Bladder problems in endometriosis are a significant concern for many women living with this condition. Endometriosis, a disorder where tissue similar to the lining of the uterus grows outside the uterus, can cause a cascade of issues throughout the pelvic region. This often leads to inflammation, adhesions, and pressure, impacting the bladder’s function and causing various symptoms.
This comprehensive exploration delves into the multifaceted aspects of bladder problems in endometriosis, examining the spectrum of symptoms, diagnostic approaches, treatment options, and the profound impact on quality of life. We’ll also discuss preventative measures and the exciting avenues of current and future research in this area.
Introduction to Bladder Problems in Endometriosis
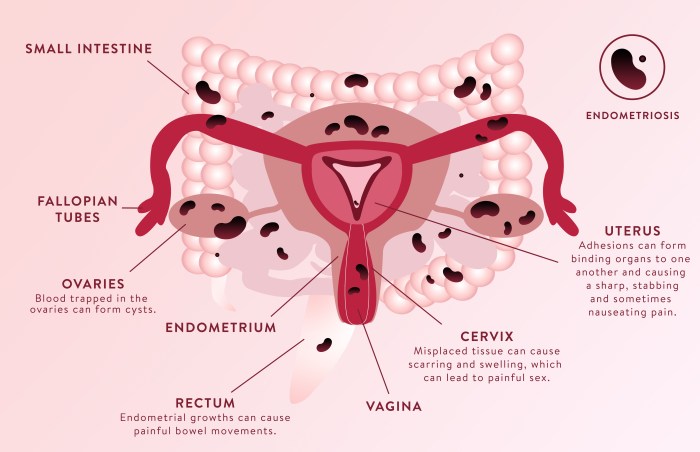
Endometriosis is a condition where tissue similar to the lining of the uterus (the endometrium) grows outside the uterus. This misplaced tissue can implant in various pelvic organs, leading to chronic inflammation, pain, and potentially significant disruptions in the normal function of these organs. The impact on the pelvic region is multifaceted, affecting not just reproductive organs but also surrounding structures like the bladder, bowel, and surrounding tissues.Endometriosis can affect the bladder in several ways.
The presence of endometrial tissue near or within the bladder can trigger inflammation. This inflammation can cause irritation and pain, leading to frequent urination and discomfort. Scar tissue, or adhesions, can form as a result of the chronic inflammatory process. These adhesions can bind the bladder to surrounding organs, potentially obstructing its normal function and causing pressure.
Furthermore, the growth of endometrial tissue can directly exert pressure on the bladder, affecting its capacity and function.The prevalence of bladder problems associated with endometriosis is not precisely quantifiable, as many cases are undiagnosed or misdiagnosed. However, studies suggest a significant correlation between endometriosis and bladder symptoms. The incidence varies based on factors like the extent of endometriosis, individual responses to the condition, and the presence of other related medical issues.
It’s crucial to note that while endometriosis can affect the bladder, not every individual with endometriosis will experience bladder problems. Individual experiences and symptom manifestation vary considerably.
Common Symptoms of Bladder Problems in Endometriosis
A range of symptoms can signal the involvement of the bladder in endometriosis. These symptoms can be subtle and easily overlooked, potentially leading to delayed diagnosis and treatment. Understanding the spectrum of potential symptoms is crucial for individuals experiencing pelvic pain or urinary issues.
| Symptom | Description | Frequency | Severity |
|---|---|---|---|
| Painful urination (dysuria) | Burning or sharp pain during urination | Variable; can be intermittent or constant | Mild to severe |
| Frequent urination (polyuria) | Increased need to urinate more often than usual | Common; often more frequent at night | Mild to moderate |
| Urgency | Sudden, intense urge to urinate | Frequent; can be incapacitating | Mild to severe |
| Nocturia | Frequent urination at night | Common; often a hallmark symptom | Mild to moderate |
| Hematuria (blood in urine) | Presence of blood in the urine | Occasional; can be associated with inflammation or trauma | Mild to moderate |
| Pelvic pain | Pain in the pelvic region, often worsening with bladder activity | Common; often a primary symptom | Mild to severe |
| Urinary retention | Difficulty emptying the bladder completely | Less frequent, but can be severe | Moderate to severe |
Symptoms and Diagnosis: Bladder Problems In Endometriosis
Navigating the complexities of endometriosis can be challenging, especially when bladder issues arise. Understanding the spectrum of symptoms and the diagnostic process is crucial for timely intervention and effective management. This section delves into the various symptoms associated with bladder dysfunction in endometriosis and Artikels the key differentiating factors from other conditions, alongside the diagnostic methods employed.The symptoms of bladder dysfunction in endometriosis can vary significantly, impacting daily life and potentially leading to misdiagnosis.
