Risk factors for rheumatoid arthritis play a crucial role in understanding this complex autoimmune disease. This exploration delves into the multifaceted nature of RA risk, examining genetic predispositions, environmental influences, immunological factors, and lifestyle choices. We’ll also investigate how these factors intertwine to affect disease severity.
Rheumatoid arthritis, a chronic inflammatory condition, affects the lining of the joints, causing pain, swelling, and stiffness. Understanding the risk factors is essential for prevention, early detection, and better management strategies. This comprehensive overview explores the various elements that contribute to the development and progression of this debilitating disease.
Introduction to Rheumatoid Arthritis
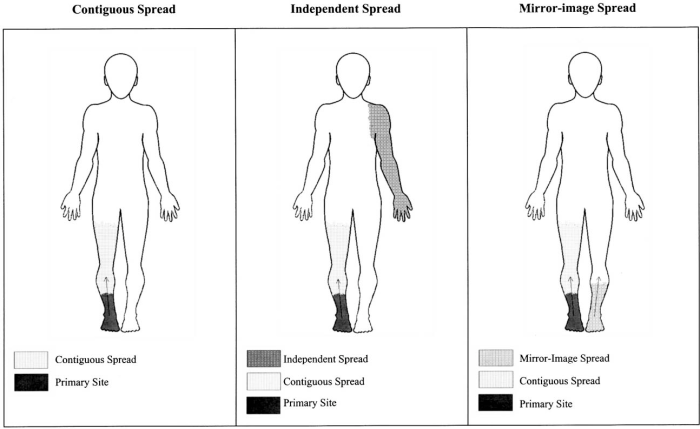
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints. It’s characterized by inflammation and pain, which can progressively damage the joint tissues, leading to long-term disability if left untreated. Understanding the nature of RA, from its initial symptoms to its potential progression, is crucial for effective management and improved quality of life.The key characteristics of RA include persistent inflammation, often symmetrical, targeting multiple joints.
This chronic inflammatory process can cause a wide range of symptoms, impacting daily activities and overall well-being. Early recognition and prompt medical intervention are vital in slowing disease progression and mitigating long-term complications.
Key Characteristics and Symptoms of RA
RA manifests with a range of symptoms that can vary in severity and duration. Common symptoms include joint pain, swelling, stiffness, and tenderness. These symptoms frequently affect multiple joints, often symmetrically (meaning both sides of the body are affected). Early symptoms may be subtle and easily overlooked, but they can escalate to significant joint damage over time.
Progression of Rheumatoid Arthritis
The progression of RA is typically characterized by periods of remission and flare-ups. Early stages often feature mild symptoms affecting a few joints, with occasional periods of relief. As the disease progresses, more joints become involved, and symptoms intensify, leading to increasing pain and stiffness. Established RA can cause significant joint deformity, functional limitations, and potentially affect other organs.
Common Misconceptions about RA
Some common misconceptions about RA include believing it’s solely a disease of the elderly, or that it only affects women. While RA can affect people of all ages, and women are more commonly affected, it’s not limited to any single demographic. Also, RA is not simply a “wear and tear” condition of the joints, but rather a complex autoimmune response.
The disease can affect many individuals and impact their lives.
Symptoms Table, Risk factors for rheumatoid arthritis
| Symptom | Description | Severity Scale | Typical Onset Age |
|---|---|---|---|
| Joint Pain | Persistent aching or throbbing sensation in the joints. | Mild (occasional discomfort) to Severe (unbearable pain). | Usually between 30 and 50 years, but can occur at any age. |
| Joint Swelling | Inflammation of the joint lining, causing visible or palpable enlargement. | Mild (slight puffiness) to Severe (significant swelling). | Usually between 30 and 50 years, but can occur at any age. |
| Joint Stiffness | Difficulty moving the affected joints, often worse in the morning. | Mild (slight limitation) to Severe (immobility). | Usually between 30 and 50 years, but can occur at any age. |
| Fatigue | Extreme tiredness and lack of energy. | Mild (occasional tiredness) to Severe (inability to perform daily tasks). | Usually between 30 and 50 years, but can occur at any age. |
Genetic Predisposition
Understanding rheumatoid arthritis (RA) requires acknowledging the significant role of genetics. While environmental factors undoubtedly play a part, a predisposition towards the disease often stems from inherited variations in certain genes. This genetic component significantly influences an individual’s risk of developing RA.The intricate dance between genetic makeup and environmental triggers shapes the development of RA. Individuals inheriting specific gene variations may be more susceptible to the disease, but environmental factors, such as infections or lifestyle choices, can ultimately determine whether these genes manifest into clinical RA.
