Clonus causes diagnosis and treatment – Clonus causes, diagnosis, and treatment is a complex medical issue. This comprehensive guide dives into the various facets of clonus, from its definition and underlying mechanisms to the different diagnostic tools and treatment approaches available. We’ll explore the neurological conditions frequently associated with clonus, discuss the impact of peripheral nerve damage, and delve into the specific symptoms that often accompany this condition.
We will also examine the prognosis and long-term management strategies.
Understanding clonus involves a deep dive into the neurological processes at play. From the initial diagnosis to the potential treatment options, we’ll navigate the complexities of this condition. This article is intended to provide a thorough overview of clonus, equipping readers with a better understanding of the challenges and approaches to managing this neurological condition.
Clonus Overview: Clonus Causes Diagnosis And Treatment
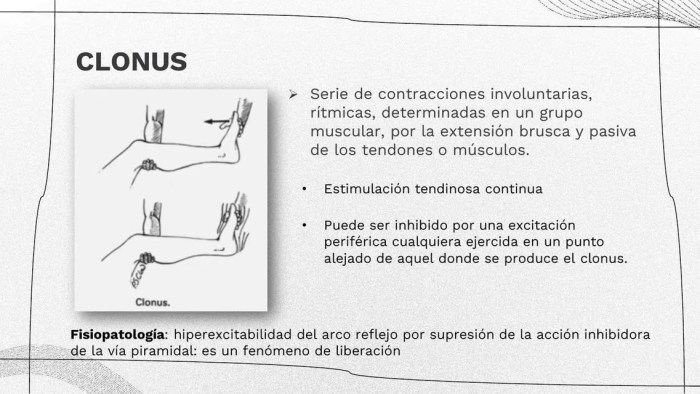
Clonus is a neurological condition characterized by rhythmic, involuntary muscle contractions. These contractions manifest as a series of rapid, repetitive movements, typically seen in the limbs or feet. Understanding clonus requires an examination of the underlying physiological mechanisms and the diverse types of clonus that can occur.Clonus arises from a disruption in the normal feedback loops regulating muscle tone.
Normally, the nervous system constantly adjusts muscle tension to maintain posture and stability. When this system is disrupted, an over-excitation of the stretch reflex pathway can occur. This leads to the cyclical contraction and relaxation of muscles, producing the characteristic clonic movements. The specific location and pattern of clonus can vary depending on the underlying cause.
Physiological Mechanisms of Clonus, Clonus causes diagnosis and treatment
The physiological basis of clonus involves an exaggerated stretch reflex. When a muscle is stretched, sensory receptors called muscle spindles detect the change in length. These receptors send signals to the spinal cord, triggering a motor response that contracts the muscle to resist the stretch. In clonus, this reflex loop is abnormally amplified. The initial muscle contraction further stretches the muscle, triggering a new signal, and the cycle repeats, resulting in the rhythmic contractions.
This over-excitement is often linked to lesions or damage in the central nervous system, particularly the spinal cord or brainstem.
Types of Clonus
While not formally categorized into distinct types, clonus can manifest differently based on the affected muscle groups and the underlying cause. Clinicians often describe clonus in terms of the affected body part (e.g., ankle clonus, jaw clonus). The severity and frequency of clonic contractions also vary considerably, impacting the clinical presentation.
Clonus Characteristics Table
| Type of Clonus | Possible Causes | Symptoms | Treatments |
|---|---|---|---|
| Ankle Clonus | Upper motor neuron lesions (e.g., stroke, multiple sclerosis, spinal cord injury), lower motor neuron lesions, and metabolic disorders | Rapid, rhythmic contractions of the calf muscles when the foot is dorsiflexed (pulled upward). Often accompanied by other neurological symptoms. | Treating the underlying cause is crucial. This may include medications to manage spasticity (e.g., baclofen, tizanidine), physical therapy to improve muscle control, and surgical interventions in severe cases. |
| Jaw Clonus | Similar to ankle clonus, upper motor neuron lesions are a common cause. Certain medications or conditions can also induce jaw clonus. | Rapid, involuntary rhythmic contractions of the jaw muscles. May be subtle or noticeable. | Addressing the underlying cause is paramount. Medications to control muscle spasms, therapies to improve jaw control, and in rare instances, surgical interventions may be employed. |
| Other Clonus Manifestations | Brain tumors, cerebral palsy, and various neurological conditions. Trauma to the head or spinal cord. Certain medications and toxins. | Variable depending on the affected area, ranging from mild muscle twitching to severe and debilitating spasms. Symptoms may also include tremors, weakness, or altered sensations. | Similar to other forms, treatment focuses on addressing the root cause. Medications to reduce muscle spasms, physical therapy to improve motor function, and supportive care are commonly used. Surgical intervention may be necessary in severe or intractable cases. |
Causes of Clonus
Clonus, characterized by rhythmic muscle contractions, is often a symptom rather than a disease itself. Understanding its underlying causes is crucial for effective diagnosis and treatment. This deeper look into the origins of clonus will highlight the neurological conditions and mechanisms that contribute to its development.A significant portion of clonus cases stem from disruptions within the central nervous system, specifically affecting the intricate pathways responsible for motor control.