Recognizing these symptoms is the first step towards seeking appropriate medical care.
Symptom Spectrum
Bladder problems in endometriosis often manifest as a range of urinary symptoms. These symptoms can fluctuate in frequency, severity, and duration, making them challenging to diagnose. Some common symptoms include:
- Painful urination (dysuria): This can range from mild discomfort to severe pain, often described as sharp or burning. The pain may be constant or intermittent and may worsen with urination frequency or pressure on the bladder.
- Frequent urination (polyuria): This involves needing to urinate more often than usual, especially at night (nocturia). The frequency can be unpredictable and may be accompanied by a sense of urgency.
- Urgency to urinate: A strong and sudden urge to urinate that is difficult to control, leading to leakage (incontinence). This is often associated with a feeling of incomplete bladder emptying.
- Pelvic pain: Pain in the lower abdomen or pelvis, which can be sharp, cramping, or dull. This pain can be associated with or separate from bladder symptoms and can radiate to the lower back or groin.
- Blood in the urine (hematuria): Presence of blood in the urine, which can be a sign of irritation or inflammation in the urinary tract. This symptom can be subtle or noticeable, depending on the amount of blood.
- Urinary incontinence: Involuntary leakage of urine, which can be stress incontinence (leakage with exertion or physical activity), urge incontinence (leakage with a sudden urge), or mixed incontinence. This symptom can range from occasional to frequent and can significantly impact daily life.
Differentiating Factors
It’s crucial to distinguish bladder problems stemming from endometriosis from other conditions like urinary tract infections (UTIs), interstitial cystitis (IC), or prostatitis (in males). While these conditions can share similar symptoms, key differentiating factors can aid in diagnosis. For example, endometriosis often presents with pelvic pain, while UTIs typically have a sudden onset and are accompanied by fever and other systemic symptoms.
Dealing with bladder problems due to endometriosis can be tough. It’s frustrating, and while I’ve been researching potential solutions, I stumbled across an interesting article about preventative Botox. Does it really work for various ailments, including those related to bladder function? You can find out more about that in this article on preventative Botox and whether it’s a viable solution: preventative botox does it really work.
Ultimately, though, finding effective management strategies for bladder issues in endometriosis is still a top priority for me.
Furthermore, a thorough medical history and physical examination, alongside imaging studies, can help identify the underlying cause.
Diagnostic Methods
Accurate diagnosis is essential for effective treatment. A combination of methods is often used to assess bladder problems in endometriosis.
| Method | Description | Accuracy | Limitations |
|---|---|---|---|
| Pelvic Examination | A physical examination of the pelvic area to assess tenderness, masses, and other abnormalities. | Moderate | Subjective findings; may not detect all endometriosis lesions. |
| Ultrasound | Uses sound waves to create images of the pelvic organs. | High | May not visualize all endometriosis lesions, especially deep infiltrating endometriosis. |
| MRI (Magnetic Resonance Imaging) | Provides detailed images of the pelvic structures using magnetic fields and radio waves. | High | Can be expensive and time-consuming; may not be readily available in all locations. |
| Laparoscopy | A surgical procedure involving inserting a small camera into the abdomen to visualize the pelvic organs. | High | Invasive procedure; carries potential risks and complications. |
| Cystoscopy | A procedure to visualize the inside of the bladder. | Moderate | Useful for detecting bladder lesions or inflammation; may not identify endometriosis outside the bladder. |
Treatment Options and Management
Managing bladder problems stemming from endometriosis requires a multifaceted approach tailored to the individual’s specific situation and the severity of the condition. Treatment strategies often involve a combination of medical and surgical interventions, aiming to alleviate symptoms, reduce inflammation, and improve overall quality of life. Early intervention and proactive management are crucial for preventing long-term complications and maximizing treatment effectiveness.Effective treatment options for bladder endometriosis often involve a combination of approaches.
These strategies can be broadly categorized into surgical and non-surgical interventions. The choice of treatment depends on several factors, including the extent of endometriosis, the patient’s overall health, and their preferences.
