Bacterial vaginosis in men, while surprisingly rare, is a condition that warrants attention. Understanding this often overlooked issue requires exploring the physiological differences between male and female genital tracts, and how these differences impact susceptibility to infection. This blog post will delve into the intricacies of bacterial vaginosis in men, from its pathophysiology to potential symptoms, diagnosis, and management.
While bacterial vaginosis (BV) is predominantly associated with women, it’s crucial to acknowledge its potential presence in men. This exploration will examine the unique microbial communities involved, potential risk factors, and the importance of accurate diagnosis and treatment. We’ll also discuss the similarities and differences in symptoms between men and women, and the crucial role of prevention in reducing the risk.
Introduction to Bacterial Vaginosis in Males
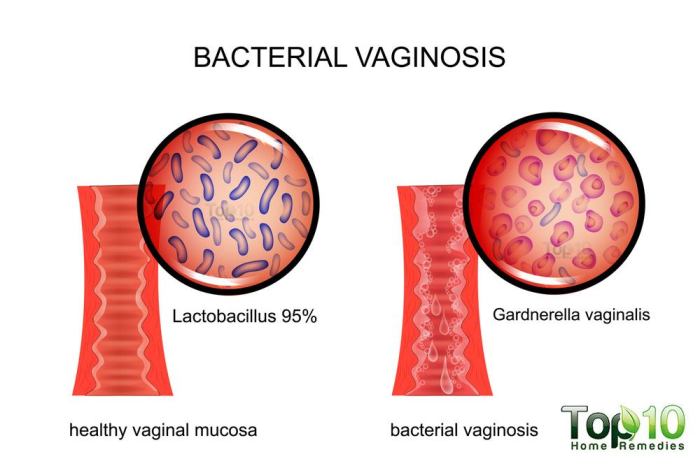
Bacterial vaginosis (BV) is a common vaginal infection in women, characterized by an imbalance in the normal vaginal bacteria. It’s typically caused by an overgrowth of certain bacteria, displacing the beneficial bacteria that normally maintain a healthy vaginal environment. This imbalance can lead to various symptoms, ranging from mild discomfort to more severe issues. Understanding BV in women is crucial for accurate diagnosis and treatment, which is often facilitated by recognizing its typical presentation.
Typical Presentation of BV in Women
Bacterial vaginosis in women typically presents with a thin, grayish-white vaginal discharge, often described as fishy smelling, especially after intercourse. This discharge may be accompanied by itching, burning, or discomfort during urination. Crucially, these symptoms can sometimes overlap with other vaginal conditions, such as yeast infections or trichomoniasis. Distinguishing BV from these conditions often requires careful examination and diagnostic testing by a healthcare professional.
Physiological Differences Between Male and Female Genital Tracts
The male and female genital tracts differ significantly in their physiology, which contributes to the rarity of BV in men. Women have a naturally acidic vaginal environment, a crucial factor in maintaining a healthy balance of vaginal flora. This acidic pH inhibits the overgrowth of harmful bacteria. The male urethra, on the other hand, has a more neutral pH and a different bacterial community.
This difference in environment makes the male genital tract less susceptible to the bacterial imbalance that characterizes BV.
Rarity of BV in Men
Bacterial vaginosis is exceptionally rare in men. The physiological differences between the male and female genital tracts, as previously mentioned, play a pivotal role. The unique environment of the male urethra, with its different bacterial flora and pH balance, makes it less hospitable to the bacteria associated with BV. Additionally, the limited research on BV in men highlights the rarity of this condition.
Comparison of Symptoms in Men and Women
| Characteristic | Women | Men |
|---|---|---|
| Discharge | Thin, grayish-white, fishy smelling | Potentially present, but often minimal and less noticeable |
| Odor | Often described as fishy | Potentially present, but often less pronounced or absent |
| Itching/Burning | Possible, ranging from mild to severe | Less likely, but possible in some cases |
| Pain during urination | Possible | Possible, but less frequent |
| Pain during intercourse | Possible | Possible, but less common |
This table summarizes the common symptoms of BV in women and men. Note that these symptoms can vary, and the absence of symptoms does not rule out the condition in either sex. It’s important to remember that the symptoms in men may be subtle and easily overlooked.
Pathophysiology of Bacterial Vaginosis in Males: Bacterial Vaginosis In Men
Bacterial vaginosis (BV) is a common condition primarily affecting women, characterized by an imbalance in the vaginal microbiome. However, the condition can also occur in men, albeit less frequently. Understanding the pathophysiology of BV in males is crucial for accurate diagnosis and effective treatment. This involves exploring the microbial communities, potential contributing factors, and mechanisms of inflammation.