This interplay highlights the complexity of the disease and underscores the importance of a multifaceted approach to understanding and managing it.
Specific Genes Associated with Increased RA Risk
Certain genes are strongly linked to an increased risk of developing rheumatoid arthritis. These genes are often involved in the body’s immune response, playing a crucial role in the autoimmune processes that characterize RA. A variety of genes, some more strongly associated than others, influence RA risk. Some examples include genes encoding proteins involved in the inflammatory response, such as those related to the major histocompatibility complex (MHC) region, and genes regulating immune cell function.
Understanding risk factors for rheumatoid arthritis is key to preventative measures. While genetics play a role, environmental factors can also influence susceptibility. Interestingly, some studies suggest a potential connection between certain lung conditions, like those affecting the pleura, and rheumatoid arthritis. For a deeper dive into the pleura and the various conditions that can affect the lungs, check out this informative article on pleura lungs definition conditions.
Ultimately, a holistic approach to understanding risk factors is crucial for managing this complex autoimmune disease.
Mechanisms of Gene Contribution to RA Development
The mechanisms by which these genes contribute to RA development are complex and not fully understood. However, several key pathways are implicated. For instance, genetic variations within the MHC region can influence the presentation of antigens to immune cells, leading to an aberrant immune response. Further, genetic variations in genes regulating immune cell function can lead to abnormal activation and proliferation of immune cells, resulting in chronic inflammation.
These genetic predispositions, combined with environmental triggers, can lead to the autoimmune cascade characteristic of RA. The interplay between these genetic factors and environmental triggers is a crucial area of ongoing research.
Comparison and Contrast of Genetic Risk Factors Across Different Populations
The genetic risk factors for RA vary across different populations. Studies have shown that certain gene variants are more prevalent in specific ethnic groups, which can contribute to variations in RA prevalence across different populations. For example, specific MHC alleles may be more frequent in certain populations, potentially explaining variations in the disease’s incidence.
Role of Family History in RA Susceptibility
A strong family history of rheumatoid arthritis significantly increases an individual’s risk of developing the disease. This observation highlights the heritability of RA and the crucial role of genetic predisposition. If a close relative has RA, the risk of an individual developing the disease is significantly higher than in the general population.
Prevalence of RA in Different Genetic Backgrounds
| Genetic Background | Prevalence of RA (Approximate) |
|---|---|
| European descent | 0.5-1.0% |
| African descent | 0.2-0.5% |
| Asian descent | 0.1-0.5% |
The table above provides a general overview of RA prevalence across different populations. It is important to note that these figures are approximate and can vary based on several factors, including the specific study design and population sampled. The wide range of prevalence emphasizes the complexity of RA’s manifestation and the influence of genetic factors in these variations. Additional factors such as lifestyle and environmental exposures further complicate the precise prediction of risk.
Environmental Factors
Beyond genetics, environmental factors play a significant role in the development of rheumatoid arthritis (RA). While the precise mechanisms are still being investigated, exposure to certain substances and conditions can trigger or exacerbate the autoimmune response that characterizes RA. Understanding these environmental influences is crucial for identifying potential risk factors and developing preventive strategies.
Impact of Environmental Exposures on RA Risk
Environmental exposures can interact with genetic predispositions to RA, potentially tipping the balance towards disease development. This interaction suggests that even individuals with a genetic predisposition might not develop RA if not exposed to certain environmental triggers. Conversely, individuals without a strong genetic link could still develop RA if exposed to a sufficiently potent combination of environmental factors.
This complex interplay highlights the importance of considering both genetic and environmental components in the overall risk assessment for RA.
Specific Environmental Factors Increasing RA Likelihood
Numerous environmental factors have been linked to an increased risk of RA. These include exposure to certain chemicals, infections, and even occupational hazards. While the precise mechanisms aren’t fully understood, the evidence strongly suggests a correlation.
While researching risk factors for rheumatoid arthritis, I stumbled upon the interesting correlation between stress and inflammation. It got me thinking about how mental health plays a role in overall well-being, and specifically, how medications for anxiety and depression might impact the body’s inflammatory response. This connection highlights the intricate interplay between physical and mental health, and emphasizes the importance of addressing all potential factors in managing rheumatoid arthritis.