Surgical Treatments
Surgical interventions are frequently employed to address bladder endometriosis. These procedures aim to remove or excise the endometrial tissue affecting the bladder, thereby reducing inflammation and alleviating pain and other symptoms. Laparoscopic surgery is a common minimally invasive approach, offering smaller incisions and faster recovery times compared to traditional open surgery.Surgical procedures can include:
- Laparoscopic excision or ablation: This involves using small incisions and specialized instruments to precisely remove or destroy the endometrial implants on the bladder. Recovery times are typically shorter than for open surgery. This approach can be effective in reducing pain and improving bladder function, but recurrence is possible in some cases.
- Open surgery: In more extensive cases, open surgery may be necessary to address severe endometriosis infiltrating the bladder wall. While offering more direct access for removal, it often leads to longer recovery times and larger scars.
- Cystoscopy: This procedure uses a thin, flexible tube with a camera to visualize the inside of the bladder. While not a surgical treatment in itself, it can aid in diagnosis and guide surgical interventions, allowing for targeted removal of endometrial tissue in some cases.
Non-Surgical Treatments
Non-surgical approaches often focus on symptom management and may be used in conjunction with or as a primary treatment strategy.
Bladder problems are a common symptom of endometriosis, often causing painful urination and frequent trips to the bathroom. Understanding how diet can impact various health conditions is key, and the dietary guidelines scientific report offers valuable insights into potential dietary strategies. These strategies, however, should be carefully considered in the context of managing bladder issues associated with endometriosis, as individual responses can vary greatly.
- Medications: Pain relievers like NSAIDs and hormonal therapies (e.g., birth control pills, GnRH agonists) can help manage pain and inflammation associated with bladder endometriosis. Hormonal therapies can suppress the growth of endometrial tissue, which can improve symptoms. However, these treatments may not always be sufficient for severe cases and may have potential side effects.
- Physical therapy: Pelvic floor physical therapy can help strengthen and relax muscles, which may alleviate pain and improve bladder function. Specific exercises and techniques may be taught to manage pain and improve bladder control.
- Dietary modifications: A balanced diet, including foods rich in anti-inflammatory properties, may help alleviate symptoms. Avoiding triggers that exacerbate bladder pain is crucial for symptom management. However, dietary changes alone may not be sufficient for complete symptom relief.
Comparison of Treatment Approaches
| Treatment | Benefits | Drawbacks | Considerations |
|---|---|---|---|
| Laparoscopic excision | Minimally invasive, faster recovery, smaller scars | Potential for recurrence, may not be suitable for extensive disease | Appropriate for mild to moderate cases; consider severity of endometriosis |
| Open surgery | Direct access for extensive removal | Longer recovery, larger scars, increased risk of complications | Reserved for severe cases where extensive tissue removal is necessary |
| Medications | Symptom management, potentially less invasive | Potential side effects, may not be sufficient for severe cases, possible recurrence | Effective for pain relief and inflammation control, may be used as adjunct |
| Physical therapy | Symptom management, improved bladder function | May not be effective for severe cases, requires commitment to exercises | Effective for improving muscle strength and function, may be used in combination with other treatments |
Impact on Quality of Life
Living with endometriosis and its associated bladder problems can significantly impact a person’s quality of life. The constant discomfort, unpredictable symptoms, and potential for complications can lead to feelings of frustration, anxiety, and isolation. Managing these issues often requires significant adjustments to daily routines and lifestyle choices. This can be challenging, and the impact on mental and emotional well-being should not be underestimated.Endometriosis-related bladder problems create a complex web of physical and emotional challenges that affect daily activities, relationships, and overall well-being.
The unpredictable nature of the pain, frequency of urination, and potential for infections can make it difficult to maintain a sense of normalcy. Coping strategies and support systems become crucial for navigating these difficulties and improving quality of life.
Physical Challenges
The physical manifestations of bladder problems in endometriosis can range from mild to severe, impacting various aspects of daily life. Frequent urination, urgency, pain during urination, and pelvic pain are common. These symptoms can interfere with work, social activities, and sleep, leading to fatigue and reduced energy levels. The need for frequent bathroom breaks can limit mobility and independence, impacting social interactions and personal relationships.
Furthermore, the risk of urinary tract infections (UTIs) is increased, adding another layer of discomfort and potential complications. The chronic pain associated with endometriosis can also impact overall physical well-being, leading to decreased mobility and participation in physical activities.
