Delirium what you should know – Delirium: What You Should Know is your comprehensive guide to understanding this often-overlooked medical condition. This in-depth look covers everything from the core characteristics and various types of delirium, to the causes, symptoms, and ultimately, effective management and prevention strategies. We’ll explore the crucial distinctions between delirium and other cognitive disorders, offering a clear and accessible understanding of this complex issue.
Delving into the different types, we’ll examine the spectrum of symptoms, from subtle signs to more overt expressions, and how these can fluctuate throughout the day. We’ll also delve into the critical factors in diagnosis and the various treatment approaches, both pharmacological and non-pharmacological. Finally, we’ll look at proactive prevention strategies and the long-term implications of delirium.
Defining Delirium
Delirium is an acutely disturbed state of mind that involves a sudden change in mental status. It’s characterized by a fluctuating course, meaning symptoms can wax and wane throughout the day or even within a short period. This fluctuating nature distinguishes it from other, more stable cognitive disorders. Understanding delirium is crucial for prompt diagnosis and effective intervention, as timely treatment can significantly improve outcomes.Delirium is fundamentally different from other cognitive disorders like dementia and depression.
While dementia is a progressive decline in cognitive abilities, and depression often presents with a persistent low mood, delirium’s hallmark is its sudden onset and fluctuating nature. Delirium is typically reversible, while dementia is not. Depression may present with some cognitive symptoms, but the overall pattern is different from the fluctuating nature of delirium.
Types of Delirium
Delirium manifests in various forms, each characterized by distinct behavioral patterns. Understanding these types aids in proper assessment and management. Hyperactive delirium is marked by heightened mental activity, such as agitation, restlessness, hallucinations, and disorientation. Hypoactive delirium, on the other hand, presents with reduced activity, slowed movements, and a quiet, withdrawn demeanor. Mixed delirium combines features of both hyperactive and hypoactive states, exhibiting a fluctuating pattern of activity levels.
Comparison of Delirium and Dementia
The following table highlights key differences between delirium and dementia, emphasizing the distinct characteristics of each condition:
| Characteristic | Delirium | Dementia |
|---|---|---|
| Symptoms | Sudden changes in mental status, such as confusion, disorientation, hallucinations, delusions, agitation, or lethargy. Symptoms fluctuate. | Progressive decline in cognitive functions, including memory, language, problem-solving, and judgment. Symptoms gradually worsen over time. |
| Onset | Rapid, often within hours or days. | Gradual, developing over months or years. |
| Duration | Temporary, usually resolving within a few days to a few weeks if treated appropriately. | Progressive and chronic, lasting for years. |
Causes and Risk Factors: Delirium What You Should Know
Delirium, a state of acute confusion, is often triggered by a complex interplay of factors. Understanding these causes and risk factors is crucial for early detection and intervention, ultimately improving patient outcomes. Identifying the underlying cause can significantly impact the treatment approach and prognosis.Common causes of delirium can be categorized in several ways, from infections to metabolic imbalances and even medication side effects.
Risk factors often include age, pre-existing medical conditions, and environmental stressors.
Common Causes of Delirium
Several factors can contribute to the development of delirium. These include infections, such as pneumonia or urinary tract infections, which can trigger inflammation and disrupt brain function. Dehydration, electrolyte imbalances, and even nutritional deficiencies can also disrupt normal brain processes, leading to delirium.
High-Risk Populations for Delirium
Certain populations are more susceptible to developing delirium. Older adults, especially those living in long-term care facilities, are at higher risk due to age-related physiological changes and pre-existing health conditions. Individuals with pre-existing cognitive impairments, such as dementia, are also more vulnerable. Furthermore, those with a history of stroke or traumatic brain injury are also at an increased risk.
Role of Pre-existing Medical Conditions
Pre-existing medical conditions can significantly increase the risk of delirium. Chronic illnesses, such as diabetes, heart failure, and chronic obstructive pulmonary disease (COPD), often involve complex interactions of medications, metabolic changes, and physiological stressors that can precipitate delirium. Even seemingly minor conditions, such as a urinary tract infection, can escalate into delirium in vulnerable individuals.
