Complete guide to diuretics delves into the fascinating world of these medications, often used to manage various health conditions. From understanding their diverse types and mechanisms of action to recognizing potential side effects and interactions, this guide provides a comprehensive overview. We’ll explore how diuretics work, their various applications, and essential precautions to ensure safe and effective use.
Get ready to navigate the complexities of diuretic therapy with confidence!
This guide covers everything from the basics of diuretic function to advanced considerations for dosage, monitoring, and patient education. We’ll discuss the different types of diuretics, their unique actions on the kidneys, and the medical conditions in which they are commonly prescribed. We’ll also address the potential side effects and interactions, highlighting the importance of careful monitoring and patient education.
Introduction to Diuretics
Diuretics are medications that increase urine output. This process, known as diuresis, helps the body eliminate excess water and salts, often sodium. Their primary function is to lower blood volume and blood pressure, making them crucial in treating various medical conditions. Understanding their diverse mechanisms of action and potential side effects is essential for safe and effective use.Diuretics work by influencing the reabsorption of water and electrolytes in the kidneys.
Different types of diuretics target specific segments of the nephron, the functional unit of the kidney, resulting in varying degrees of diuresis and electrolyte loss. This targeted approach allows physicians to tailor diuretic therapy to individual patient needs and conditions.
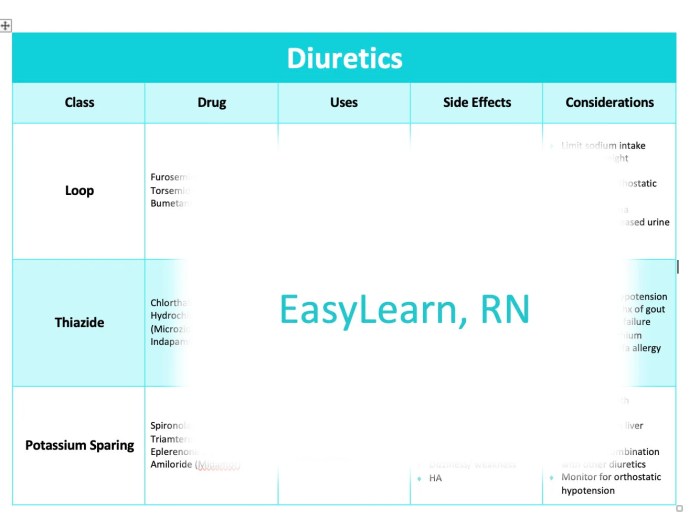
Types of Diuretics
Diuretics are broadly categorized based on their mechanism of action and their effect on electrolyte balance. Understanding these categories is vital for selecting the appropriate diuretic for a specific condition.
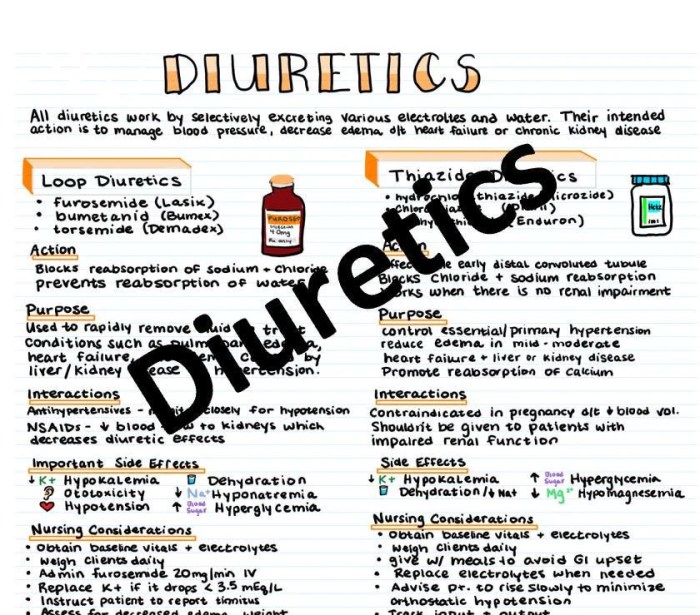
- Thiazide Diuretics: These diuretics act on the distal convoluted tubule in the kidney, inhibiting sodium reabsorption. This leads to an increase in sodium and water excretion, lowering blood pressure. Examples include hydrochlorothiazide and chlorthalidone. They are often a first-line treatment for hypertension and edema.