The complex interplay of these pathways, including the corticospinal tract and various brainstem structures, can be disrupted by various neurological conditions. Peripheral nerve damage, spinal cord injuries, and specific disease processes can all contribute to the development of clonus. Understanding these pathways and their interactions is key to grasping how clonus arises.
Clonus, a condition involving involuntary muscle spasms, can stem from various neurological issues. Diagnosing clonus often involves a neurological exam, looking for specific rhythmic movements. Treatment varies greatly depending on the underlying cause, but sometimes, managing the symptoms of dizziness, which can accompany clonus, is a key part of the process. For instance, if you’re experiencing nasal polyps and dizziness, exploring resources like nasal polyps symptoms dizzy might offer insights.
Ultimately, a doctor’s assessment is crucial to determine the best course of action for treating clonus.
Neurological Conditions Associated with Clonus
Various neurological conditions are frequently linked to clonus. These conditions affect the brain and spinal cord, causing disruptions in the neural pathways responsible for motor control and reflexes. These disruptions can lead to involuntary muscle contractions, manifesting as clonus. Understanding these conditions helps in accurate diagnosis and targeted treatment strategies.
Role of Neurological Pathways in Clonus Development
The corticospinal tract, a vital pathway for voluntary movement, plays a critical role in the development of clonus. Damage or dysfunction in this tract can lead to abnormal reflexes and involuntary muscle contractions. Other neurological pathways, including the brainstem and spinal cord, also contribute to the generation and control of muscle reflexes. Disruptions in these pathways can similarly result in the characteristic rhythmic muscle contractions of clonus.
Impact of Peripheral Nerve Damage on Clonus
Peripheral nerve damage can sometimes contribute to clonus, though less frequently than central nervous system disorders. Peripheral neuropathy, a condition characterized by damage to peripheral nerves, can alter the delicate balance of excitatory and inhibitory signals within the nervous system. This imbalance can contribute to the development of abnormal reflexes, including clonus. For example, in certain cases of diabetic neuropathy, peripheral nerve damage can lead to clonus in the affected limbs.
Role of Spinal Cord Injuries in Clonus Development
Spinal cord injuries are a significant cause of clonus. Damage to the spinal cord disrupts the normal flow of signals between the brain and the body, leading to alterations in reflexes. The resulting loss of inhibitory control can contribute to the development of clonus, especially in cases of injuries affecting the upper motor neuron pathways. For example, a severe spinal cord injury at the cervical level can lead to the development of clonus in the arms and legs.
Examples of Conditions Causing Clonus
| Condition | Typical Presentation | Diagnostic Procedures | Notes |
|---|---|---|---|
| Multiple Sclerosis | Progressive neurological dysfunction, including muscle weakness, sensory disturbances, and vision problems. Clonus is often seen in the legs. | Neurological examination, MRI of the brain and spinal cord, evoked potential studies. | Clonus in MS is a sign of upper motor neuron involvement. |
| Stroke | Sudden onset of neurological deficits, often affecting one side of the body. Clonus may be present in the affected limb. | Neurological examination, CT or MRI of the brain, blood tests. | Clonus in stroke patients indicates involvement of the corticospinal tract. |
| Cerebral Palsy | Group of disorders affecting motor skills, often resulting in muscle weakness and spasticity. Clonus can be a feature in some types. | Neurological examination, developmental history, MRI of the brain. | Clonus in cerebral palsy varies depending on the type and severity. |
| Spinal Cord Injury | Trauma to the spinal cord, leading to varying degrees of motor and sensory deficits. Clonus may develop in the limbs below the level of injury. | Neurological examination, MRI or CT scan of the spinal cord, neurological assessments. | Spinal cord injury often results in severe clonus. |
Diagnosis of Clonus
Diagnosing clonus involves a meticulous approach combining clinical observations with specific neurological tests. A thorough understanding of the underlying causes and associated symptoms is crucial for accurate diagnosis and appropriate treatment strategies. Careful evaluation helps differentiate clonus from other neurological conditions with similar symptoms.