Microbial Communities Associated with BV in Men and Women
The vaginal and urethral environments of both men and women harbor complex microbial communities. In healthy individuals, these communities are dominated by beneficial bacteria, which help maintain a balanced ecosystem. However, in cases of BV, an overgrowth of certain anaerobic bacteria disrupts this balance. Key differences exist between the microbial composition in healthy women and men. In women, a healthy vaginal environment usually contains Lactobacillus species, while in men, the urethral microbiome is more diverse, with a variety of facultative and anaerobic bacteria coexisting.
This difference in normal flora is a critical factor in considering the specific bacterial species implicated in BV in each sex.
Comparison of Bacterial Species Involved in BV in Both Sexes
While the specific bacterial species implicated in BV can vary, some commonalities exist. Gardnerella vaginalis is often identified in both women and men with BV. However, other bacteria, like Mobiluncus species and various anaerobic bacteria, may also contribute to the condition in men. This implies that the causative agents may overlap but not be identical, reflecting the differences in the normal flora of the female and male genital tracts.
Factors Contributing to BV in Men
Several factors may predispose men to developing BV. Lifestyle choices, such as poor hygiene practices, can disrupt the delicate balance of the urethral microbiome. Sexual activity plays a significant role, potentially leading to the introduction of bacteria from a partner with BV. The use of certain personal care products or exposure to chemicals may also contribute to dysbiosis.
Role of Sexual Activity in BV Transmission
Sexual activity is a potential avenue for the transmission of BV-associated bacteria in men. If a partner has BV, the exchange of fluids during sexual intercourse can introduce the problematic bacteria into the male genital tract. The frequency and nature of sexual activity, as well as the presence of other sexually transmitted infections, can influence the risk.
Mechanisms of Inflammation and Infection
The overgrowth of certain bacteria in the male genital tract can trigger an inflammatory response. The bacteria may produce toxins or other substances that irritate the tissues, leading to discomfort and potential infection. This response varies based on the specific bacteria involved and the individual’s immune system.
Factors Influencing the Onset and Progression of BV in Men
| Factor | Description |
|---|---|
| Hygiene | Poor hygiene practices can disrupt the balance of the urethral microbiome. |
| Sexual Activity | Exposure to BV-associated bacteria from a partner can lead to infection. |
| Lifestyle Factors | Certain lifestyle choices (e.g., use of harsh soaps) may contribute to dysbiosis. |
| Pre-existing Conditions | Conditions that compromise the immune system can increase susceptibility. |
| Urethral Microbiome | A pre-existing imbalance in the urethral microbiome can make an individual more vulnerable. |
Symptoms and Diagnosis of Bacterial Vaginosis in Males
Bacterial vaginosis (BV) is a common vaginal infection in women, but it can also affect men, albeit less frequently. Understanding the symptoms and diagnostic processes in men is crucial for early detection and appropriate treatment. Misdiagnosis is a significant concern due to the relative rarity of BV in males, and it’s essential to differentiate it from other, more common conditions.
Hey everyone, talking about bacterial vaginosis in men today. It’s a less common condition, but it can still affect guys. While there’s no direct link between BV in men and treating dandruff, some natural remedies like using coconut oil for dandruff efficacy and how to use it are gaining popularity. coconut oil for dandruff efficacy and how to use it is an interesting option for some skin concerns.
Regardless of its efficacy on dandruff, it’s important to remember that a doctor should be consulted for any health concerns, including bacterial vaginosis in men.
Common Symptoms in Males
Male BV often presents with a range of symptoms, some of which may be subtle or easily overlooked. Symptoms may not always be directly related to the genitals, potentially causing confusion with other issues. A thin, grayish-white discharge from the penis is a possible indicator. This discharge may have a fishy odor, particularly after sexual activity. Some men may experience irritation or burning sensations around the penis or groin area.
It’s important to note that these symptoms can be quite mild and vary significantly in severity. Furthermore, some men may experience no noticeable symptoms at all, making early detection challenging.
Potential for Misdiagnosis
The relatively low prevalence of BV in men often leads to misdiagnosis or delayed diagnosis. Physicians might initially suspect other more common conditions, such as urinary tract infections (UTIs) or sexually transmitted infections (STIs). The lack of clear, distinctive symptoms can contribute to the challenge of accurate diagnosis. Misinterpreting the symptoms as part of a routine infection can further hinder timely diagnosis.