- Loop Diuretics: Loop diuretics, such as furosemide and bumetanide, exert their effect on the loop of Henle. They are highly effective in increasing urine output, which is beneficial in situations requiring rapid diuresis, such as acute pulmonary edema or heart failure. Their potent action makes them a strong choice for conditions requiring substantial fluid reduction.
- Potassium-Sparing Diuretics: These diuretics, including spironolactone and amiloride, work by blocking the reabsorption of sodium while retaining potassium. This is crucial in preventing the loss of potassium, a vital electrolyte. They are frequently used in conjunction with other diuretics to mitigate potassium depletion.
Medical Conditions Treated with Diuretics
Diuretics are prescribed for a range of medical conditions characterized by fluid retention or high blood pressure. Their use is carefully considered based on the individual patient’s needs and medical history.
- Hypertension: Diuretics are frequently used as a first-line treatment for high blood pressure, as they help reduce blood volume and subsequently lower blood pressure. This is achieved by increasing the excretion of sodium and water from the body.
- Heart Failure: In heart failure, the heart’s ability to pump blood is compromised, leading to fluid buildup in the lungs and other tissues. Diuretics help remove excess fluid, easing symptoms and improving overall cardiac function. Rapid diuresis is often needed in acute heart failure cases.
- Kidney Disease: In cases of kidney disease, the kidneys may not effectively filter waste products and fluids. Diuretics help manage fluid overload and improve the function of the kidneys in patients with compromised renal function. The type of diuretic selected depends on the specific stage and type of kidney disease.
- Liver Cirrhosis: Liver cirrhosis, a chronic liver condition, can lead to fluid retention in the abdomen (ascites). Diuretics can be used to reduce the accumulation of fluid, improving patient comfort and well-being.
Diuretic Comparison Table
The following table summarizes the key characteristics of different diuretic types.
| Diuretic Type | Mechanism of Action | Common Side Effects | Typical Uses |
|---|---|---|---|
| Thiazide | Inhibits sodium reabsorption in the distal convoluted tubule | Dehydration, hypokalemia, dizziness, nausea | Hypertension, edema |
| Loop | Inhibits sodium and chloride reabsorption in the loop of Henle | Dehydration, hypokalemia, hypomagnesemia, ototoxicity (rare), dizziness, nausea | Acute pulmonary edema, heart failure, hypercalcemia |
| Potassium-Sparing | Blocks sodium reabsorption while retaining potassium | Hyperkalemia, dizziness, nausea, gynecomastia (spironolactone) | Hypertension, edema, heart failure, preventing potassium loss with other diuretics |
Types of Diuretics
Diuretics, often called water pills, are medications that increase urine output. They play a crucial role in managing various health conditions, from high blood pressure to heart failure and kidney disease. Understanding the different types of diuretics and their mechanisms of action is vital for effective treatment and minimizing potential side effects.
Thiazide Diuretics
Thiazide diuretics are a common class of diuretics, primarily acting on the distal convoluted tubule of the kidneys. They inhibit the reabsorption of sodium and chloride ions, leading to increased excretion of water. This mechanism helps lower blood pressure by reducing fluid volume in the bloodstream.
- Mechanism of Action: Thiazides block the sodium-chloride cotransporter, reducing sodium reabsorption. This leads to an increased excretion of sodium and chloride, which is accompanied by water loss.
- Effectiveness: Thiazides are generally effective in lowering blood pressure, particularly in mild to moderate hypertension. They are often the first-line treatment for hypertension in many cases.
- Potential Side Effects: Potential side effects include hypokalemia (low potassium levels), hyponatremia (low sodium levels), hyperuricemia (increased uric acid), and increased blood glucose levels. Careful monitoring of electrolyte levels is essential when prescribing thiazides.
- Examples: Hydrochlorothiazide (HCTZ), chlorthalidone, and metolazone are common examples of thiazide diuretics.
Loop Diuretics
Loop diuretics are potent diuretics that act on the loop of Henle in the kidneys. Their powerful effect on sodium and chloride reabsorption results in significant fluid loss. They are frequently used in cases of severe edema and hypertension that do not respond to other diuretics.