Common Clinical Tests for Clonus
Clinical tests play a vital role in identifying clonus. These tests focus on eliciting the characteristic rhythmic muscle contractions. A key aspect is the consistency of the results across different tests and their correlation with other clinical findings.
- Neurological Examination: A comprehensive neurological examination is essential. It assesses reflexes, muscle tone, coordination, sensation, and mental status. This assessment provides valuable information about the presence and characteristics of clonus, including the affected limbs and the degree of muscle involvement.
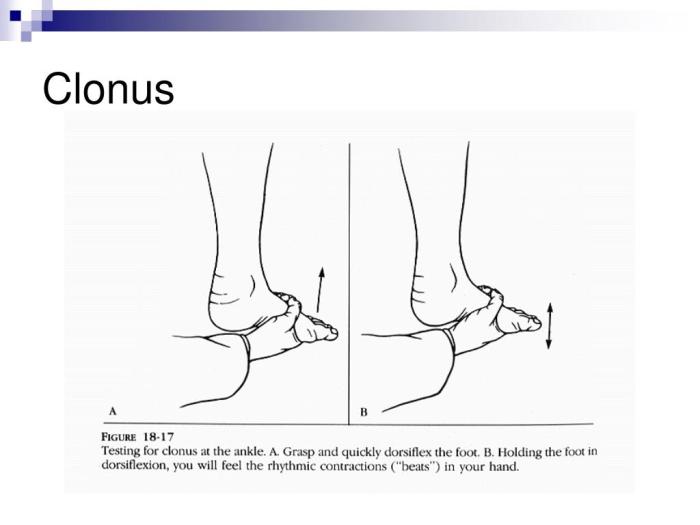
- Eliciting the Clonus Reflex: The clonus reflex is elicited by briskly dorsiflexing the foot. This action stretches the muscles in the lower leg, stimulating the stretch reflex. The examiner observes the rapid, rhythmic contractions. The examiner maintains the dorsiflexion and observes the frequency and amplitude of the oscillations. The frequency of the oscillations, measured in cycles per second, and the duration of the clonus are important diagnostic indicators.
Understanding clonus, a condition characterized by involuntary muscle contractions, involves exploring its causes, diagnosis, and treatment options. While various factors can contribute to clonus, a key area of investigation often involves exploring potential underlying neurological issues. For example, knowing about the properties of natural cleaning products like castile soap, as detailed in this article about castile soap what it is uses risks , might seem unrelated, but a holistic approach to health can be important.
Ultimately, accurate diagnosis and tailored treatment plans are crucial for managing clonus effectively.
- Muscle Strength Testing: Assessing muscle strength helps determine the presence of weakness or spasticity associated with clonus. This is crucial for differentiating between various neurological conditions and establishing a more precise diagnosis. The examiner observes the patient’s ability to resist passive movement against force.
Role of Neurological Examinations in Detecting Clonus
Neurological examinations provide a structured framework for evaluating the nervous system. These examinations assess various functions, including motor skills, sensory perception, reflexes, and coordination. The evaluation of reflexes is crucial in detecting clonus.
- Reflex Assessment: A detailed evaluation of deep tendon reflexes is essential. The examiner observes the response to percussion on specific tendons, such as the Achilles tendon. This assessment helps determine the presence and characteristics of clonus, such as the frequency and amplitude of oscillations. The degree of hyperreflexia, if present, provides additional diagnostic clues.
- Coordination Testing: Testing coordination helps assess the involvement of the cerebellum and other brain structures. Assessing gait and balance, and performing finger-to-nose or heel-to-shin tests helps determine the presence of neurological dysfunction.