Conditions Mimicking BV in Males
Several conditions can mimic the symptoms of BV in men, requiring careful differentiation by healthcare professionals. Urinary tract infections (UTIs) frequently exhibit similar symptoms, such as burning during urination and discharge. Certain sexually transmitted infections (STIs), like gonorrhea or chlamydia, can also present with similar discharge characteristics. Furthermore, some skin conditions or allergies can also cause irritation and discharge, making a correct diagnosis even more challenging.
Therefore, a comprehensive medical history and physical examination are crucial for differentiating BV from other potential causes.
Diagnostic Procedures
Diagnosing BV in men involves a multifaceted approach that considers clinical presentation, medical history, and appropriate laboratory tests. A physical examination of the penis and surrounding area is essential to evaluate for any visible signs of inflammation or discharge. Furthermore, a detailed medical history, including sexual history, helps to rule out other potential causes. Laboratory tests are critical in confirming the diagnosis.
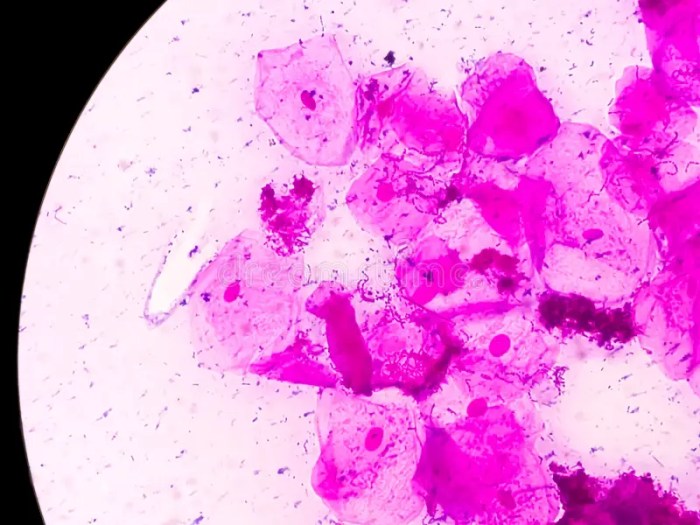
Laboratory Tests and Methods
A crucial aspect of diagnosing BV in men is the use of laboratory tests to identify the specific microorganisms associated with the condition. Microscopic examination of the discharge can reveal the presence of clue cells, which are characteristic of BV. Specific culture methods may be employed to isolate and identify the specific bacteria involved. Furthermore, a Gram stain can aid in differentiating BV from other infections based on the types of bacteria present.
The use of specific tests for other conditions, like STIs, is often necessary to rule them out.
Table of Diagnostic Methods
| Diagnostic Method | Sensitivity | Specificity | Description |
|---|---|---|---|
| Microscopic Examination | High | Moderate | Visual inspection of discharge for clue cells. |
| Gram Stain | High | Moderate | Identifies bacterial types present in the sample. |
| Culture | Moderate | High | Growth and identification of specific bacteria. |
| Nucleic Acid Amplification Tests (NAATs) | High | High | Identifies specific bacteria through genetic material. |
Note: Sensitivity and specificity values can vary depending on the specific laboratory and the method used.
Management and Treatment of Bacterial Vaginosis in Males
Bacterial vaginosis (BV) in men, though less common than in women, requires appropriate management to alleviate symptoms and prevent complications. Effective treatment hinges on accurate diagnosis and adherence to prescribed regimens. The underlying causes and contributing factors should be considered alongside the treatment plan to ensure long-term well-being.Understanding the nuances of BV treatment in men is crucial for successful management.
Similar to women, the goal is to restore the natural vaginal microbiome balance. However, the specific approach may differ based on individual circumstances.
Hey everyone! So, bacterial vaginosis, while more common in women, can sometimes affect men too. It’s important to get it checked out if you’re experiencing symptoms. Speaking of health, have you considered incorporating some flavorful spices into your diet for weight loss? Exploring options like ginger, turmeric, and cinnamon might help you reach your goals! spices for weight loss can be a delicious and potentially effective part of a balanced approach to wellness.
Regardless, if you’re a man experiencing any unusual discharge or discomfort, it’s always best to consult a healthcare professional for proper diagnosis and treatment.
Treatment Options for BV in Males
Treatment for BV in men primarily focuses on eliminating the overgrowth of anaerobic bacteria, often employing antibiotics. Similar to women, the choice of antibiotic and dosage depends on factors such as the severity of the infection, the patient’s overall health, and any potential drug interactions.