- Mechanism of Action: Loop diuretics inhibit the sodium-potassium-chloride cotransporter, preventing the reabsorption of these electrolytes. This significantly increases the excretion of sodium, chloride, and water.
- Effectiveness: Loop diuretics are highly effective in inducing diuresis, making them crucial in situations requiring rapid fluid removal, such as acute pulmonary edema or severe heart failure.
- Potential Side Effects: Potential side effects include hypokalemia, hyponatremia, hypomagnesemia, ototoxicity (damage to the inner ear), and dehydration. Monitoring of electrolytes and careful dosage adjustments are necessary.
- Examples: Furosemide (Lasix), bumetanide, and torsemide are common examples of loop diuretics.
Potassium-Sparing Diuretics
Potassium-sparing diuretics are a class of diuretics that act on the distal tubule and collecting ducts of the kidneys. Their primary function is to reduce potassium loss, making them useful in situations where potassium depletion is a concern.
- Mechanism of Action: These diuretics either block the sodium channels or increase potassium reabsorption, thereby reducing potassium excretion.
- Effectiveness: Potassium-sparing diuretics are typically less potent than thiazides or loop diuretics in terms of diuresis. They are primarily used in combination with other diuretics to prevent potassium loss or in cases where potassium-sparing is the primary goal.
- Potential Side Effects: Potential side effects include hyperkalemia (high potassium levels), gynecomastia (breast enlargement in males), and metabolic acidosis. Close monitoring of potassium levels is crucial.
- Examples: Spironolactone, amiloride, and triamterene are examples of potassium-sparing diuretics.
Comparison Table
| Diuretic Type | Site of Action | Mechanism | Effectiveness | Side Effects | Applications |
|---|---|---|---|---|---|
| Thiazides | Distal convoluted tubule | Inhibit Na+/Cl- cotransporter | Moderate | Hypokalemia, hyperuricemia | Mild-moderate hypertension |
| Loop Diuretics | Loop of Henle | Inhibit Na+/K+/2Cl- cotransporter | High | Hypokalemia, ototoxicity | Severe edema, heart failure |
| Potassium-Sparing | Distal tubule and collecting ducts | Block Na+ channels or increase K+ reabsorption | Low | Hyperkalemia | Prevent K+ loss, combination therapy |
Uses and Indications
Diuretics, often called “water pills,” play a crucial role in managing a wide range of medical conditions by increasing urine output. Their effectiveness stems from their ability to enhance the kidney’s filtering process, removing excess fluid from the body. This action is beneficial in various situations where fluid retention poses a threat or complicates existing conditions. Understanding the specific uses and indications for diuretics is essential for responsible prescribing and patient management.Prescribing diuretics requires careful consideration of individual patient factors.
Their effectiveness and safety are significantly influenced by age, pre-existing conditions, and concomitant medications. For instance, certain diuretics may be more suitable for elderly patients due to their potential impact on electrolyte balance. Proper assessment of these factors ensures optimal therapeutic outcomes and minimizes potential adverse effects.
Medical Conditions Treated with Diuretics
Diuretics are prescribed for a variety of medical conditions where fluid retention is a significant factor. These conditions include hypertension, edema, heart failure, and certain kidney diseases. The rationale behind using diuretics in each case stems from their ability to reduce excess fluid volume, thereby relieving symptoms and preventing further complications.
Hypertension
Diuretics are frequently used as a first-line treatment for hypertension. Their effectiveness in lowering blood pressure arises from their ability to reduce blood volume. Reduced blood volume decreases the pressure exerted on blood vessel walls, thus lowering blood pressure. This mechanism is particularly important in patients with high blood volume contributing to hypertension. For example, patients with kidney disease or heart failure often have increased blood volume, making diuretics an essential component of their treatment regimen.
Edema
Edema, characterized by fluid buildup in tissues, is effectively managed with diuretics. This fluid retention can arise from various causes, including heart failure, kidney disease, liver cirrhosis, and certain medications. Diuretics help reduce the excess fluid, alleviating swelling and discomfort. A common example is patients with chronic venous insufficiency, who experience swelling in their lower extremities. Diuretics are often prescribed to reduce this swelling and improve comfort.