Occupational Hazards Potentially Linked to RA
Certain occupational environments can expose individuals to substances that may trigger or exacerbate RA. Examples include exposure to silica dust, certain heavy metals, and even some pesticides. The specific mechanisms linking these exposures to RA development are often complex and involve interactions with the immune system. These occupational hazards highlight the importance of workplace safety measures and monitoring for potential RA risk factors in specific industries.
Table of Environmental Factors
| Factor | Mechanism of Impact | Evidence Level |
|---|---|---|
| Silica Dust | Inhalation of silica dust can lead to inflammation and immune system activation, potentially triggering or exacerbating RA in susceptible individuals. | Moderate |
| Heavy Metals (e.g., cadmium, lead) | Exposure to heavy metals may disrupt immune system regulation, increasing the likelihood of an autoimmune response, potentially contributing to RA development. | Moderate |
| Pesticides | Certain pesticides may contain chemicals that trigger an inflammatory response in the body, potentially influencing the development of RA. | Low to Moderate (more research needed) |
| Infections (e.g., Epstein-Barr virus) | Infections, particularly persistent or chronic infections, can trigger or modulate the immune system, potentially influencing the development of RA. | Moderate |
| Smoking | Smoking has been linked to a higher risk of developing RA and influencing disease progression. The exact mechanism is not fully understood, but it is thought to involve immune system dysregulation. | High |
Comparison of Environmental Triggers
The impact of different environmental triggers on RA risk varies. While some, like silica dust, might directly cause inflammation, others, such as infections, may act by altering the immune system’s response. Smoking, for example, seems to have a more generalized impact on immune function, increasing the risk of several autoimmune diseases, not just RA. The variability in mechanisms highlights the complex interplay between environmental factors, genetic predisposition, and the development of RA.
Immunological Factors
Rheumatoid arthritis (RA) is fundamentally an autoimmune disease, meaning the body’s immune system mistakenly attacks its own tissues. Understanding the intricacies of this immune response is crucial to comprehending the disease’s pathogenesis and developing effective treatments. This section delves into the immune cells, molecules, and pathways involved in RA, highlighting the dysregulation that drives the chronic inflammation characteristic of the disease.The immune system, normally tasked with defending the body against pathogens, malfunctions in RA, leading to the persistent attack on the synovial lining of joints.
This chronic inflammation eventually damages cartilage and bone, resulting in the debilitating joint destruction that defines RA.
The Role of the Immune System in RA Pathogenesis
The immune system’s primary function is to distinguish self from non-self. In RA, this critical distinction breaks down, resulting in an inappropriate and sustained immune response against the body’s own tissues. This dysregulation begins with the activation of specific immune cells and the production of autoantibodies, ultimately leading to chronic inflammation.
Immune Cells and Molecules Involved in the Autoimmune Response
The complex interplay of immune cells and molecules is essential in RA’s development. Key players include:
- T cells: A critical component of the adaptive immune system, T cells are activated by antigen-presenting cells (APCs) like macrophages and dendritic cells. Activated T cells, specifically Th1 and Th17 cells, release cytokines, proteins that orchestrate the inflammatory response. The abnormal activation and proliferation of these T cells contribute significantly to the pathogenesis of RA.
- B cells: B cells are responsible for producing antibodies. In RA, B cells are activated and produce autoantibodies, particularly rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPA). These autoantibodies target specific proteins within the joints, exacerbating inflammation.
- Macrophages and dendritic cells: These APCs play a crucial role in presenting antigens to T cells, initiating the immune response. Their activation and sustained presence in the synovium are hallmarks of RA’s inflammatory process. They contribute to the amplification and maintenance of the inflammatory cascade.
- Cytokines: Cytokines are signaling molecules that regulate the immune response. In RA, there’s an overproduction of pro-inflammatory cytokines like TNF-α, IL-1, and IL-6. These cytokines amplify the inflammatory cascade and contribute to the damage of joint tissues.
- Antigen-presenting cells (APCs): These cells, such as dendritic cells and macrophages, process and present antigens to T cells, initiating the immune response. In RA, APCs in the synovium are often activated and dysfunctional, leading to persistent immune activation.
Dysregulation of Immune Responses Contributing to RA
The immune response in RA is characterized by chronic and excessive inflammation, a deviation from the typical regulated immune response. This dysregulation stems from several factors, including:
- Genetic predisposition: Certain genetic variations predispose individuals to RA, impacting the function and activation of immune cells.
- Environmental triggers: Environmental factors, like infections or exposure to certain chemicals, may contribute to the development of RA by influencing the immune system.
