Fecal oral route for transmission of infection is a significant public health concern. It describes how infectious agents spread from contaminated feces to the mouth, often through contaminated food or water. This route can lead to a variety of diseases, highlighting the crucial role of sanitation and hygiene in preventing their transmission. A simple flow chart illustrates this pathway, showing how easily infection can occur.
This article explores the mechanisms behind fecal-oral transmission, the pathogens commonly involved, and the factors that influence their spread. It will also delve into the clinical presentations, diagnosis, prevention strategies, and the global impact of these infections. We will also consider emerging pathogens and future challenges in controlling their transmission.
Introduction to Fecal-Oral Transmission
Fecal-oral transmission is a significant mode of disease spread, where pathogens travel from the feces of an infected individual to the mouth of a susceptible person. This route is a common cause of various infections, often affecting the digestive system. Understanding this pathway is crucial for implementing effective preventive measures.This transmission occurs when contaminated food or water is consumed, or through direct contact with contaminated surfaces or objects.
The cycle involves shedding of pathogens in feces, followed by their ingestion by another person, leading to infection. This process can happen in diverse settings, from contaminated water supplies in developing nations to contaminated food served in restaurants.
Mechanisms of Pathogen Spread
Fecal-oral transmission involves several mechanisms, all stemming from the direct or indirect transfer of pathogens from the infected individual’s feces to the mouth of a susceptible individual. This process can involve contaminated food, water, or even direct contact with contaminated objects or surfaces. The pathogens, which are microscopic organisms capable of causing illness, are excreted in the feces.
These can then contaminate surfaces, food, or water, creating a pathway for transmission. Contaminated food or water is a common vector for the spread of pathogens.
Role of Contaminated Food and Water
Contaminated food and water are key factors in fecal-oral transmission. Food can become contaminated during preparation if hygiene practices are inadequate, such as improper handwashing by food handlers or the use of contaminated utensils. Similarly, water sources can be contaminated by sewage or animal waste, leading to the presence of harmful pathogens. These pathogens then enter the food chain, leading to potential contamination of foods like vegetables, fruits, or even meat products.
- Improper food handling practices, like insufficient handwashing, can introduce pathogens from feces to food, leading to infection in consumers.
- Contaminated water sources, such as wells or rivers polluted by sewage, can harbor pathogens that are then ingested, causing illness.
- Raw or undercooked food, particularly seafood and meat, can carry pathogens that are not eliminated by normal cooking processes, potentially causing illness.
- Food preparation surfaces that are not properly cleaned and disinfected can serve as vectors for the spread of pathogens.
Fecal-Oral Transmission Flowchart
This simple flowchart illustrates the fecal-oral pathway:
| Step | Description |
|---|---|
| 1 | Infected individual excretes pathogens in feces. |
| 2 | Contaminated food or water source comes into contact with the pathogens. |
| 3 | Susceptible individual consumes the contaminated food or water. |
| 4 | Pathogens enter the susceptible individual’s body and cause infection. |
This simple model illustrates the critical steps in the fecal-oral transmission process. Awareness of these steps is vital for prevention.
Pathogens Transmitted via Fecal-Oral Route
The fecal-oral route is a significant mode of pathogen transmission, often overlooked in public health campaigns. This route highlights the crucial link between hygiene, sanitation, and the prevention of infectious diseases. Understanding the specific pathogens involved, their characteristics, and the diseases they cause is essential for effective disease control strategies.
Common Pathogens
A multitude of microorganisms can be transmitted via the fecal-oral route, posing a significant threat to human health. These pathogens vary in their virulence, survival mechanisms, and the diseases they induce. The severity of infection depends on the pathogen’s ability to cause disease, the individual’s immune response, and environmental factors.
Bacterial Pathogens
Bacteria are a significant group of pathogens transmitted via the fecal-oral route. Their diverse survival mechanisms and virulence factors contribute to their ability to cause disease.