Heart Failure
Heart failure is a condition where the heart’s ability to pump blood is compromised. Fluid buildup in the lungs and other tissues is a common symptom. Diuretics are frequently used in heart failure management to reduce this fluid overload. Their role is critical in alleviating symptoms like shortness of breath and edema, thus improving the patient’s overall quality of life.
A clear example is the use of diuretics to reduce pulmonary congestion in patients experiencing acute decompensated heart failure.
Kidney Diseases
Certain kidney diseases can lead to fluid retention. Diuretics are often used to manage this fluid overload, preventing further damage to the kidneys and improving patient outcomes. For example, patients with chronic kidney disease often experience fluid retention as their kidneys lose their filtering capacity. Diuretics can help maintain adequate fluid balance in these patients.
Other Indications
Diuretics may be indicated in other conditions, such as:
- Premenstrual syndrome (PMS): Some women experience fluid retention during PMS. Diuretics may be used to reduce this symptom, though this use is not as common or straightforward as for other conditions.
- Certain types of seizures: In some cases, diuretics may be used to help manage fluid imbalances associated with seizures.
- Urinary tract disorders: Diuretics may be used to help manage certain urinary tract conditions.
It’s crucial to remember that diuretic use requires careful consideration of the individual patient’s medical history, including age, pre-existing conditions, and other medications. Monitoring electrolyte levels is vital to prevent potential complications. The decision to prescribe diuretics and the type of diuretic to use is a complex process that must be tailored to each patient’s unique needs.
Side Effects and Precautions
Diuretics, while crucial for managing various health conditions, come with potential side effects. Understanding these risks and taking precautions is vital for safe and effective treatment. Careful monitoring and proactive measures can significantly minimize these adverse reactions.
Potential Side Effects
Diuretics work by increasing urine output, which can lead to several side effects if not managed properly. The most common concern is dehydration, resulting from excessive fluid loss. Electrolyte imbalances, particularly low potassium (hypokalemia), are also significant risks. Other potential side effects include dizziness, headache, and nausea. It is essential to recognize these potential issues to promptly address them and prevent serious complications.
So, you’re diving deep into diuretics? That’s a great choice! Understanding how they work is key, especially if you’re navigating medication changes after a recent semaglutide introduction. For a thorough look at how your other medications might need adjusting after starting semaglutide, check out this handy guide: medication changes after semaglutide. This knowledge will be super helpful as you explore the complete guide to diuretics further, helping you understand potential interactions and side effects.
Monitoring for Adverse Reactions
Regular monitoring of patients taking diuretics is crucial. Blood tests to assess electrolyte levels (especially potassium) are essential. Vital signs, including blood pressure and heart rate, should be routinely checked. Clinicians must be attentive to any reported symptoms, such as muscle weakness, cramps, or unusual fatigue, which could indicate an electrolyte imbalance. Early detection and intervention are key to preventing severe complications.
Minimizing the Risk of Side Effects
Several strategies can help minimize the risk of side effects associated with diuretic use. Patient education plays a vital role, as understanding potential side effects empowers patients to report any unusual symptoms promptly. Adjusting the dosage and type of diuretic based on individual patient needs can also help. Maintaining a balanced diet rich in potassium-containing foods (e.g., bananas, spinach, potatoes) can help prevent hypokalemia.
Regular hydration is also important to counteract fluid loss.
Table of Potential Side Effects, Frequency, and Management
| Side Effect | Frequency | Management Strategy |
|---|---|---|
| Dehydration | Common, especially with high doses or inadequate fluid intake | Increase fluid intake. Monitor urine output. Adjust diuretic dose as needed. |
| Hypokalemia (low potassium) | Common, especially with loop and thiazide diuretics | Dietary potassium supplementation. Potassium-sparing diuretics. Monitor potassium levels regularly. |
| Electrolyte Imbalances (other than potassium) | Possible, depending on the type of diuretic | Monitor blood electrolytes. Adjust diuretic therapy. Address underlying causes if present. |
| Hypotension (low blood pressure) | Possible, especially in patients with pre-existing hypotension | Monitor blood pressure closely. Reduce diuretic dose. Administer fluid replacement as needed. |
| Muscle cramps | Possible, especially with hypokalemia | Correct the underlying electrolyte imbalance (e.g., potassium). Provide appropriate hydration. |
| Headache, dizziness, nausea | Occasional | Monitor for symptoms. Reduce diuretic dose. Provide symptomatic relief (e.g., antiemetics). |
Important Note: This table provides general information and is not a substitute for professional medical advice. Always consult with a healthcare professional for personalized guidance on diuretic use and management of potential side effects.