- Immune cell dysfunction: The ability of immune cells to regulate themselves is compromised, leading to a persistent and uncontrolled inflammatory response.
- Autoantibody production: The production of autoantibodies, such as RF and ACPA, is excessive and targets healthy tissues, further driving the inflammatory process.
Immunological Pathways Targeted by Current Therapies
Current therapies for RA aim to modulate the dysregulated immune responses. These therapies target key inflammatory pathways:
- TNF-α inhibitors: These medications block the activity of TNF-α, a key cytokine involved in inflammation.
- IL-1 and IL-6 inhibitors: These drugs target other inflammatory cytokines crucial in RA pathogenesis.
- B-cell depletion therapies: These strategies aim to reduce the number of B cells and consequently the production of autoantibodies.
- T-cell modulation therapies: These treatments aim to regulate the activity of T cells, reducing their contribution to the inflammatory response.
Illustrative Immunological Cascade Leading to RA
(Note: This is a simplified representation of a complex process.)
| Step | Event |
|---|---|
| 1 | Environmental triggers or genetic predisposition activate the immune system. |
| 2 | Antigen-presenting cells (APCs) present antigens to T cells. |
| 3 | T cells, particularly Th1 and Th17 cells, become activated and proliferate. |
| 4 | Activated T cells release cytokines, amplifying inflammation. |
| 5 | Cytokines stimulate B cells to produce autoantibodies (e.g., RF, ACPA). |
| 6 | Autoantibodies bind to target tissues (e.g., joint tissues). |
| 7 | Inflammation becomes chronic, leading to joint damage. |
Lifestyle Factors
Beyond genetics and environmental exposures, lifestyle choices play a significant role in the development and progression of rheumatoid arthritis (RA). Understanding how diet, exercise, and stress impact RA risk is crucial for proactive management. Adopting healthy habits can potentially mitigate the risk and lessen the severity of symptoms, contributing to a better quality of life for those affected.
The Influence of Diet on RA Risk
A balanced diet rich in fruits, vegetables, and whole grains is associated with a reduced risk of developing various chronic inflammatory conditions, including RA. Anti-inflammatory foods, such as fatty fish rich in omega-3 fatty acids, can help modulate the immune system. Conversely, diets high in processed foods, saturated fats, and refined sugars may contribute to inflammation, potentially increasing RA risk.
The precise mechanisms linking diet to RA are still being investigated, but evidence suggests a strong correlation.
Understanding risk factors for rheumatoid arthritis is crucial for prevention and early intervention. While genetics play a role, environmental factors also contribute. Interestingly, similar to rheumatoid arthritis, certain factors can increase the likelihood of developing macular degeneration, like age and family history. Learn more about the factors that contribute to macular degeneration at macular degeneration causes risk factors.
Ultimately, pinpointing risk factors for rheumatoid arthritis is a complex puzzle, with ongoing research helping us piece together the picture.
The Impact of Exercise on RA Risk
Regular physical activity is crucial for overall health and well-being, and it can also positively influence RA risk. Exercise helps maintain a healthy weight, which is important because obesity is a recognized risk factor for several inflammatory conditions. Furthermore, exercise improves cardiovascular health and can potentially reduce systemic inflammation. Moderate-intensity exercise, such as brisk walking, swimming, or cycling, can be beneficial.
It’s essential to consult with a healthcare professional before starting any new exercise program, especially if RA symptoms are present. Exercise should be tailored to individual needs and capabilities.
The Role of Stress in RA Development
Chronic stress can negatively impact the immune system, potentially increasing susceptibility to autoimmune diseases like RA. Stress hormones can exacerbate inflammation and hinder the body’s natural ability to regulate the immune response. Stress management techniques, such as meditation, yoga, and deep breathing exercises, may help reduce stress levels and potentially mitigate the risk of RA or help manage symptoms.
Lifestyle Interventions for Managing RA Risk
Implementing specific lifestyle interventions can contribute to reducing RA risk and managing its symptoms. These include adopting a balanced diet rich in fruits, vegetables, and whole grains; engaging in regular physical activity; and practicing stress management techniques. Maintaining a healthy weight through a combination of balanced nutrition and regular exercise is also vital.