Medical Conditions Associated with Delirium
| Condition | Mechanism | Associated Symptoms |
|---|---|---|
| Urinary Tract Infection (UTI) | Infection triggers inflammation and releases toxins that can affect brain function. | Fever, chills, confusion, disorientation, urinary urgency. |
| Pneumonia | Inflammation of the lungs, often accompanied by fever and systemic response. | Fever, cough, shortness of breath, confusion, disorientation, rapid heart rate. |
| Dehydration | Insufficient fluid intake leads to electrolyte imbalance, disrupting brain function. | Dry mouth, thirst, decreased urine output, confusion, dizziness, weakness. |
| Electrolyte Imbalance (e.g., Sodium, Potassium) | Disruptions in sodium or potassium levels can affect nerve and muscle function, potentially causing delirium. | Nausea, vomiting, muscle cramps, confusion, seizures. |
| Medication Side Effects | Certain medications, particularly those affecting the central nervous system, can cause delirium as a side effect. | Confusion, hallucinations, agitation, tremors, disorientation. |
| Stroke | Reduced blood flow to the brain disrupts brain function, leading to delirium. | Sudden onset of confusion, weakness on one side of the body, difficulty speaking, vision changes. |
| Traumatic Brain Injury (TBI) | Physical damage to the brain can lead to inflammation and dysfunction. | Headache, nausea, vomiting, confusion, memory loss, seizures. |
Symptoms and Signs
Delirium is a fluctuating mental state characterized by a disturbance in attention and awareness. Recognizing the diverse range of symptoms is crucial for timely diagnosis and appropriate intervention. Understanding how these symptoms manifest and fluctuate can aid in differentiating delirium from other conditions.
Symptoms Across Cognitive Domains
Symptoms of delirium encompass various cognitive domains, impacting a person’s ability to think, process information, and react to their environment. This fluctuation in cognitive function can make it challenging to consistently assess the individual’s mental state. The fluctuating nature of delirium requires ongoing monitoring and observation.
- Attention and Awareness: Individuals experiencing delirium often have difficulty focusing, sustaining attention, and shifting their focus to different tasks. They may be easily distracted or exhibit a reduced awareness of their surroundings. This can range from mild difficulty concentrating to a complete disorientation in time and place. For instance, a patient might be unable to follow a conversation or respond appropriately to questions.
- Memory Impairment: Short-term memory problems are common. Patients might have difficulty remembering recent events or instructions. This could manifest as forgetting appointments, repeating questions, or losing track of conversations. Long-term memory, while sometimes affected, is usually less impacted compared to short-term memory.
- Thinking Disturbances: Patients may exhibit disorganized thinking, racing thoughts, or difficulty in expressing their thoughts clearly. They may experience illogical or nonsensical speech, making it challenging to understand their communication. This includes disorganized thought processes, hallucinations, and delusions.
Symptoms Across Behavioral Domains
Behavioral changes are also prominent features of delirium. These changes can vary significantly, impacting social interactions and daily activities.
- Psychomotor Activity: Patients may display either hyperactivity (restlessness, agitation, rapid movements) or hypoactivity (lethargy, reduced movement, slow responses). Hyperactivity often includes pacing, restlessness, and verbal outbursts, while hypoactivity manifests as reduced responsiveness and decreased engagement with the environment. This fluctuating activity level can be alarming for caregivers and medical professionals.
- Sleep-Wake Cycle Disturbances: Disruptions in the sleep-wake cycle are common, leading to insomnia or excessive daytime sleepiness. Nighttime confusion and agitation can be significant challenges for both the patient and their caregivers. This can be a prominent symptom, particularly in the elderly population.
- Changes in Perception: Hallucinations (seeing or hearing things that are not there) are a possible symptom. These can be visual, auditory, or tactile, and often contribute to the overall disorientation. Illusions (misinterpreting real stimuli) are also possible, leading to misinterpretations of the environment.
Symptoms Across Emotional Domains
Emotional lability and fluctuations are crucial aspects of delirium. These shifts can be sudden and unpredictable, impacting interactions and emotional well-being.
- Emotional Lability: Patients may experience rapid shifts in mood, from euphoria to anxiety, fear, or irritability. These mood swings can be challenging to manage and may be unpredictable. This includes abrupt changes in emotional expression, ranging from inappropriate laughter to extreme fear or anger.
- Anxiety and Fear: Anxiety and fear are common emotional responses in delirium. These feelings can be triggered by perceived threats or changes in the environment. This can lead to increased agitation and distress. The fear and anxiety can be intense and may not always be clearly related to external factors.