Emotional Challenges
The emotional toll of bladder problems in endometriosis is often overlooked but can be equally significant. The unpredictable nature of symptoms can lead to feelings of anxiety, frustration, and helplessness. The fear of pain, discomfort, and social embarrassment can impact self-esteem and confidence. The constant need to manage symptoms can also create stress and strain on personal relationships.
Dealing with bladder problems as a symptom of endometriosis can be incredibly frustrating. It’s a common complaint, but often overshadowed by other, potentially more serious, health concerns. While not directly related, understanding conditions like congestive heart failure vs heart failure can offer insight into how different medical issues can impact overall well-being. Ultimately, however, managing bladder problems due to endometriosis requires a personalized approach tailored to each individual’s unique experience.
The difficulty in getting accurate diagnoses and effective treatments can further exacerbate feelings of isolation and hopelessness.
Coping Strategies
Managing the impact of bladder problems on quality of life requires a multifaceted approach that combines medical interventions, lifestyle adjustments, and emotional support. Open communication with healthcare providers is crucial to develop a personalized treatment plan. Lifestyle modifications, such as dietary changes, stress management techniques, and regular exercise, can help alleviate symptoms and improve overall well-being. Support groups and counseling can provide valuable emotional support and coping mechanisms for individuals facing these challenges.
Table: Potential Emotional and Physical Effects of Bladder Problems in Endometriosis
| Aspect | Description | Impact | Mitigation strategies |
|---|---|---|---|
| Physical | Frequent urination, urgency, pain during urination, pelvic pain, fatigue, decreased mobility | Interference with work, social activities, sleep, reduced energy, limited mobility, increased risk of UTIs | Regular exercise, healthy diet, stress management techniques, pelvic floor exercises, medication |
| Emotional | Anxiety, frustration, helplessness, low self-esteem, social isolation, stress on relationships | Negative impact on mental health, strained relationships, difficulty coping with symptoms | Support groups, counseling, mindfulness practices, open communication with healthcare providers, relaxation techniques |
Illustrative Cases and Scenarios
Navigating the complexities of bladder problems in endometriosis often requires understanding diverse presentations. These cases highlight the varied symptoms, diagnostic challenges, and therapeutic approaches, emphasizing the importance of a personalized treatment plan. The intricate nature of the disease necessitates careful consideration of individual patient needs.
Case 1: The Gradually Progressive Case
This patient presented with mild urinary frequency and urgency, initially dismissed as a common ailment. Over several months, the symptoms worsened, including dysuria (painful urination) and pelvic pain. She experienced increasing difficulty voiding, sometimes requiring straining. Diagnostic imaging revealed significant endometrial implants around the bladder, compressing the surrounding tissues. Treatment involved a combination of pain management, hormonal therapies to reduce inflammation, and, ultimately, a minimally invasive surgical procedure to excise the implants.
The patient experienced significant improvement in bladder function and pain reduction post-surgery.
Case 2: The Acute Onset Case
A young woman experienced sudden, severe pelvic pain accompanied by intense urinary urgency and frequency. The pain was so intense that she required immediate medical attention. Physical examination revealed tenderness in the lower abdomen, and urine analysis showed no signs of infection. Ultrasound imaging showed extensive endometrial implants around the bladder, causing inflammation and significant pressure. The initial treatment focused on pain relief and anti-inflammatory medications.
Following a thorough diagnostic workup, a surgical intervention was deemed necessary. The outcome was positive with reduced pain and improved bladder function following the surgical removal of the implants.
Case 3: The Chronic Pain Case
This patient presented with chronic pelvic pain and urinary symptoms that persisted for years. The pain was often associated with menstrual cycles, and she experienced significant disruptions in daily life. The symptoms included urinary frequency, urgency, and occasional dysuria. Repeated attempts at medical management failed to significantly alleviate the pain. A detailed evaluation, including imaging studies and thorough history taking, indicated significant endometriosis affecting the bladder and surrounding structures.
The most appropriate treatment involved a multi-modal approach combining pain management, hormonal therapy, and surgical excision of the affected tissues. The patient reported significant improvement in pain management and quality of life after a comprehensive treatment plan.