Interactions and Contraindications
Diuretics, while beneficial for managing various conditions, can interact with other medications and may not be suitable for everyone. Understanding these interactions and contraindications is crucial for safe and effective use. A thorough understanding of a patient’s medical history and current medications is essential before prescribing any diuretic.Careful consideration of potential drug interactions and contraindications is paramount to ensuring patient safety and therapeutic efficacy.
This section details these important aspects, emphasizing the significance of a comprehensive patient history prior to diuretic prescription.
Ever wondered about the complete guide to diuretics? They’re fascinating, but honestly, sometimes I get sidetracked thinking about other things that could be boosting my health, like home remedies for hair growth. Home remedies for hair growth are a whole other ballgame, but they do connect to the overall health picture. Regardless, understanding the complete guide to diuretics is crucial for anyone looking to manage their fluid balance effectively.
Potential Drug Interactions
Diuretics can interact with numerous medications, potentially altering their effectiveness or increasing the risk of adverse effects. These interactions often stem from the diuretics’ impact on electrolyte balance or kidney function.
- Certain medications, like lithium, can have their levels significantly altered by diuretics. This can lead to toxicity, highlighting the importance of monitoring lithium levels when diuretics are prescribed.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce the effectiveness of diuretics by impairing kidney function. This interaction may lead to decreased diuresis and potentially elevated blood pressure.
- Digoxin, a cardiac medication, can experience increased blood levels with diuretics, especially loop diuretics, potentially causing digoxin toxicity. Regular monitoring of digoxin levels is crucial in this scenario.
- Diuretics can also interact with certain antibiotics and antihypertensives, potentially leading to adverse effects. The precise nature of these interactions can vary depending on the specific diuretic and the interacting medication.
Contraindicated Conditions
Certain medical conditions necessitate avoiding diuretic use due to potential harm or lack of therapeutic benefit. A careful assessment of the patient’s overall health is crucial.
- Severe kidney disease or kidney failure can make diuretics ineffective or even harmful, potentially exacerbating existing issues. In such cases, alternative treatments are preferred.
- Dehydration is a significant contraindication, as diuretics can worsen the condition. Adequate hydration is vital for preventing dehydration and managing fluid balance.
- Electrolyte imbalances, particularly low potassium or sodium levels, can be exacerbated by diuretics. Careful monitoring of electrolyte levels is essential, and correction of imbalances is often required before diuretic initiation.
- Patients with severe heart conditions, such as uncontrolled heart failure or acute heart attack, should be carefully evaluated before diuretic use, as they may be unsuitable candidates due to potential adverse reactions. Careful consideration of potential risks and benefits is necessary.
Importance of Patient History
A complete and accurate patient history is crucial before prescribing any diuretic. This comprehensive overview includes a detailed account of current medications, past illnesses, allergies, and lifestyle factors. This approach ensures that the diuretic is appropriate for the individual’s specific needs and health status.
- Knowing the patient’s current medications is essential for identifying potential drug interactions and ensuring patient safety.
- Understanding past medical history helps determine if any underlying conditions might make diuretics inappropriate.
- Allergies to medications or other substances can influence the selection of a suitable diuretic.
- Lifestyle factors, such as diet and fluid intake, play a role in managing potential side effects and maximizing the benefits of diuretics.
Summary Table
| Diuretic Type | Potential Drug Interactions | Contraindicated Conditions |
|---|---|---|
| Thiazide Diuretics | NSAIDs, lithium, digoxin, some antibiotics | Severe kidney disease, dehydration, electrolyte imbalances |
| Loop Diuretics | NSAIDs, digoxin, aminoglycoside antibiotics | Severe kidney disease, dehydration, electrolyte imbalances, severe heart conditions |
| Potassium-Sparing Diuretics | ACE inhibitors, potassium supplements | Severe kidney disease, hyperkalemia, dehydration |
Dosage and Administration
Diuretics, crucial for managing fluid balance and various medical conditions, require precise dosage and administration to maximize effectiveness and minimize side effects. Understanding the appropriate dosages, routes of administration, and schedules is vital for safe and optimal patient care. This section delves into the specifics of administering diuretics, highlighting key considerations for different patient populations.