Recommended Lifestyle Changes for Reducing RA Risk
| Lifestyle Aspect | Recommended Changes |
|---|---|
| Diet | Prioritize whole, unprocessed foods, including fruits, vegetables, and whole grains. Limit processed foods, saturated fats, and refined sugars. Include foods rich in omega-3 fatty acids, like fatty fish. |
| Exercise | Engage in regular moderate-intensity exercise, such as brisk walking, swimming, or cycling. Consult with a healthcare professional before starting a new exercise program. |
| Stress Management | Practice stress-reducing techniques like meditation, yoga, deep breathing exercises, or spending time in nature. Prioritize sufficient sleep. |
| Weight Management | Maintain a healthy weight through a balanced diet and regular exercise. |
Other Potential Risk Factors: Risk Factors For Rheumatoid Arthritis
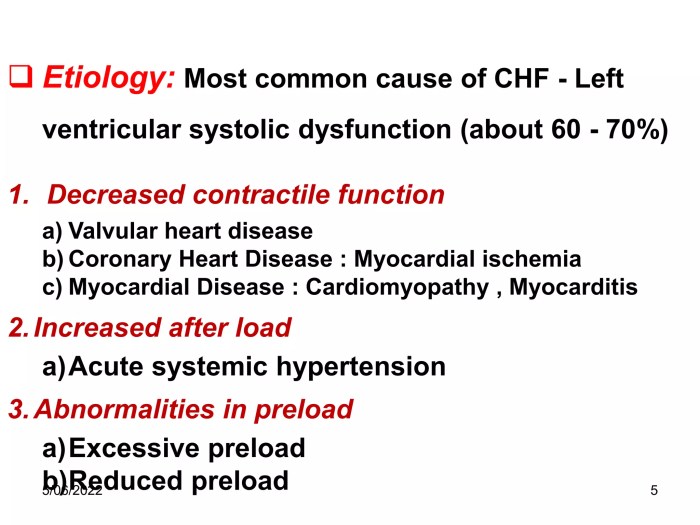
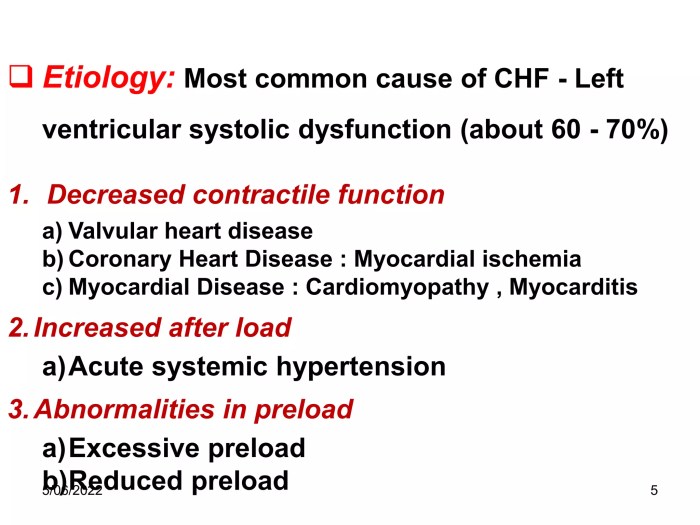
While genetic predisposition, environmental triggers, and immunological dysregulation play significant roles in rheumatoid arthritis (RA) development, other factors may also contribute. Infections, trauma, and hormonal fluctuations are potential risk factors that warrant further investigation. Understanding the possible mechanisms behind these associations and the current research landscape is crucial for developing a more comprehensive picture of RA etiology.The interplay between these potential factors and the underlying mechanisms involved in RA development remains complex.
While definitive causal links are often elusive, emerging research provides valuable insights into the intricate pathways that might connect these factors to the onset and progression of the disease. This exploration delves into the role of infections, trauma, and hormonal influences, exploring potential mechanisms and highlighting areas where further research is needed.
Infections
Certain infections have been linked to an increased risk of developing RA. These infections may trigger an inflammatory response that could contribute to the autoimmune process associated with RA. The exact mechanisms involved in this connection remain under investigation, but research suggests that some infections may mimic autoimmune responses, potentially leading to the activation of the immune system in a way that targets healthy tissues.
Trauma
While seemingly unrelated, trauma has been implicated as a possible risk factor for RA. Certain types of trauma, particularly those involving joints, may lead to tissue damage and inflammation. This inflammation could potentially trigger or exacerbate the autoimmune process in genetically predisposed individuals. Research into the relationship between joint trauma and RA is ongoing, exploring whether specific types of trauma or locations of injury might be associated with a higher risk.