- Depression: In some cases, delirium can be accompanied by depressive symptoms. This can manifest as sadness, hopelessness, and loss of interest in activities. These symptoms can be particularly challenging to distinguish from other conditions.
Fluctuations in Symptoms
Delirium symptoms often fluctuate throughout the day. This means that a patient’s cognitive, behavioral, and emotional states can change significantly over a short period.
- Daytime vs. Nighttime: Symptoms are often more pronounced during the night or in periods of reduced stimulation. This fluctuation can be significant and may not always be consistent.
- Impact of Environmental Changes: The environment can significantly influence the intensity of delirium symptoms. A sudden change in surroundings, noise, or the presence of unfamiliar people can trigger or exacerbate symptoms. This emphasizes the need for a calm and supportive environment.
Variability in Delirium Types, Delirium what you should know
The specific presentation of delirium symptoms can vary depending on the underlying cause and contributing factors.
- Hyperactive Delirium: This type is characterized by restlessness, agitation, and increased psychomotor activity. The patient may be more easily startled or confused.
- Hypoactive Delirium: This type involves reduced psychomotor activity, lethargy, and decreased responsiveness. The patient may appear withdrawn or unresponsive.
Subtle Signs of Delirium
Certain signs of delirium can be subtle and easily overlooked.
- Changes in Speech and Communication: Difficulty understanding or expressing oneself, or using unusual or nonsensical words, can be early indicators of delirium.
- Changes in Daily Activities: Sudden difficulty with tasks that were previously routine, such as dressing or eating, could be early signs.
Symptom Categorization Table
| Domain | Symptoms |
|---|---|
| Cognitive | Attention deficits, memory problems, disorganized thinking, disorientation |
| Behavioral | Hyperactivity, hypoactivity, psychomotor agitation, sleep-wake cycle disturbances, changes in perception |
| Emotional | Emotional lability, anxiety, fear, depression |
Diagnosis and Assessment
Pinpointing delirium isn’t always straightforward. It requires a keen eye for subtle changes in a patient’s mental state, coupled with a thorough understanding of their medical history and current condition. Accurate diagnosis is crucial, as the appropriate treatment depends entirely on the underlying cause. Early recognition and intervention can significantly improve outcomes.A comprehensive diagnostic approach involves a multi-faceted evaluation, moving beyond simple observation to incorporate standardized assessment tools, physical examination findings, and a careful review of the patient’s medical history.
The goal is to distinguish delirium from other conditions that may present with similar symptoms, ensuring the right treatment plan is implemented.
Knowing the signs of delirium is crucial; it’s a serious condition that requires immediate medical attention. While exploring different treatments, understanding the nuances of medications like Wellbutrin and Zoloft, especially their similarities and differences, wellbutrin vs zoloft similarities and differences , can be helpful in the bigger picture of your overall health. Ultimately, staying informed about delirium and its potential impact on your well-being is key.
Diagnostic Criteria for Delirium
The diagnosis of delirium relies on the presence of specific criteria. These include a disturbance in attention and awareness, the development of these symptoms over a short period, and evidence of fluctuating course throughout the day. Crucially, the symptoms must be directly attributable to a medical condition, substance intoxication or withdrawal, or exposure to medications.
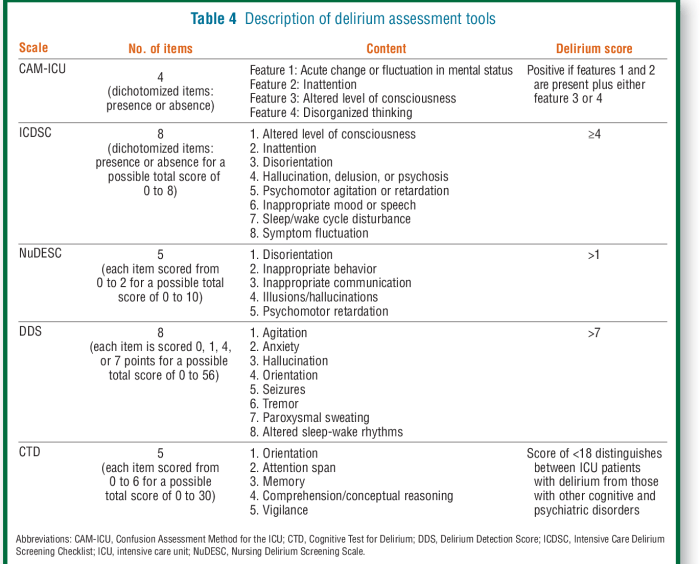
Methods for Assessing Cognitive Function
Several standardized cognitive assessment tools can help evaluate the cognitive function of individuals suspected of having delirium. These tools are designed to measure various cognitive domains, including attention, orientation, memory, language, and executive function. Examples include the Confusion Assessment Method (CAM), the Mini-Mental State Examination (MMSE), and the Montreal Cognitive Assessment (MoCA). Each tool assesses different aspects of cognitive function, providing a more comprehensive picture of the patient’s mental status.