Dosage Ranges for Various Diuretics, Complete guide to diuretics
The dosage of a diuretic depends on several factors, including the specific type of diuretic, the patient’s medical history, kidney function, and the severity of the condition being treated. There is a wide range of dosages for each diuretic, and it is crucial to follow the prescribing physician’s instructions carefully. Dosage adjustments are frequently necessary to achieve the desired effect while minimizing adverse reactions.
Routes of Administration
Diuretics are typically administered orally, making them convenient for home use. However, intravenous (IV) administration is often employed in emergencies or when rapid diuresis is needed. The route of administration influences the onset and duration of the diuretic’s action.
Common Administration Schedules
Administration schedules vary depending on the diuretic and the patient’s needs. For example, some diuretics may be taken once daily, while others require multiple doses throughout the day. Regular monitoring of fluid intake and output is essential to adjust the dosage or schedule as needed.
Considerations for Specific Patient Populations
Elderly patients, individuals with impaired kidney function, and those with other underlying medical conditions may require lower initial doses of diuretics. Close monitoring is critical to detect any adverse reactions and adjust the dosage accordingly.
Table: Dosage Guidelines for Different Diuretics
| Diuretic | Dosage Range (mg/day) | Route of Administration | Frequency |
|---|---|---|---|
| Furosemide | 20-400 mg | Oral, IV | Once daily to twice daily |
| Hydrochlorothiazide | 12.5-50 mg | Oral | Once daily |
| Spironolactone | 25-100 mg | Oral | Once daily |
| Bumetanide | 0.5-10 mg | Oral, IV | Once daily to twice daily |
Monitoring and Evaluation
Diuretic therapy, while effective in managing fluid overload and various conditions, requires meticulous monitoring to ensure patient safety and optimal outcomes. Careful observation and evaluation are crucial for identifying potential side effects and adjusting the treatment plan as needed. This phase is not just about checking for symptoms; it’s about actively tracking the patient’s response to the medication and ensuring it’s working as intended.Close monitoring allows for early detection of adverse reactions, preventing complications, and fine-tuning the diuretic regimen to achieve the desired therapeutic effect.
This proactive approach enhances patient comfort and safety, making diuretic therapy a more effective and reliable treatment option.
So, you’re diving deep into a complete guide to diuretics? Knowing how these medications work is crucial, but understanding your rights to your medical records under HIPAA is equally important. This ensures you have full control over the information related to your health, including details about any diuretic prescriptions. This complete guide to diuretics will equip you with the knowledge you need, but remembering your rights is a crucial part of your health journey.
your rights to your medical records under hipaa Ultimately, staying informed about both your medication and your rights will help you make the best health decisions.
Electrolyte Balance Monitoring
Electrolyte imbalances are a significant concern with diuretic use. Diuretics increase the excretion of water, but also electrolytes like sodium, potassium, magnesium, and calcium. These imbalances can lead to a variety of serious complications, ranging from mild fatigue to life-threatening arrhythmias. Maintaining precise electrolyte levels is essential for optimal patient health.Regular blood tests are crucial to assess electrolyte levels.
These tests should be performed at specific intervals to track changes and make necessary adjustments to the diuretic regimen or supplement prescription. This proactive approach ensures the patient’s safety and well-being during diuretic therapy.
Assessing for Signs of Dehydration and Other Side Effects
Diligent observation for signs of dehydration is vital. Dehydration can manifest in various ways, including dry mouth, decreased urine output, dizziness, fatigue, and sunken eyes. Monitoring vital signs, including blood pressure, heart rate, and respiratory rate, provides additional crucial information.Careful evaluation of other potential side effects is equally important. Patients should be educated on the potential side effects, including nausea, vomiting, muscle cramps, and weakness.
Prompt reporting of these symptoms by the patient allows for early intervention and adjustment of the treatment plan. This proactive approach ensures patient comfort and minimizes potential complications.
Frequency of Monitoring and Follow-up Visits
The frequency of monitoring and follow-up visits depends on several factors, including the type of diuretic, the patient’s overall health, and the severity of the condition being treated. For example, patients starting on a new diuretic or those with pre-existing kidney or heart conditions may require more frequent monitoring and visits.Initial visits may be weekly or bi-weekly, followed by monthly or bi-monthly check-ups as the patient’s condition stabilizes.