Diagnostic Tools to Differentiate Clonus from Other Conditions
Accurate differentiation between clonus and other neurological conditions is crucial for appropriate treatment.
- Electrodiagnostic Studies: Electromyography (EMG) and nerve conduction studies help differentiate clonus from other neurological conditions characterized by muscle spasms or abnormal electrical activity. These studies can help identify the specific location and nature of the neurological abnormality.
- Imaging Studies: Magnetic resonance imaging (MRI) and computed tomography (CT) scans provide detailed anatomical images of the brain and spinal cord. These images help identify structural abnormalities, such as tumors, lesions, or vascular malformations, that may be associated with clonus. These studies can reveal underlying anatomical causes of the clonus.
- Blood Tests: Comprehensive blood tests help rule out metabolic or other systemic conditions that might mimic the symptoms of clonus. These tests aid in identifying any underlying medical conditions that may be contributing to the neurological symptoms.
Diagnostic Methods Summary Table
| Diagnostic Method | Accuracy | Potential Limitations | Clinical Significance |
|---|---|---|---|
| Neurological Examination | High | Subjectivity in interpretation, inconsistent findings | Initial screening tool, identifies potential clonus |
| EMG/NCS | High | Invasive procedure, expensive | Confirms presence of nerve/muscle dysfunction |
| Imaging (MRI/CT) | High | Cost, exposure to radiation (CT) | Identifies structural abnormalities |
| Blood Tests | Moderate | May not always reveal cause of clonus | Rules out systemic conditions |
Treatment of Clonus
Clonus, a sustained muscle spasm characterized by rhythmic contractions, can significantly impact a person’s quality of life. Effective treatment aims to manage the symptoms, address the underlying cause, and improve overall function. While a complete cure isn’t always possible, various therapeutic approaches can help reduce the severity and frequency of clonic episodes.Pharmacological interventions, physiotherapy, and in some cases, surgical procedures play a crucial role in the treatment strategy.
Careful consideration of the individual’s specific condition, including the underlying neurological disorder and overall health, is essential in determining the most appropriate course of action.
Pharmacological Interventions
Pharmacological agents are frequently employed to manage the involuntary muscle contractions associated with clonus. These medications work by targeting the neural pathways responsible for the abnormal muscle activity. Commonly used medications include benzodiazepines, such as diazepam, which can effectively reduce spasticity and clonus. Other options include baclofen, a muscle relaxant, and certain anti-epileptic drugs, which can help modulate abnormal neuronal activity.
The choice of medication depends on the severity of clonus, the presence of other neurological conditions, and potential side effects.
Role of Physiotherapy
Physiotherapy plays a vital role in the comprehensive management of clonus. Physiotherapists use various techniques to improve muscle strength, flexibility, and coordination. These strategies include stretching exercises, range-of-motion exercises, and strengthening programs tailored to the individual’s needs. Furthermore, physiotherapy helps to address the secondary complications that often arise from clonus, such as contractures and joint deformities. The goal is to maintain or improve functional abilities and reduce the impact of clonus on daily activities.
Surgical Interventions
Surgical interventions for clonus are typically reserved for cases where other treatments have failed to provide adequate relief. Procedures such as deep brain stimulation (DBS) target specific brain regions involved in motor control, aiming to reduce abnormal neural activity. However, the decision to pursue surgery should be made cautiously, weighing the potential benefits against the risks involved. Careful consideration should be given to the patient’s overall health, the severity of the clonus, and the possibility of alternative treatments.
Management of Underlying Conditions
Effective clonus management frequently involves addressing the underlying neurological disorder. For instance, if clonus is a symptom of multiple sclerosis, treatment strategies will focus on managing the symptoms of multiple sclerosis itself. Similarly, if clonus is a manifestation of cerebral palsy, interventions will encompass physical therapy, occupational therapy, and medication aimed at improving motor function. Comprehensive care that considers the root cause is essential for optimal outcomes.