Case Comparison Table
| Case | Symptoms | Treatment | Outcome |
|---|---|---|---|
| Case 1: Gradually Progressive | Mild urinary frequency/urgency, progressing to dysuria, straining | Pain management, hormonal therapy, minimally invasive surgery | Significant improvement in bladder function and pain reduction |
| Case 2: Acute Onset | Sudden, severe pelvic pain, intense urinary urgency/frequency | Pain relief, anti-inflammatory medications, surgical intervention | Reduced pain and improved bladder function post-surgery |
| Case 3: Chronic Pain | Chronic pelvic pain, urinary frequency/urgency, dysuria, cycle-related pain | Multi-modal approach: pain management, hormonal therapy, surgical excision | Significant improvement in pain management and quality of life |
Prevention and Early Detection
Understanding the risk factors and proactively seeking early detection are crucial for managing bladder problems associated with endometriosis. By recognizing potential triggers and implementing preventative measures, individuals can significantly improve their quality of life and potentially mitigate the severity of these complications. Early intervention can often lead to more effective treatment strategies and better long-term outcomes.Early detection and preventative strategies are not just about avoiding future issues; they’re about empowering individuals to take control of their health journey.
Proactive steps, coupled with open communication with healthcare providers, can pave the way for timely interventions and a more positive outlook.
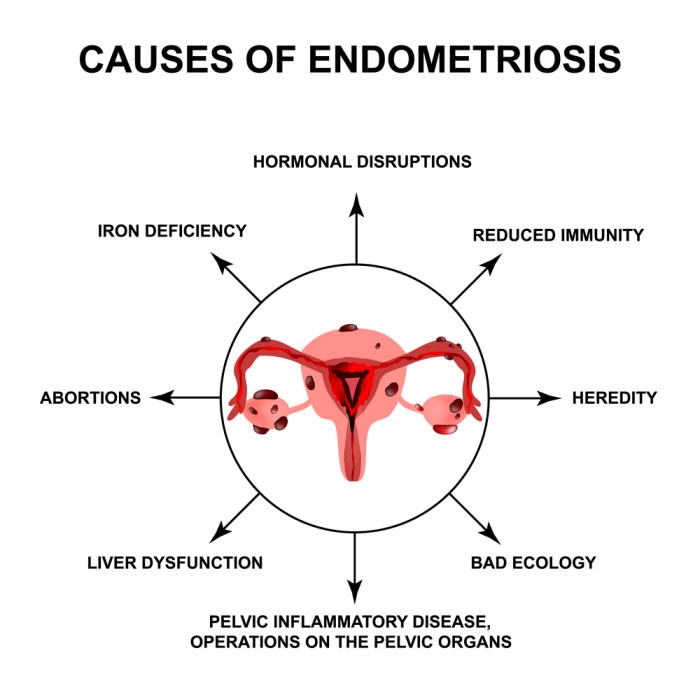
Risk Factors for Bladder Involvement in Endometriosis
Several factors can increase the likelihood of bladder problems developing in individuals with endometriosis. These include the location and extent of endometrial implants, hormonal fluctuations, and the presence of adhesions. Genetic predisposition may also play a role, although more research is needed to fully understand the interplay of these factors.
Importance of Early Detection, Bladder problems in endometriosis
Early detection is paramount in managing bladder problems related to endometriosis. Prompt diagnosis allows for tailored treatment plans and potentially prevents the progression of the condition, which can lead to more severe symptoms and complications. By catching the problem early, individuals can often avoid the need for more extensive and potentially invasive interventions in the future.
Preventative Measures
Taking proactive steps to minimize the risk of bladder complications is vital. These measures aim to reduce the impact of endometriosis on the bladder and promote overall well-being. Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques, plays a key role in overall health and potentially reducing the severity of endometriosis symptoms.
- Healthy Lifestyle Choices: A balanced diet rich in fruits, vegetables, and whole grains, combined with regular physical activity, can contribute to overall health and potentially reduce the risk of bladder issues. Stress management techniques like yoga, meditation, or deep breathing exercises can also help manage hormonal fluctuations and associated pain. Adequate hydration is essential for overall health and can help flush out toxins.
Maintaining a healthy weight can reduce strain on the bladder and pelvic organs.
- Regular Check-ups and Monitoring: Consistent monitoring with healthcare providers is crucial. Regular check-ups, including pelvic exams and discussions about symptoms, can allow for early detection of bladder issues related to endometriosis. This proactive approach can lead to timely intervention and management of the condition.