Regular blood tests and assessments for signs of dehydration and other side effects are crucial throughout the treatment process. Adjustments to the medication regimen are made based on these evaluations, ensuring the treatment is effective and safe.
Tracking and Evaluating Patient Response to Diuretic Therapy
Tracking patient response involves careful documentation of the patient’s weight, intake and output of fluids, and blood pressure readings. These measurements help determine the effectiveness of the diuretic in reducing fluid retention and improving overall symptoms.Evaluating response includes analyzing the patient’s subjective reports of symptoms, such as edema reduction or improved breathing. Combining objective measurements with patient feedback provides a holistic view of the treatment’s efficacy.
This process allows for adjustments to the diuretic dosage or type if needed to optimize the therapy’s efficacy.
Patient Education
Understanding and managing diuretics effectively requires patient education. This empowers individuals to take an active role in their health, promoting adherence to treatment plans and minimizing potential side effects. Proper education ensures patients understand how diuretics work, when to take them, and what to watch for.
Crucial Information for Patients
Diuretics, often called water pills, help the body eliminate excess fluid. This can be beneficial for managing high blood pressure, edema (swelling), and certain heart conditions. Patients need to understand the specific diuretic prescribed, its purpose, and how it affects their body. They should be aware of potential side effects, such as dehydration, electrolyte imbalances, and dizziness, and when to contact their healthcare provider.
Knowledge of proper storage and disposal of medications is also important.
Questions Patients Should Ask
Patients should feel comfortable asking their healthcare providers questions about their diuretic regimen. This includes questions about the specific type of diuretic, the dosage, the frequency of administration, and the expected outcomes. Understanding potential side effects and how to manage them is crucial. Asking about dietary adjustments, and what to expect in terms of symptoms is also essential for patient understanding.
A detailed understanding of interactions with other medications is also important for patient safety.
Effective Communication Strategies
Clear and concise communication is key when educating patients about diuretics. Use simple language, avoiding medical jargon. Active listening is vital to ensure the patient understands the information. Visual aids, such as diagrams or charts, can be helpful in explaining complex concepts. Encourage questions and address concerns directly and honestly.
Emphasize the importance of adherence to the prescribed regimen and the potential consequences of non-compliance.
Patient Education Checklist
This checklist provides a framework for educating patients on diuretic use and management.
- Confirm Understanding of Diuretic Purpose: Ensure the patient understands the reason for taking the diuretic, whether it’s for high blood pressure, edema, or another condition. Explain the intended outcome and its impact on the patient’s overall health.
- Dosage and Administration Instructions: Clearly explain the correct dosage, timing, and method of administration (e.g., with food, on an empty stomach). Provide written instructions and encourage the patient to ask questions if anything is unclear.
- Potential Side Effects and Management: Discuss common side effects like dehydration, dizziness, and electrolyte imbalances. Emphasize the importance of reporting any unusual symptoms immediately to the healthcare provider. Provide strategies for managing side effects, such as increasing fluid intake or adjusting the diet.
- Dietary Considerations: Discuss any dietary restrictions or modifications that might be necessary, such as increasing potassium intake (for some diuretics) or limiting sodium intake. Explain why these dietary adjustments are needed.
- Monitoring and Follow-up Instructions: Artikel the importance of regular follow-up appointments with the healthcare provider to monitor the patient’s response to the medication and adjust the treatment plan as needed. Highlight specific monitoring procedures like blood pressure checks, and weight management.
- Importance of Adherence: Emphasize the importance of taking the medication as prescribed to achieve the desired therapeutic outcome. Discuss the potential consequences of not adhering to the treatment plan.
Ultimate Conclusion: Complete Guide To Diuretics
In conclusion, this complete guide to diuretics provides a robust understanding of these essential medications. We’ve covered their diverse applications, mechanisms of action, potential side effects, and critical considerations for safe use. Remember, this information is for educational purposes only, and it’s crucial to consult with a healthcare professional for any health concerns or before making any decisions related to your treatment.
By understanding the intricacies of diuretics, you can better collaborate with your doctor to achieve optimal health outcomes.