Role of Medical History and Physical Examination
A thorough medical history and physical examination are integral to the diagnostic process. The history should explore potential contributing factors, such as recent infections, medications, surgery, or other illnesses. The physical examination should look for signs of underlying medical conditions that might be causing or exacerbating the delirium. This could include fever, dehydration, or evidence of infections.
Distinguishing Delirium from Other Conditions
It’s vital to distinguish delirium from other conditions that may present with similar symptoms, such as dementia, depression, or psychosis. Dementia, for instance, typically involves a gradual decline in cognitive function, whereas delirium presents with a more acute onset and fluctuating symptoms. Depression often manifests with sadness and loss of interest, contrasting with the fluctuating attention and awareness characteristic of delirium.
Understanding delirium can be tricky, but knowing the basics is key. It’s a temporary state of confusion and disorientation, and while it can be scary, it’s important to remember that treatment options exist. Often, massage therapy helps relieve pain associated with various conditions, including some that might contribute to delirium. For more information on how massage therapy can ease discomfort, check out this helpful resource: massage therapy helps relieve pain.
Ultimately, if you suspect someone is experiencing delirium, seeking professional medical help is crucial.
Careful consideration of the patient’s clinical picture, including the timeline of symptom development and fluctuations in their mental state, is critical for accurate diagnosis.
Steps in Diagnosing Delirium
| Assessment Tools | Observations | Expected Findings |
|---|---|---|
| Confusion Assessment Method (CAM) | Attention (ability to maintain focus and respond to questions) | Reduced attention span, difficulty focusing, easily distracted |
| Mini-Mental State Examination (MMSE) | Orientation (awareness of time, place, and person) | Disorientation to time, place, or person |
| Montreal Cognitive Assessment (MoCA) | Memory (short-term and long-term recall) | Impaired short-term and/or long-term memory |
| Medical History | Recent illnesses, medications, surgeries | Presence of underlying conditions potentially contributing to delirium |
| Physical Examination | Vital signs (temperature, heart rate, blood pressure), hydration status | Signs of infection, dehydration, or other medical issues |
Management and Treatment
Managing delirium effectively hinges on swift recognition and a multi-faceted approach. Prompt intervention is crucial to minimize the severity of symptoms and prevent long-term complications. A combination of non-pharmacological strategies and, when necessary, pharmacological treatments are often employed to address the underlying causes and alleviate the symptoms.
Importance of Early Intervention
Early recognition and intervention are paramount in delirium management. Delaying treatment can lead to prolonged confusion, increased risk of falls, complications from immobility, and difficulties in rehabilitation. Early action can significantly improve patient outcomes by reducing the duration of delirium and its associated cognitive impairment. For example, a timely intervention with appropriate hydration and pain management can prevent a patient from experiencing escalating confusion and agitation.
Understanding delirium is crucial for anyone concerned about their health. It’s a serious condition, and knowing the symptoms and when to seek help is important. Before you buy Allegra, for example, it’s essential to understand that certain medications can potentially worsen delirium symptoms in some individuals. Consulting your doctor about potential interactions is always a good idea.
Ultimately, staying informed about delirium and its possible links to other health concerns is key to good overall well-being. before you buy allegra
Non-Pharmacological Interventions
Non-pharmacological interventions are often the first line of treatment for delirium. These strategies aim to create a safe and supportive environment that reduces stress and disorientation for the patient.
- Creating a calming environment: This involves minimizing environmental stressors such as loud noises, bright lights, and excessive stimulation. Maintaining a consistent routine with predictable mealtimes and activities can also be helpful. A quiet, well-lit room with familiar objects can be reassuring for a patient experiencing delirium.