Comparison of Treatment Approaches
Different treatment approaches for clonus offer varying degrees of efficacy and potential side effects. A balanced evaluation of these factors is crucial in selecting the most appropriate course of action. The table below provides a concise comparison of various treatment options.
| Treatment Option | Potential Benefits | Potential Risks | Suitable Conditions |
|---|---|---|---|
| Pharmacological Agents (e.g., Diazepam, Baclofen) | Reduction in spasticity and clonus; potential improvement in motor function | Sedation, dizziness, weakness, dependence | Various neurological disorders exhibiting spasticity and clonus |
| Physiotherapy | Improved muscle strength, flexibility, and coordination; reduced secondary complications | Potential for discomfort during exercises; limited impact on underlying neurological disorder | All individuals with clonus, regardless of underlying cause |
| Surgical Interventions (e.g., Deep Brain Stimulation) | Significant reduction in clonus in some cases; improvement in motor function | Surgical risks, infection, device malfunction, cognitive side effects | Severe clonus unresponsive to other treatments; specific neurological conditions |
Clonus and Associated Symptoms
Clonus, a series of involuntary muscle contractions, isn’t typically a standalone symptom. It often co-occurs with other neurological issues, significantly impacting a patient’s quality of life. Understanding these associated symptoms is crucial for proper diagnosis and management.Clonus frequently presents alongside a constellation of neurological symptoms, ranging from mild to severe. The specific symptoms and their severity depend on the underlying cause of the clonus and the affected area of the nervous system.
This interconnectedness underscores the importance of a comprehensive neurological evaluation.
Common Accompanying Symptoms
Clonus, often a sign of an underlying neurological condition, can manifest with a variety of associated symptoms. These symptoms can range from subtle motor issues to more significant impairments affecting daily life.
- Muscle weakness (paresis): Weakness in muscles surrounding the area affected by clonus can lead to difficulty with movement and coordination. For example, a patient with clonus in their lower legs might experience difficulty walking or climbing stairs.
- Spasticity: Increased muscle tone and stiffness, beyond the rhythmic contractions of clonus, can further limit movement and range of motion. This can be particularly noticeable in the affected limbs.
- Sensory disturbances: Patients may experience abnormal sensations such as numbness, tingling, or pain in the affected areas. These sensations can be related to nerve damage or dysfunction.
- Headaches: Certain neurological conditions associated with clonus can trigger headaches. The intensity and frequency of headaches can vary significantly.
- Pain: Muscle spasms and the associated pressure on nerves can cause pain. This pain can range from mild discomfort to severe, debilitating pain.
Relationship Between Clonus and Other Neurological Symptoms
The relationship between clonus and other neurological symptoms is complex and often intertwined. Clonus is frequently a manifestation of an underlying neurological disorder or injury. The presence of clonus, combined with other symptoms, can offer valuable diagnostic clues to the underlying pathology.
- Multiple Sclerosis (MS): In MS, clonus may be a sign of demyelination, affecting the nerve pathways responsible for muscle control. Other symptoms in MS can include visual disturbances, fatigue, and cognitive changes.
- Stroke: Clonus can occur after a stroke, particularly affecting the lower extremities. The presence of clonus can indicate the extent of the brain damage and the areas affected. Other stroke symptoms include hemiparesis (weakness on one side of the body), aphasia (speech difficulties), and vision problems.
- Brain tumors: A brain tumor pressing on the brain stem or other motor pathways can induce clonus. Symptoms beyond clonus might include changes in personality, seizures, or difficulty with balance.
Impact on Functional Abilities
Clonus significantly impacts a patient’s functional abilities, affecting various aspects of daily life. The severity of the impact is directly related to the severity of clonus and the presence of other neurological symptoms.
- Walking and mobility: Clonus in the legs can severely restrict a patient’s ability to walk, stand, or climb stairs. The involuntary movements can interfere with balance and coordination.
- Activities of daily living (ADLs): Clonus can hinder daily tasks such as dressing, eating, bathing, and personal hygiene. The spasticity associated with clonus can make these tasks difficult or impossible to perform independently.
- Social participation: Difficulty with mobility and performing daily tasks can affect a patient’s social participation. This can lead to isolation and decreased quality of life.