Common Antibiotics Used to Treat BV in Males
A variety of antibiotics are used to treat BV in men. Metronidazole is frequently prescribed due to its effectiveness in combating the causative bacteria. Tinidazole is another common option, often preferred for a single-dose administration. These antibiotics are typically well-tolerated, but potential side effects exist and should be considered.
Importance of Appropriate Antibiotic Selection and Dosage
Proper antibiotic selection is paramount for effective treatment. Choosing the right antibiotic, and the appropriate dosage, is crucial to minimize the risk of antibiotic resistance. A healthcare provider should tailor the treatment plan to the individual patient, taking into account factors like age, existing health conditions, and potential drug interactions.
Importance of Following Treatment to Prevent Recurrence
Adherence to the prescribed treatment regimen is essential to prevent recurrence of BV. Incomplete treatment can allow the causative bacteria to persist, potentially leading to a return of symptoms. Patients should complete the full course of antibiotics as directed by their healthcare provider, even if symptoms subside before the course is finished. This ensures that the infection is eradicated completely.
Table of Treatment Options
| Treatment Option | Potential Side Effects | Efficacy in Managing BV |
|---|---|---|
| Metronidazole | Nausea, vomiting, headache, metallic taste, and potentially a disulfiram-like reaction with alcohol | Generally effective, but adherence to the full course is crucial |
| Tinidazole | Nausea, vomiting, headache, metallic taste | Generally effective, often with a single-dose regimen |
| Clindamycin | Diarrhea, abdominal pain, nausea, and vaginal irritation in women | Can be effective, but requires careful monitoring due to potential side effects |
The efficacy of treatment depends on factors such as the individual’s response to the antibiotic and their adherence to the prescribed regimen. Regular follow-up appointments with the healthcare provider are vital to monitor progress and adjust the treatment plan as needed.
Prevention and Public Health Implications
Bacterial vaginosis (BV) in men, while less common than in women, can still cause discomfort and potentially impact sexual health. Understanding preventive measures and public health implications is crucial for promoting overall well-being and reducing the spread of this condition. Effective prevention strategies require a multifaceted approach encompassing safe sexual practices, hygiene, and public health initiatives.Preventing BV in men involves similar principles to preventing it in women, but with some nuances.
Effective prevention often relies on responsible sexual behaviors, good hygiene practices, and awareness campaigns. This section delves into these aspects, highlighting the importance of early detection and treatment for both individual and community health.
Preventive Measures for Reducing BV Risk
Understanding the risk factors and implementing preventative measures is crucial for reducing the incidence of BV in men. These strategies are designed to minimize exposure to potential causative agents and promote a healthy vaginal environment.
While bacterial vaginosis is primarily associated with women, it can affect men too. Understanding the potential complications of this condition is crucial, and it’s important to note that certain underlying health conditions, like internal shingles risks and complications here , can increase the risk of complications. Ultimately, men experiencing symptoms should consult a healthcare professional for accurate diagnosis and treatment.
- Safe Sexual Practices: Consistent and correct condom use significantly reduces the risk of transmitting BV. Using condoms during all sexual activities, including vaginal, anal, and oral sex, helps prevent the exchange of vaginal fluids and reduces exposure to potential pathogens. Open communication with partners about sexual health and practices is also essential.
- Hygiene Practices: Maintaining good hygiene, including regular cleansing of the genital area with mild soap and water, can help prevent the overgrowth of bacteria. Avoiding harsh soaps, douches, or scented products that can disrupt the natural vaginal flora is recommended. Proper hygiene practices, when coupled with safe sexual practices, can contribute significantly to minimizing the risk of BV.
- Early Detection and Treatment: Regular check-ups with a healthcare provider are vital. Early detection and treatment of BV can prevent potential complications and transmission to partners. Prompt medical intervention can ensure the best possible outcomes and minimize the impact of the infection.
Role of Education and Awareness Campaigns
Public awareness campaigns play a critical role in educating individuals about BV prevention and management. These campaigns aim to dispel myths, promote responsible sexual behavior, and emphasize the importance of seeking timely medical attention.
- Dissemination of Information: Educational materials, including brochures, websites, and social media campaigns, can effectively disseminate information about BV, its causes, symptoms, and prevention strategies. These resources can reach diverse audiences and empower individuals with knowledge to make informed decisions about their sexual health.
- Addressing Misconceptions: Awareness campaigns can address misconceptions about BV, emphasizing the importance of seeking medical advice for any unusual symptoms. This can help reduce stigma associated with the condition and encourage open communication about sexual health.