- Medication Management: While medication primarily focuses on symptom relief and pain management, some medications might also contribute to reducing the risk of certain complications. It is important to discuss potential risks and benefits with a healthcare provider. Following prescribed medication regimens and adhering to the dosage instructions carefully is vital.
- Surgical Interventions (when necessary): Minimally invasive surgical procedures can help remove endometrial implants and adhesions, thereby reducing the risk of bladder complications. However, surgical interventions are typically considered when conservative treatments fail to provide adequate relief. This approach requires careful consideration and discussion with a healthcare professional.
Preventative Measures Effectiveness Summary
| Measure | Description | Effectiveness | Considerations |
|---|---|---|---|
| Healthy Lifestyle Choices | Balanced diet, exercise, stress management | Potentially reduces inflammation, improves overall health | Individual results vary; may not prevent all complications |
| Regular Check-ups | Pelvic exams, symptom discussions | Enables early detection, allows for timely intervention | Requires consistent follow-up with healthcare provider |
| Medication Management | Following prescribed regimens | May help manage symptoms and potentially reduce complication risk | Individual response varies; potential side effects exist |
| Surgical Interventions | Removing endometrial implants/adhesions | Can significantly reduce complications in some cases | Considered a last resort, invasive procedure with potential risks |
Research and Future Directions
Understanding bladder dysfunction in endometriosis requires ongoing research to unravel the complex interplay of factors involved. Current research efforts are focused on identifying specific mechanisms driving the inflammation and fibrosis that contribute to bladder problems. This knowledge will be crucial for developing more targeted and effective therapies.The current state of research highlights promising avenues for future investigation. Identifying biomarkers for early detection and stratifying patients based on specific bladder pathology are key areas for further study.
This will pave the way for personalized treatment strategies tailored to individual patient needs.
Current Research Focus
Research into bladder endometriosis is exploring various avenues. One key area is investigating the role of immune responses in the development of bladder dysfunction. Studies are examining how immune cells contribute to inflammation and tissue damage, aiming to identify potential therapeutic targets. Another area of focus involves understanding the intricate interplay between hormonal fluctuations and bladder dysfunction, given the known influence of estrogen on the pelvic region.
This research seeks to determine how hormonal changes exacerbate bladder symptoms and identify potential hormonal interventions.
Areas Requiring Further Investigation
Several areas require further investigation to improve our understanding of bladder problems in endometriosis. A deeper understanding of the long-term effects of bladder dysfunction on patients’ overall health and quality of life is needed. The impact of these issues on future reproductive health and potential for pregnancy should also be examined. The development of non-invasive diagnostic tools that can accurately detect and assess the extent of bladder involvement in endometriosis is crucial.
This will help in making timely and informed treatment decisions.
Future Research Directions
Future research directions should focus on developing novel therapeutic strategies to effectively manage bladder dysfunction in endometriosis. Investigating the efficacy of minimally invasive surgical techniques for bladder endometriosis treatment, such as targeted laser ablation or endoscopic procedures, is warranted. Studies evaluating the effectiveness of novel drug therapies, such as immunomodulators or targeted therapies, should be conducted to reduce inflammation and fibrosis.
The development of personalized treatment plans, incorporating biomarkers and individual patient characteristics, is expected to lead to more effective outcomes. The incorporation of advanced imaging techniques, like MRI and ultrasound, can also improve diagnostic accuracy and monitoring of treatment response.
Emerging Trends and Technologies
Emerging trends in the field of endometriosis research include the utilization of advanced imaging technologies, like MRI and ultrasound, to improve diagnostic accuracy and monitor treatment response. The development of sophisticated biomarkers for early detection and disease stratification holds promise for personalized medicine approaches. Furthermore, the application of regenerative medicine techniques, like stem cell therapy, may provide new avenues for tissue repair and restoration of bladder function.
Research exploring the use of targeted drug therapies, potentially combined with non-invasive procedures, is a significant area of exploration. For instance, exploring the effectiveness of specific anti-inflammatory medications to manage bladder inflammation is an example of targeted drug therapy.
End of Discussion
In conclusion, bladder problems in endometriosis present a complex challenge requiring a multi-faceted approach to diagnosis and management. Understanding the various symptoms, diagnostic methods, and treatment options empowers both patients and healthcare professionals to navigate this complex condition. While significant progress has been made in research, ongoing investigation is crucial to refine treatments, improve patient outcomes, and ultimately enhance the quality of life for those affected.
The journey to better understanding and improved care continues.