Impact on Daily Activities
The severity of clonus’ impact on daily activities is variable and depends on the individual and the associated symptoms. Clonus can create substantial challenges, affecting not only physical function but also emotional well-being.
| Associated Symptom | Severity (Example) | Potential Impact on Daily Functioning | Example |
|---|---|---|---|
| Muscle weakness | Mild to moderate | Difficulty with walking, dressing, or lifting objects | Inability to climb stairs independently |
| Spasticity | Moderate to severe | Impaired mobility, reduced range of motion, and painful muscle contractions | Significant limitations in performing ADLs like bathing or eating |
| Sensory disturbances | Mild to severe | Pain, numbness, tingling, or altered perception, impacting daily tasks | Difficulty with fine motor skills due to numbness |
| Pain | Severe | Significant discomfort, limiting mobility and affecting overall well-being | Inability to sleep due to severe muscle pain |
Illustrative Cases of Clonus
Understanding clonus requires exploring real-world examples. These cases illustrate the spectrum of presentation, diagnostic challenges, and treatment responses associated with this neurological condition. Analyzing patient histories and outcomes provides valuable insight into the complexities of managing clonus.
A Patient with Spastic Cerebral Palsy
This patient, a 10-year-old girl with spastic cerebral palsy, presented with intermittent clonus in her left lower limb. Her medical history revealed a perinatal brain injury. Symptoms included exaggerated muscle stretch reflexes, particularly in the affected limb. The diagnosis was confirmed through neurological examination, which demonstrated brisk and rhythmic contractions in the left gastrocnemius and soleus muscles.
Treatment focused on managing spasticity with botulinum toxin injections and physical therapy to improve muscle function and reduce the impact of clonus on daily activities.
Clonus of Unknown Origin
A 65-year-old man presented with clonus in both legs. His medical history was unremarkable, and initial investigations did not reveal any specific underlying neurological or systemic disease. The diagnostic process involved a comprehensive neurological evaluation, blood tests, and imaging studies (MRI of the brain and spinal cord). Electrodiagnostic studies (electromyography and nerve conduction studies) were also crucial to exclude other potential causes.
This case highlighted the importance of a thorough diagnostic workup when the underlying cause of clonus remains uncertain. Treatment involved symptomatic management of the clonus through medications and physical therapy to improve function. The ongoing monitoring and investigations were critical to identify a potential cause over time.
Resolution of Clonus Following Treatment of Multiple Sclerosis
A 45-year-old woman with a history of multiple sclerosis (MS) experienced progressively worsening clonus in her legs. Her MS diagnosis was confirmed through clinical examination, neurological history, and supportive laboratory testing, including MRI of the brain. The patient was treated with disease-modifying therapies (DMTs) for MS. Following a period of aggressive treatment, the clonus significantly improved and ultimately resolved.
This case underscores the crucial role of treating the underlying cause of clonus. The resolution of clonus after successful treatment of MS exemplifies the positive impact of addressing the root condition on neurological symptoms.
Progression and Diagnostic Challenges in Different Clonus Cases
The progression of clonus can vary significantly depending on the underlying cause. Some cases exhibit a gradual onset and worsening over time, while others may have a sudden, acute presentation. The diagnostic process can be challenging when the cause of clonus is unclear. Comprehensive neurological assessments, coupled with imaging and laboratory studies, are essential to identify the potential causes, such as stroke, spinal cord injury, and other neurological disorders.
Understanding clonus, a condition characterized by involuntary muscle contractions, involves examining its causes, diagnosis, and treatment. Often, underlying neurological issues are the culprit, but sometimes, conditions like atrioventricular reentrant tachycardia AVRT can manifest with similar symptoms. Precise diagnosis relies on neurological examinations and potentially imaging tests, while treatment targets the root cause and alleviates symptoms. Further research into the intricate relationship between neurological conditions and clonus is crucial for improved patient outcomes.
A thorough medical history, detailed physical examination, and specific diagnostic tests are critical for precise diagnosis. For example, in cases of suspected metabolic disorders, specialized blood tests are necessary. Treatment approaches vary based on the identified cause. For instance, treatment for MS differs significantly from treatment for a stroke.
Treatment Responses and Outcomes in Clonus Cases
Treatment responses to clonus are diverse and depend heavily on the underlying cause. Some patients may experience significant improvement with medication, physical therapy, or surgical interventions. Other patients may only experience partial or temporary relief. Long-term outcomes often depend on the severity of the underlying condition, the effectiveness of the chosen treatment, and the patient’s overall health status.
Regular monitoring is essential to track the response to treatment and adjust the approach as needed.