- Promoting sensory stimulation and engagement: Appropriate sensory stimulation can be beneficial for patients experiencing delirium. This could include calming music, gentle touch, or familiar objects. Encouraging participation in activities that are cognitively stimulating, but not overwhelming, can help improve focus and orientation. For example, showing pictures of loved ones or engaging in gentle conversation can be effective.
- Maintaining hydration and nutrition: Dehydration and malnutrition can exacerbate delirium symptoms. Ensuring adequate fluid intake and a balanced diet is essential for patient well-being. Regular monitoring of hydration status and appropriate dietary adjustments can contribute to a positive outcome.
- Pain management: Uncontrolled pain can worsen delirium symptoms. Thorough pain assessment and effective pain management are crucial in delirium care. Using non-pharmacological methods like heat or cold therapy alongside pain medication can be beneficial.
- Addressing sleep disturbances: Adequate sleep is vital for cognitive function. Ensuring the patient has a quiet, comfortable sleep environment and promoting sleep hygiene can reduce the severity of delirium symptoms.
Pharmacological Treatments
Pharmacological interventions for delirium are typically reserved for cases where non-pharmacological methods are insufficient or when the patient experiences severe agitation or hallucinations. The choice of medication depends on the individual patient’s condition and the underlying cause of the delirium.
- Antipsychotics: Antipsychotic medications, such as haloperidol or quetiapine, can be used to manage agitation and hallucinations. However, their use should be carefully considered due to potential side effects. Antipsychotics can effectively reduce agitation, but may cause extrapyramidal side effects like tremors or stiffness.
- Benzodiazepines: In certain cases, benzodiazepines might be considered for patients with delirium that has a component of anxiety or restlessness. However, their use needs to be cautious due to their potential for respiratory depression, particularly in elderly individuals or those with pre-existing respiratory conditions. Benzodiazepines may be helpful in reducing agitation but may also worsen confusion.
Comparison of Treatment Approaches
Non-pharmacological interventions offer a less invasive approach to delirium management, focusing on supportive care and environmental adjustments. They are generally preferred as a first-line approach, as they avoid the potential risks associated with pharmacological interventions. However, in severe cases, pharmacological treatments can be necessary to manage agitation and hallucinations effectively.
| Treatment Category | Intervention | Potential Benefits | Potential Risks |
|---|---|---|---|
| Pharmacological | Antipsychotics (e.g., haloperidol) | Reduces agitation, hallucinations | Extrapyramidal side effects, potential for worsening confusion |
| Pharmacological | Benzodiazepines (e.g., lorazepam) | Reduces anxiety, restlessness | Respiratory depression, cognitive impairment |
| Non-Pharmacological | Creating a calming environment | Reduces stress, disorientation | Requires careful monitoring and environmental adaptation |
| Non-Pharmacological | Maintaining hydration and nutrition | Supports overall well-being | Requires careful monitoring and intervention |
Prevention
Delirium, a state of acute confusion, is often preventable. Proactive measures, focusing on risk reduction and optimized care, play a crucial role in preventing its onset. Early identification of risk factors and timely interventions are essential to minimize the negative impact of delirium on patients.Effective prevention strategies require a multifaceted approach encompassing environmental modifications, nutritional support, and meticulous medical management.
By understanding the interplay of these factors, healthcare providers can create a supportive environment that mitigates the risk of delirium.
Optimizing Patient Care
Preventing delirium hinges on recognizing high-risk patients and implementing proactive measures. This includes careful monitoring of patients’ vital signs, cognitive status, and overall well-being. Early detection of potential triggers, such as infection or dehydration, is paramount. Implementing a multidisciplinary approach involving nurses, physicians, and other healthcare professionals ensures a coordinated response to patient needs. Close collaboration fosters a consistent and comprehensive plan of care, reducing the likelihood of delirium development.
Environmental Factors
The environment significantly influences a patient’s vulnerability to delirium. A calm and familiar environment is crucial for reducing stress and anxiety. Minimizing sensory overload, such as excessive noise or brightly lit rooms, is critical. Clear signage, familiar objects, and the presence of loved ones can provide a sense of comfort and reassurance. These measures contribute to a supportive environment that reduces the risk of confusion and disorientation.
Nutritional Support
Adequate hydration and nutrition are essential for preventing delirium. Maintaining proper hydration prevents dehydration, a significant risk factor for delirium. Patients should receive adequate caloric intake to maintain their energy levels and cognitive function. Malnutrition can significantly increase susceptibility to delirium. Providing nutritious meals and monitoring fluid intake are essential components of preventative care.
