucial for effective management.
Ever wondered about atrial fibrillation drugs to avoid? Some medications can actually worsen your condition, impacting your overall well-being. Understanding the nuances of different treatments, like exploring the differences between stool softeners and laxatives, can be surprisingly helpful. For a deeper dive into the world of digestive health, check out this helpful guide on stool softener vs laxative what s the difference.
Ultimately, consulting your doctor is crucial for pinpointing the best approach to managing atrial fibrillation and avoiding potentially harmful drugs.
While some cases are triggered by underlying conditions like high blood pressure, heart valve disease, or hyperthyroidism, others may arise without a readily identifiable cause. Age, family history, and lifestyle factors like smoking and excessive alcohol consumption can also contribute to the development of AFib.Proper medication management is paramount in treating AFib. Medications play a vital role in controlling heart rate, preventing blood clots, and addressing underlying conditions that may be contributing to the condition.
This approach is crucial to reducing the risk of serious complications and improving overall heart health.Various treatment options are available for AFib, including medications, catheter ablation, and surgery. Medications, often the first line of treatment, aim to restore a normal heart rhythm, control heart rate, and prevent blood clots. Catheter ablation involves using heat or cold to destroy the abnormal pathways in the heart that cause the irregular rhythm.
Surgery, in some cases, may be considered as a last resort to address structural issues contributing to AFib.
Types of Atrial Fibrillation
Different types of AFib exist, each with varying characteristics and treatment approaches. Understanding these distinctions is essential for appropriate patient management.
| Type | Characteristics |
|---|---|
| Paroxysmal AFib | Episodes of AFib that start and stop spontaneously, often lasting for a short duration (typically less than 7 days). These episodes may resolve without intervention, or require medication to restore normal rhythm. |
| Persistent AFib | AFib that lasts longer than 7 days and does not spontaneously convert to a normal sinus rhythm. Treatment often involves medications to control heart rate and rhythm, or procedures like catheter ablation. |
| Permanent AFib | AFib that persists despite treatment attempts, often after multiple interventions. Management focuses on controlling heart rate and symptoms to prevent complications like stroke. |
Identifying Medications to Avoid
Navigating atrial fibrillation (AFib) often involves careful medication management. Certain drugs, while essential for other conditions, can trigger or worsen AFib symptoms. Understanding these potential triggers is crucial for preventing complications and maintaining a healthy heart rhythm. This section dives deep into medications known to exacerbate AFib and explores the underlying mechanisms.
Common Medications Exacerbating AFib
Many medications, seemingly unrelated to the heart, can indirectly affect the electrical signals in the heart, potentially leading to or worsening AFib. These include some over-the-counter and prescription drugs. Understanding these connections allows for proactive communication with healthcare providers to identify and mitigate risks.
- Certain diuretics (water pills): Diuretics can lead to electrolyte imbalances, particularly potassium depletion, which can increase the risk of AFib. This is due to the direct effect on the electrical conductivity within the heart, increasing the risk of abnormal heart rhythms.
- Some medications for high blood pressure:
- Beta-blockers: While often used to control high blood pressure, some beta-blockers can slow the heart rate too much, which can sometimes trigger AFib. The precise mechanisms involve modulating the autonomic nervous system’s influence on the heart.
- Calcium channel blockers: Like beta-blockers, some calcium channel blockers can influence the heart’s electrical conduction pathways, potentially leading to AFib in susceptible individuals.
- Anticholinergics: These drugs, often used for various conditions, can disrupt the autonomic nervous system’s control over heart rate. This interference can create conditions favorable to AFib development.
- Some medications for psychiatric conditions:
- Certain antidepressants:
- Antipsychotics:
- Stimulants:
- Some medications for other conditions:
- Asthma medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These can indirectly affect heart function and electrolytes, potentially contributing to AFib in certain individuals.
- Medications for thyroid disorders:
Mechanisms of Negative Impact
The mechanisms by which these medications worsen AFib are multifaceted. They can affect electrolyte balance, alter the heart’s electrical conduction, and influence the autonomic nervous system’s control over heart rate. Understanding these complex interactions is key to patient management.