Hormonal Influences
Hormonal fluctuations, particularly in women, have been suggested as potential risk factors for RA. The role of hormones, such as estrogen and progesterone, in immune regulation is well-established. Changes in hormone levels during menstruation, pregnancy, or menopause might influence the immune system’s activity and potentially contribute to the development or exacerbation of RA symptoms. Research is actively exploring the specific hormonal pathways involved and how they might interact with other risk factors.
Summary Table of Potential Risk Factors
| Potential Risk Factor | Possible Mechanisms | Supporting Evidence |
|---|---|---|
| Infections | Mimicking autoimmune responses, triggering inflammatory cascades, molecular mimicry | Studies showing associations between specific infections (e.g., Epstein-Barr virus) and RA development |
| Trauma | Joint damage and inflammation, triggering or exacerbating autoimmune responses in genetically susceptible individuals | Observational studies suggesting links between joint injuries and RA onset |
| Hormonal Influences | Alterations in immune regulation, impacting the balance between pro-inflammatory and anti-inflammatory processes, particularly in women | Studies showing increased RA risk in women during specific hormonal transitions |
Risk Factors and Disease Severity
Understanding rheumatoid arthritis (RA) severity is crucial for effective management. While various factors contribute to the development of RA, the interplay between these factors significantly impacts the disease’s progression and the degree of inflammation and joint damage. This section explores how different risk factors influence RA severity and the potential correlations between them.The severity of rheumatoid arthritis can range from mild, impacting daily life minimally, to severe, causing significant disability and affecting multiple organ systems.
The factors influencing this range are complex and interconnected, requiring a holistic approach to understanding and managing the disease.
Influence of Genetic Predisposition on Disease Severity
Genetic factors play a substantial role in determining an individual’s susceptibility to RA. Certain genes, particularly those involved in the immune system, increase the risk of developing the disease. Individuals with a stronger genetic predisposition might experience a more aggressive form of RA, characterized by faster progression, greater joint destruction, and an earlier onset. For example, a person inheriting a higher number of RA-associated genes may experience more severe symptoms like inflammation and pain at a younger age compared to someone with a weaker genetic predisposition.
Impact of Environmental Factors on Disease Progression
Environmental triggers, like infections, smoking, and exposure to certain chemicals, can exacerbate the effects of a genetic predisposition. Smoking, for instance, is a well-established environmental risk factor strongly associated with more aggressive disease courses. The combination of a genetic predisposition to RA and environmental exposures, like smoking, can lead to a more rapid progression and increased joint damage.
Individuals with a genetic predisposition might experience an earlier and more severe onset of RA symptoms when exposed to environmental triggers.
Role of Lifestyle Factors in Modifying Risk
Lifestyle choices can either exacerbate or mitigate the impact of genetic and environmental factors. A diet rich in processed foods and a lack of physical activity can contribute to systemic inflammation, potentially accelerating RA progression. Conversely, a balanced diet, regular exercise, and stress management techniques can potentially help to control inflammation and slow down the disease’s progression. For instance, a person with a genetic predisposition to RA and a sedentary lifestyle may experience a more severe and rapidly progressing form of the disease than someone with a similar genetic profile but who maintains an active lifestyle and a healthy diet.
Combinations of Risk Factors and Aggressive Disease
Certain combinations of risk factors can lead to a more aggressive form of RA. For example, a strong genetic predisposition coupled with heavy smoking and exposure to certain environmental pollutants can result in a rapidly progressive disease with significant joint destruction. The interplay between these factors creates a complex scenario, where one factor can amplify the effects of another.
This is not to say that every individual with a combination of risk factors will experience severe disease, but it does highlight the importance of understanding the potential impact of these factors in combination.
Table: Potential Impact of Risk Factor Combinations on Disease Severity
| Risk Factor Combination | Potential Impact on Disease Severity |
|---|---|
| Strong genetic predisposition + Heavy smoking + Environmental pollutants | High risk of aggressive disease, rapid progression, and significant joint damage |
| Moderate genetic predisposition + Sedentary lifestyle + Unhealthy diet | Increased risk of moderate disease progression, with potential for exacerbating inflammation |
| Strong genetic predisposition + Infections + Certain medications | Increased risk of flare-ups and potential for more aggressive disease in susceptible individuals |
Closure
In conclusion, risk factors for rheumatoid arthritis are a complex interplay of genetic, environmental, immunological, and lifestyle elements. While some factors are unchangeable, understanding these risks empowers individuals to take proactive steps towards reducing their susceptibility. Continued research into the intricate relationships between these factors is crucial for improving diagnostic tools, preventative measures, and ultimately, treatment outcomes for those affected by this chronic condition.