Comparison of Prevention Strategies for BV in Men and Women
While the underlying principles of BV prevention are similar for both men and women, some strategies may differ based on anatomical and physiological differences.
- Focus on Safe Sexual Practices: Condom use is critical for both men and women to reduce transmission risks. However, the specific details of safe sexual practices may vary based on the types of sexual activity.
- Emphasis on Hygiene: Maintaining good genital hygiene is important for both genders. However, the specific products and techniques used might vary based on individual needs and preferences.
Importance of Early Diagnosis and Treatment
Prompt diagnosis and treatment of BV are essential for preventing complications and reducing the risk of transmission.
- Minimizing Complications: Early intervention can prevent the development of more serious conditions. Untreated BV can lead to complications such as pelvic inflammatory disease (PID) in women. In men, it might lead to inflammation of the urethra or other related conditions.
- Reducing Transmission: Prompt treatment prevents the spread of BV to sexual partners. This is crucial for maintaining sexual health and preventing the cycle of infection.
Preventive Measures Table
| Preventive Measure | Effectiveness | Ease of Implementation |
|---|---|---|
| Consistent and correct condom use | High | Moderate |
| Regular genital hygiene with mild soap and water | Moderate | High |
| Open communication about sexual health with partners | High | High |
| Regular check-ups with a healthcare provider | High | Moderate |
Illustrative Cases
Understanding bacterial vaginosis (BV) in men requires careful consideration of potential presentations and diagnostic approaches. This section provides a hypothetical case study to illustrate the process of identifying and managing BV in males. While a formal diagnosis can only be made by a healthcare professional, this case study will help readers understand the potential symptoms, diagnostic considerations, and treatment plans involved.
Patient Presentation
A 28-year-old male presents to his primary care physician complaining of a thin, grayish-white discharge from his penis, accompanied by a slight burning sensation during urination. He reports no fever or other systemic symptoms. He denies any recent sexual activity or changes in hygiene practices. The patient’s medical history is unremarkable, and he denies any allergies. These symptoms suggest a possible infection, but further investigation is needed to determine the specific cause.
Diagnostic Approach
Given the patient’s presentation, the physician will first conduct a thorough history and physical examination. A focused history should inquire about potential risk factors for sexually transmitted infections (STIs) and other possible causes of urethritis. The physical examination will include a visual inspection of the penis and urethral meatus for any abnormalities or discharge. A sample of the discharge will be collected for laboratory analysis, including a Gram stain and wet mount microscopy.
These analyses will aid in identifying the presence of clue cells, a hallmark of bacterial vaginosis.
Differential Diagnoses, Bacterial vaginosis in men
Several conditions can present with similar symptoms to bacterial vaginosis in males. Differential diagnoses that should be considered include:
- Urinary tract infection (UTI): UTIs can cause urethral discharge and dysuria. The absence of systemic symptoms, such as fever, might make BV a more likely diagnosis.
- Sexually transmitted infections (STIs): STIs like gonorrhea and chlamydia can also cause urethritis. A comprehensive STI panel is often necessary to rule out these possibilities.
- Non-infectious urethritis: Allergic reactions or other inflammatory conditions can also cause urethral discharge and discomfort.
Treatment Plan
The treatment plan will be guided by the laboratory results. If bacterial vaginosis is confirmed, treatment will likely involve a course of oral or topical antibiotics. The choice of antibiotic and duration of treatment will be determined by the physician based on the specific causative agents and the patient’s response to therapy. Patient education about the importance of completing the full course of antibiotics is crucial to prevent recurrence.
Patient Progression
| Time Point | Action | Findings | Diagnosis | Treatment |
|---|---|---|---|---|
| Initial Visit | History and physical exam, discharge sample collection | Thin, grayish-white discharge, mild dysuria | Suspected BV | Gram stain, wet mount, STI panel ordered |
| 2-3 Days | Laboratory results | Positive for clue cells on wet mount, negative for other STIs | Bacterial Vaginosis Confirmed | Metronidazole 500 mg twice daily for 7 days prescribed |
| 1 Week | Follow-up visit | Patient reports improvement in symptoms | BV Resolved | Treatment completed |
Outcome Summary
In conclusion, bacterial vaginosis in men, though rare, presents a complex interplay of microbial factors, lifestyle considerations, and potential for misdiagnosis. This in-depth look at the topic highlights the need for greater awareness and understanding among healthcare professionals. Early diagnosis and appropriate treatment are key to managing the condition and preventing potential complications. Further research is crucial to better understand the nuances of BV in men and to improve diagnostic and treatment protocols.