- Electrolyte Imbalances: Diuretics can deplete potassium, affecting the heart’s electrical stability and increasing the likelihood of AFib.
- Altered Conduction Pathways: Certain drugs can directly or indirectly affect the electrical pathways in the heart, creating conditions that favor the development of abnormal heart rhythms, including AFib.
- Autonomic Nervous System Modulation: Some medications interfere with the autonomic nervous system’s regulation of heart rate. This disruption can lead to an abnormal heart rhythm.
Comparison of Drug Classes
Different drug classes can impact AFib in varying ways. Understanding these differences helps in tailoring treatment strategies and mitigating potential risks.
- Beta-blockers vs. Calcium Channel Blockers: Both classes can affect heart rate and conduction, but their mechanisms and potential side effects differ. Beta-blockers primarily affect sympathetic nervous system activity, while calcium channel blockers primarily affect the electrical conduction pathways.
Medication Interactions Table
A comprehensive table outlining potential side effects and interactions is essential for healthcare professionals and patients. This table highlights the importance of careful consideration when prescribing medications for AFib patients.
| Medication Class | Potential Side Effects (Related to AFib) | Possible Interactions with AFib Treatment |
|---|---|---|
| Diuretics | Electrolyte imbalances (e.g., hypokalemia) | May increase risk of AFib or worsen existing AFib |
| Beta-blockers | Bradycardia (slow heart rate) | May mask symptoms of AFib or worsen existing AFib in some cases |
| Calcium Channel Blockers | Bradycardia, AV block | Potential interaction with AFib management |
| Anticholinergics | Heart rate variability | May interfere with the effectiveness of AFib medications |
| NSAIDs | Electrolyte disturbances | Potential to exacerbate existing AFib or contribute to new onset |
Drug Interactions and Considerations
Understanding potential drug interactions is crucial for managing atrial fibrillation (AFib) effectively. Many medications used to treat AFib, or other conditions, can interact negatively with each other, leading to adverse effects and complications. Careful consideration of these interactions is vital for maintaining patient safety and optimizing treatment outcomes.Careful monitoring of patients taking multiple medications is essential. A thorough medication history, including over-the-counter drugs, supplements, and herbal remedies, is necessary for a complete picture of potential interactions.
Clinicians should collaborate closely with patients to ensure that they understand the potential risks and benefits of all prescribed medications.
Potential Drug Interactions
Drug interactions can significantly impact the efficacy and safety of AFib medications. These interactions can alter the metabolism or excretion of drugs, leading to either increased or decreased drug levels in the body. This can result in unpredictable responses, and sometimes dangerous side effects.
Steering clear of certain atrial fibrillation drugs is crucial, but equally important is understanding broader health risks, like those linked to PFAS forever chemicals. Learning about the sources and how to avoid them is vital, as detailed in this informative guide on pfas forever chemicals health risks sources how to avoid. Ultimately, staying informed about potential risks, from PFAS to medications, empowers you to make the best choices for your health when it comes to atrial fibrillation management.
Examples of Interactions to Avoid
Certain combinations of medications can pose significant risks for patients with AFib. For instance, some medications used to treat high blood pressure can interact negatively with AFib medications like digoxin, potentially leading to dangerously low potassium levels. Similarly, certain antibiotics or antifungal medications can alter the effectiveness of blood thinners prescribed for AFib, increasing the risk of blood clots.
These interactions can lead to serious complications, including heart failure, stroke, and kidney damage.
Steering clear of certain atrial fibrillation drugs is crucial, as some can unexpectedly worsen existing health conditions. For example, some medications can exacerbate side effects of diabetes, which can lead to complications like heart problems. Understanding the potential interplay between these conditions is key when discussing treatment options with your doctor, so you can find the safest and most effective atrial fibrillation drugs for your individual needs.