For example, ensuring patients receive easily digestible foods and clear liquids in appropriate quantities can significantly impact the risk.
Medical Interventions
Proactive medical interventions are key to delirium prevention. Identifying and addressing underlying medical conditions can significantly reduce the risk of delirium. For instance, treating infections swiftly and aggressively can prevent their progression into delirium. Regular medication reviews and adjustments to dosages can also mitigate the risk. Managing pain effectively is crucial, as pain can be a significant trigger for delirium.
Effective pain management reduces stress and discomfort, decreasing the likelihood of confusion.
Preventative Measures
- Environmental: Maintaining a quiet, well-lit, and familiar environment. Minimizing sensory overload by reducing noise and bright lights. Ensuring easy access to familiar items and support persons.
- Nutritional: Providing adequate hydration and caloric intake. Encouraging nutritious meals and clear liquids in appropriate quantities. Early identification and treatment of malnutrition.
- Medical: Addressing underlying medical conditions, such as infections, dehydration, and pain. Regular medication reviews and adjustments to dosages. Prompt treatment of infections and other medical issues.
Prognosis and Complications
Delirium, while often a temporary state, can have significant consequences. Understanding the potential outcomes and long-term complications is crucial for effective management and patient care. The impact on a person’s functional independence and the increased risk of mortality associated with delirium underscore the importance of prompt diagnosis and treatment. This section will explore the possible trajectories of delirium and the lasting effects it can have.
Potential Outcomes of Delirium
Delirium’s course varies widely. Some individuals experience a rapid resolution of symptoms within a few days, while others may experience a more prolonged period of confusion and disorientation. Factors such as the underlying cause, severity of the illness, and the patient’s overall health status all play a role in determining the length and intensity of the delirium episode.
In some cases, delirium may transition into a more persistent cognitive impairment, such as dementia. Careful monitoring and ongoing assessment are crucial to determine the specific course and potential long-term effects of delirium in each individual.
Long-Term Complications
Delirium’s impact extends beyond the acute phase. Long-term complications can significantly affect a person’s quality of life. One notable consequence is an increased risk of developing chronic cognitive impairment, including mild cognitive impairment (MCI) or dementia. Furthermore, delirium can exacerbate existing mental health conditions or contribute to the development of new ones. For example, an individual experiencing delirium due to a severe infection may experience lingering anxiety or depression following recovery from the acute illness.
The effects of delirium can also manifest as difficulty with daily activities and reduced functional independence.
Impact on Functional Independence
Delirium can significantly impair a person’s ability to perform daily tasks. This includes difficulties with activities of daily living (ADLs), such as bathing, dressing, and eating. Furthermore, delirium can disrupt cognitive functions, such as memory, attention, and problem-solving, hindering a person’s ability to manage finances, participate in social activities, and maintain personal relationships. A patient experiencing delirium may also experience difficulties with mobility and coordination, potentially requiring assistance with ambulation or other physical activities.
Link Between Delirium and Increased Mortality Risk
Studies have demonstrated a strong correlation between delirium and increased mortality risk. Delirium, especially in older adults, can be a marker of serious underlying health issues and a predictor of future complications. This increased risk is likely multifactorial, involving the interplay of the underlying medical conditions, the stress response triggered by delirium, and the potential for complications arising from prolonged illness.
For example, a patient experiencing delirium secondary to a stroke may have a higher risk of complications like aspiration pneumonia or further strokes, leading to a poorer prognosis.
Summary of Potential Complications
| Category | Potential Complications |
|---|---|
| Short-Term Effects | Confusion and disorientation |
| Hallucinations and delusions | |
| Agitation and restlessness | |
| Difficulty with communication and interaction | |
| Long-Term Effects | Increased risk of chronic cognitive impairment (e.g., dementia) |
| Exacerbation of pre-existing mental health conditions | |
| Reduced functional independence | |
| Increased mortality risk |
Summary
In conclusion, delirium is a significant health concern requiring prompt attention. By understanding its multifaceted nature, from definition and causes to symptoms, diagnosis, and management, we equip ourselves with the knowledge to support those affected. Prevention and early intervention are crucial for minimizing the potential impact of delirium, ultimately improving the quality of life for individuals and their loved ones.
Armed with this knowledge, you’ll be better prepared to navigate this complex medical condition.