Clonus and Prognosis
Understanding the long-term outlook for individuals experiencing clonus is crucial for effective management and support. Clonus, characterized by involuntary muscle spasms, can significantly impact a person’s quality of life. Predicting the specific trajectory of clonus, however, is complex, as numerous factors contribute to the outcome. The severity of the underlying condition, the responsiveness to treatment, and the individual’s overall health are all critical elements to consider.The prognosis for clonus is not a simple yes or no answer; rather, it depends on several interwoven variables.
These include the underlying cause of clonus, the efficacy of treatment strategies, and the patient’s overall health and resilience. Careful monitoring and personalized interventions are essential for optimizing the patient’s long-term well-being.
Factors Influencing Clonus Prognosis
The effectiveness of clonus treatment and the eventual prognosis depend on a variety of intertwined factors. These factors include the underlying neurological condition, the patient’s age, and their overall health status.
- Underlying Neurological Condition: The cause of clonus significantly influences the prognosis. For instance, if clonus arises from a treatable condition like a stroke in its early stages, the prognosis may be more favorable than if it’s associated with a progressive neurological disorder. Early diagnosis and intervention are crucial in these cases.
- Age of Onset: The age at which clonus develops can impact the long-term outcome. Younger individuals may have a greater capacity for neurological recovery compared to older adults. This is because younger brains have greater neuroplasticity and the ability to adapt to damage.
- Overall Health Status: Pre-existing medical conditions, such as diabetes or cardiovascular disease, can affect the course of clonus and influence the prognosis. Patients with comorbidities may experience more complications or slower recovery.
- Treatment Response: The effectiveness of treatment strategies plays a pivotal role. A prompt and effective response to medication or other interventions positively influences the prognosis. This can lead to a decrease in clonus severity and improved quality of life.
Potential Outcomes of Clonus
The outcome of clonus treatment varies widely. Some individuals experience a complete or near-complete resolution of clonus symptoms, while others may experience a reduction in severity. The long-term management strategy needs to address the specific circumstances of each patient.
- Complete Resolution: In some cases, clonus can completely resolve, often linked to successful treatment of the underlying cause. This positive outcome hinges on factors like the early detection of the condition and the timely implementation of appropriate interventions.
- Partial Resolution: In many cases, clonus may be significantly reduced, but not completely eradicated. The severity and frequency of clonus episodes may diminish, allowing for a better quality of life.
- Persistent Clonus: In some situations, clonus may persist despite treatment. The impact on quality of life can be significant, necessitating ongoing support and management strategies.
Long-Term Management Strategies
The ongoing management of clonus necessitates a multidisciplinary approach. This includes medication adjustments, physical therapy, and lifestyle modifications. Monitoring the patient’s condition over time is crucial for adapting the treatment plan as needed.
| Factors Influencing Prognosis | Potential Outcomes | Long-Term Management Strategies | Illustrative Example |
|---|---|---|---|
| Underlying cause (e.g., stroke, multiple sclerosis) | Complete resolution (stroke in early stages), partial resolution (multiple sclerosis), or persistent clonus | Early diagnosis and treatment, rehabilitation, ongoing monitoring, symptom management | A patient with a stroke experiencing complete resolution of clonus following intensive rehabilitation |
| Patient’s age and overall health | Favorable outcome in younger patients with good health, potentially slower recovery in older or compromised individuals | Personalized treatment plan, management of comorbidities, tailored rehabilitation | An elderly patient with cardiovascular disease experiencing a slower recovery from clonus |
| Treatment response | Positive response to medication, improved quality of life, or persistent clonus despite treatment | Medication adjustments, physical therapy, lifestyle modifications, assistive devices | A patient with persistent clonus showing positive response to botulinum toxin injections |
Impact of Clonus on Quality of Life
Clonus can profoundly impact an individual’s quality of life. The involuntary muscle spasms can cause pain, discomfort, and limitations in movement and daily activities. This can lead to social isolation, emotional distress, and decreased participation in social and recreational activities.
Epilogue
In conclusion, clonus presents a multifaceted challenge requiring a nuanced approach to diagnosis and treatment. From the initial clinical presentation to the long-term management of the condition, understanding the interplay between the causes, diagnostic methods, and treatment options is crucial. This article has provided a comprehensive overview of clonus, highlighting the complexities and potential outcomes. Ultimately, a multidisciplinary approach, incorporating medical expertise and patient-centered care, is essential for achieving optimal outcomes.