Consulting a healthcare professional is always recommended to avoid potential adverse reactions. side effects of diabetes
Individual Patient Factors
Individual patient factors play a critical role in determining appropriate medication choices and dosages. Age, kidney function, and liver function all influence how the body processes medications. Older adults, for example, often have reduced kidney function, which can affect the clearance of certain drugs. Patients with liver disease may metabolize medications differently, requiring adjustments to dosages.
Impact of Kidney and Liver Function
Kidney and liver function directly impact the excretion and metabolism of medications. Reduced kidney function can lead to a buildup of medication in the body, potentially resulting in toxicity. Similarly, liver dysfunction can impair the body’s ability to process and eliminate certain drugs, leading to adverse reactions. Clinicians must consider these factors when selecting and adjusting dosages for AFib medications.
Medication Interactions Table
| Common Medication | Potential Interaction with AFib Drugs | Explanation |
|---|---|---|
| Amiodarone | Many drugs, including statins, calcium channel blockers, and some antibiotics | Amiodarone can prolong the QT interval, increasing the risk of serious arrhythmias. Some medications can exacerbate this effect. |
| Digoxin | Diuretics, antacids, and some antibiotics | These drugs can alter the absorption or excretion of digoxin, potentially leading to toxicity or reduced efficacy. |
| Warfarin | NSAIDs, antibiotics, and some herbal supplements | These drugs can increase or decrease the anticoagulant effect of warfarin, increasing the risk of bleeding or clotting. |
| Beta-blockers | Other medications that affect heart rate or blood pressure | Combinations of beta-blockers with certain drugs can lead to excessive slowing of the heart rate, potentially causing bradycardia or other complications. |
Patient Considerations and Risk Factors
Choosing the right AFib medication involves careful consideration of individual patient factors. Underlying health conditions, lifestyle choices, and age all play a significant role in determining the best course of treatment. Understanding these nuances is crucial for maximizing treatment effectiveness and minimizing potential risks.Patient-specific factors significantly influence the selection and management of AFib medications. The goal is to find the most effective and safest approach for each individual, balancing potential benefits against potential side effects.
This requires a comprehensive understanding of the patient’s overall health picture, beyond just the AFib itself.
Underlying Health Conditions
Different medical conditions can impact the effectiveness and safety of AFib medications. For example, kidney or liver impairment may necessitate adjustments to drug dosages or even the selection of different medications. These adjustments are essential to prevent adverse reactions and ensure the treatment remains safe and effective.
- Kidney Disease: Many AFib medications are eliminated by the kidneys. Patients with impaired kidney function may need lower doses or alternative medications to avoid potentially toxic buildup in the body. A creatinine clearance test helps determine the level of kidney function.
- Liver Disease: The liver plays a role in metabolizing many medications. Patients with liver issues might require lower doses or different drugs, as their bodies might not process the medication as efficiently. Liver function tests (LFTs) are used to assess liver health.
- Heart Failure: Patients with heart failure may have reduced tolerance to certain AFib medications. The choice of medication often involves careful consideration of potential interactions with heart failure treatments.
- Hypertension: High blood pressure can increase the risk of side effects from some AFib medications. A thorough assessment of blood pressure management is crucial when prescribing AFib drugs.
- Thyroid Issues: Thyroid disorders can influence the risk of developing AFib and may also affect how the body metabolizes AFib medications. Regular thyroid function tests are important.
Patient Age and Elderly Considerations
Elderly patients often have a higher prevalence of comorbidities, including kidney or liver disease, and are more susceptible to the side effects of medications. This necessitates careful medication selection and monitoring to prevent complications.
- Reduced Organ Function: Older adults often experience a decline in kidney and liver function, making them more sensitive to the side effects of certain medications. Lower doses or alternative medications are often necessary to prevent accumulation of the drug in the body.
- Increased Risk of Adverse Reactions: Elderly patients are more prone to experiencing adverse reactions to medications. This includes a higher risk of falls, cognitive impairment, and other complications. Careful monitoring is essential to address these issues early on.
- Polypharmacy: Elderly patients are more likely to be taking multiple medications for various conditions. This increases the potential for drug interactions and complications. A comprehensive medication reconciliation is crucial.
Lifestyle Factors
Lifestyle choices, such as diet, exercise, and alcohol consumption, can impact medication effectiveness and safety. These factors can also influence the risk of AFib itself.
- Diet and Nutrition: A balanced diet rich in fruits, vegetables, and whole grains can support overall health and may influence the effectiveness of AFib medications. Excessive sodium intake can negatively affect blood pressure and increase the risk of side effects.
- Exercise and Physical Activity: Regular exercise can help manage blood pressure, improve heart health, and potentially reduce the need for certain AFib medications. Physical activity also reduces the risk of several other health problems.
- Alcohol Consumption: Excessive alcohol consumption can exacerbate AFib and interact with some medications. Moderation is crucial for patients taking AFib medications.
Specific Patient Scenarios
Careful consideration of individual circumstances is vital. A patient with a history of severe liver disease might require a different AFib medication than one without such a condition. Examples of scenarios where specific medications should be avoided include:
- Patient with severe kidney disease: Medications primarily eliminated by the kidneys should be avoided or used with extreme caution and close monitoring.
- Patient with known allergy to a specific medication component: Avoidance of the specific medication is mandatory.
- Patient with a history of significant drug interactions: Careful consideration of potential interactions with existing medications is essential.
Alternative Treatments and Management Strategies
Beyond medication, a holistic approach to managing atrial fibrillation (AFib) often yields significant benefits. This involves understanding that AFib is not just a medical condition but a potential reflection of broader health patterns. Addressing underlying health factors, adopting healthy lifestyle choices, and exploring non-pharmacological interventions can contribute substantially to symptom reduction and overall well-being.A multifaceted strategy encompassing medication, lifestyle adjustments, and non-pharmacological interventions is often the most effective approach to manage AFib.
This comprehensive approach acknowledges the interconnectedness of various factors influencing AFib and promotes a more personalized and proactive approach to care.
Lifestyle Modifications
Adopting healthy lifestyle choices is a cornerstone of AFib management. These modifications can complement medication and contribute to improved heart health and reduced AFib episodes. These choices encompass diet, exercise, stress management, and sleep hygiene.
- Dietary Changes: A balanced diet rich in fruits, vegetables, and whole grains, coupled with a reduction in processed foods, saturated fats, and excessive sodium intake, can significantly improve cardiovascular health. Reducing alcohol consumption can also contribute to better AFib control. Examples of dietary strategies include adopting a Mediterranean-style diet, which emphasizes fruits, vegetables, whole grains, and healthy fats.
- Regular Exercise: Engaging in regular physical activity, even moderate exercise, can significantly reduce AFib risk. Physical activity promotes cardiovascular health and strengthens the heart’s ability to regulate its rhythm. Examples include brisk walking, swimming, cycling, or any activity that elevates your heart rate for at least 30 minutes most days of the week.
- Stress Management Techniques: Chronic stress can exacerbate AFib symptoms. Stress-reduction techniques like yoga, meditation, or deep breathing exercises can help manage stress levels and contribute to improved heart health. These techniques can be particularly beneficial for individuals experiencing high stress levels, offering a proactive approach to managing potential triggers.
- Adequate Sleep: Ensuring sufficient sleep plays a crucial role in maintaining overall health and cardiovascular well-being. A consistent sleep schedule, a relaxing bedtime routine, and a comfortable sleep environment can significantly impact AFib symptoms. Adequate sleep contributes to better heart rhythm regulation.
Non-Pharmacological Interventions
Non-pharmacological interventions play a vital role in AFib management. These interventions are not intended to replace medication but rather to complement them and improve overall well-being. They encompass various approaches, each with unique mechanisms and potential benefits.
- Electrical Cardioversion: This procedure involves using electrical impulses to restore a normal heart rhythm. It’s a potentially effective method, but its effectiveness and suitability depend on individual factors, including the type and duration of AFib episodes.
- Catheter Ablation: This procedure involves using heat or cold to destroy the abnormal heart tissue responsible for causing AFib. It’s a more invasive approach than electrical cardioversion, but it may offer long-term solutions for some individuals with persistent AFib.
- Lifestyle Modification Impact Comparison: The effectiveness of non-pharmacological approaches can vary significantly. For example, while dietary changes can improve overall cardiovascular health and potentially reduce AFib episodes, the impact of electrical cardioversion or catheter ablation is more direct and targeted at restoring the heart’s rhythm.
Lifestyle Changes and Potential Benefits for AFib Management
| Lifestyle Change | Potential Benefits for AFib Management |
|---|---|
| Balanced Diet | Improved cardiovascular health, reduced risk of other health problems, potentially decreased AFib episodes. |
| Regular Exercise | Improved heart function, reduced stress, better overall health, potentially reduced AFib episodes. |
| Stress Management Techniques | Reduced stress levels, improved overall health, potentially reduced AFib episodes. |
| Adequate Sleep | Improved cardiovascular health, better heart rhythm regulation, potentially reduced AFib episodes. |
Specific Examples of Drugs to Avoid
Knowing which medications can exacerbate or trigger atrial fibrillation (AFib) is crucial for effective management. Avoiding these drugs can significantly improve a patient’s quality of life and reduce the risk of complications. This section details specific examples, their mechanisms of action, potential side effects, and their implications for AFib patients.
Specific Medications and Their Risks
Certain medications can inadvertently worsen AFib by impacting the heart’s electrical system or increasing the risk of other conditions that contribute to AFib. Understanding the underlying mechanisms helps patients and healthcare providers make informed decisions.
- Certain Diuretics: Loop diuretics, such as furosemide, and thiazide diuretics, can sometimes induce or worsen AFib, particularly in susceptible individuals. These diuretics can alter electrolyte balance, affecting the heart’s electrical conductivity and increasing the risk of arrhythmias. Possible side effects include dehydration, hypokalemia (low potassium), and hyponatremia (low sodium), all of which can contribute to AFib.
- Some Anticholinergics: Medications like certain antihistamines, some antidepressants, and some antipsychotics can interfere with the heart’s rhythm. These drugs block the action of acetylcholine, a neurotransmitter that plays a role in regulating heart rate and rhythm. This blockage can lead to a faster heart rate, increased automaticity of the heart, and a higher propensity for AFib. Potential side effects include dry mouth, blurred vision, constipation, and urinary retention, all of which can be problematic for patients with AFib.
- Certain Medications Affecting the Renin-Angiotensin-Aldosterone System (RAAS): While ACE inhibitors and ARBs are often beneficial for cardiovascular health, some patients with pre-existing heart conditions, including AFib, may experience a worsening of symptoms or an increased risk of AFib with these medications. These medications can impact the delicate balance of electrolytes and blood pressure, leading to potential disruptions in the heart’s electrical activity. Side effects can include hypotension (low blood pressure) and electrolyte imbalances, which can trigger or worsen AFib.
- Some Antibiotics: Certain antibiotics, particularly some types of quinolones, have been associated with an increased risk of AFib. The exact mechanism isn’t fully understood, but it’s thought that these medications can influence the electrical conduction system of the heart. Possible side effects can include QT prolongation, which can lead to potentially dangerous cardiac arrhythmias, including AFib.
Drug Class-Specific Risks for AFib Patients
The following table Artikels the potential risks associated with specific drug classes and their implications for AFib patients. It’s essential to note that this is not an exhaustive list and individual responses can vary significantly.
| Drug Class | Potential Risks | Implications for AFib Patients |
|---|---|---|
| Diuretics (e.g., loop, thiazide) | Electrolyte imbalances (hypokalemia, hyponatremia), dehydration | Increased risk of AFib, worsening of existing AFib |
| Anticholinergics (e.g., some antihistamines, antidepressants) | Increased heart rate, altered heart rhythm | Increased risk of AFib, worsening of existing AFib |
| RAAS Inhibitors (e.g., ACE inhibitors, ARBs) | Hypotension, electrolyte imbalances | Potential worsening of AFib symptoms, increased risk of AFib in susceptible individuals |
| Certain Antibiotics (e.g., quinolones) | QT prolongation, arrhythmias | Increased risk of AFib, potentially life-threatening cardiac arrhythmias |
Important Considerations for Healthcare Professionals
Navigating the complexities of atrial fibrillation (AFib) management requires a nuanced approach, particularly when considering medication choices. This involves not only understanding the specific drugs that should be avoided, but also the crucial role of thorough patient assessments and open communication in tailoring treatment plans. Healthcare professionals play a pivotal role in optimizing AFib patient outcomes by carefully considering the interplay of medications, potential interactions, and individual patient factors.Effective AFib management hinges on a proactive and individualized approach.
A comprehensive understanding of patient history, current health conditions, and lifestyle factors is essential for identifying potential medication risks. This proactive approach, coupled with open communication, fosters a collaborative environment where patients feel empowered to participate in their treatment decisions.
Thorough Patient Assessments for Medication Risks
A comprehensive patient assessment is paramount in identifying potential medication risks associated with AFib. This involves a detailed review of the patient’s medical history, including any pre-existing conditions, allergies, and previous adverse drug reactions. Furthermore, careful consideration of the patient’s current medications, including over-the-counter drugs and herbal supplements, is crucial. Identifying potential drug interactions or contraindications is vital to avoid adverse outcomes.
This assessment should also encompass the patient’s lifestyle, including dietary habits, alcohol consumption, and smoking history. These factors can influence medication efficacy and safety.
Significance of Open Communication Between Patients and Healthcare Providers
Open communication between patients and healthcare providers is critical in the selection of appropriate medications for AFib. Patients should feel empowered to ask questions, express concerns, and actively participate in the decision-making process. Clear and concise explanations of medication choices, potential side effects, and alternative treatment options are vital for informed consent. Healthcare professionals should actively listen to patient concerns and tailor their recommendations to individual needs and preferences.
Building trust and rapport facilitates a collaborative approach, optimizing adherence to treatment plans.
Best Practices for Medication Selection in AFib Patients
Optimizing medication selection in AFib patients involves adhering to evidence-based guidelines and considering individual patient characteristics. Prioritizing the use of FDA-approved medications for AFib management is crucial. Careful consideration of the patient’s specific AFib type, severity, and underlying health conditions is paramount. A holistic approach, incorporating patient preferences and lifestyle factors, is essential for successful treatment outcomes.
Regular monitoring of medication effectiveness and side effects is vital for adjusting the treatment plan as needed.
Key Factors for Healthcare Professionals to Consider, Atrial fibrillation drugs to avoid
| Factor | Description |
|---|---|
| Patient History | Thorough review of medical history, allergies, and previous adverse drug reactions. |
| Current Medications | Comprehensive list of all medications, including over-the-counter drugs and supplements. |
| Lifestyle Factors | Assessment of dietary habits, alcohol consumption, smoking history, and exercise routine. |
| Patient Preferences | Incorporating patient preferences and values into the treatment plan. |
| Drug Interactions | Identifying and mitigating potential drug interactions to minimize adverse effects. |
Ongoing Monitoring and Adjustments to Medication Regimens
Ongoing monitoring and adjustments to medication regimens are essential for optimal AFib management. Regular follow-up appointments allow for assessment of medication effectiveness, detection of side effects, and adjustment of the treatment plan as needed. This proactive approach enables healthcare professionals to identify and address any emerging concerns or complications in a timely manner. Regular monitoring of vital signs, electrocardiograms (ECGs), and blood tests are crucial for evaluating treatment response and ensuring patient safety.
Adapting the medication regimen based on the patient’s evolving needs and response to therapy is key.
Outcome Summary
In conclusion, navigating the complexities of AFib treatment often involves careful consideration of potential drug interactions and individual patient factors. This comprehensive guide provides a detailed overview of atrial fibrillation drugs to avoid, empowering both patients and healthcare providers with valuable knowledge. By understanding the potential risks and alternative treatment strategies, we can strive for better management and improved outcomes for those affected by this condition.