- Escherichia coli ( E. coli): E. coli strains, while typically harmless, some are pathogenic. Certain strains produce toxins that cause severe diarrheal illness, ranging from mild to life-threatening conditions. Virulence factors like toxins and fimbriae allow E. coli to adhere to the intestinal lining and cause damage.
- Salmonella spp.: Salmonella bacteria contaminate food and water sources, leading to salmonellosis. The bacteria multiply in the intestines, causing fever, abdominal cramps, and diarrhea. Virulence factors include flagella for motility and fimbriae for adhesion.
- Campylobacter spp.: These bacteria commonly cause food poisoning. They are often associated with undercooked poultry and contaminated water. Symptoms include diarrhea, fever, and abdominal pain. Their spiral shape allows them to penetrate intestinal lining, contributing to their virulence.
Viral Pathogens
Viruses are another significant class of pathogens transmitted via the fecal-oral route. Their reliance on host cells for replication presents challenges in their control.
- Norovirus: This highly contagious virus is a leading cause of viral gastroenteritis, commonly associated with outbreaks in settings like restaurants and cruise ships. The virus’s resistance to various environmental conditions contributes to its widespread transmission. Transmission is rapid due to the virus’s stability in the environment and high infectious dose.
- Rotavirus: Rotavirus infection is a major cause of severe diarrhea in infants and young children. The virus is highly contagious, spreading easily through contaminated food, water, or surfaces. Viral replication in the small intestine causes the characteristic watery diarrhea.
Parasitic Pathogens
Parasitic infections are also prevalent in the fecal-oral transmission route. Their life cycles often involve complex stages, influencing transmission dynamics.
- Giardia lamblia: This protozoan parasite causes giardiasis, a diarrheal illness. It is transmitted through contaminated water sources and often found in areas with poor sanitation. Its cyst form allows for survival outside the host, contributing to its transmission.
- Cryptosporidium spp.: This parasite causes cryptosporidiosis, characterized by watery diarrhea and abdominal cramps. It is known for its resistance to chlorine disinfection, posing a significant threat to waterborne outbreaks. The parasite’s ability to persist in the environment increases its transmissibility.
Categorization of Pathogens by Infection Type, Fecal oral route for transmission of infection
| Pathogen | Disease | Transmission Mode | Symptoms |
|---|---|---|---|
| Escherichia coli O157:H7 | Hemolytic Uremic Syndrome (HUS) | Fecal-oral | Bloody diarrhea, kidney failure |
| Salmonella Typhi | Typhoid Fever | Fecal-oral | Fever, headache, abdominal pain, and sometimes a rash |
| Norovirus | Norovirus Gastroenteritis | Fecal-oral | Vomiting, diarrhea, and stomach cramps |
| Rotavirus | Rotavirus Gastroenteritis | Fecal-oral | Severe watery diarrhea, vomiting, and fever, especially in infants and young children |
| Giardia lamblia | Giardiasis | Fecal-oral | Diarrhea, abdominal cramps, and gas |
| Cryptosporidium | Cryptosporidiosis | Fecal-oral | Watery diarrhea, abdominal cramps, and fever |
Factors Influencing Transmission

The fecal-oral route is a significant pathway for infectious disease transmission, impacting global health disproportionately in regions with limited access to sanitation and hygiene. Understanding the factors that influence this transmission is crucial for developing effective prevention strategies. These factors range from simple hygiene practices to complex socioeconomic and environmental conditions. Analyzing these elements provides insights into how to interrupt the cycle of infection and protect vulnerable populations.The transmission of pathogens via the fecal-oral route is profoundly influenced by a multitude of factors, making it a complex public health concern.
Factors such as hygiene practices, sanitation levels, socioeconomic conditions, and environmental factors all play critical roles in determining the prevalence and intensity of these infections. Understanding these interconnected factors is essential for developing targeted interventions to prevent the spread of diseases.
Hygiene Practices and Transmission
Maintaining high standards of personal hygiene is paramount in preventing fecal-oral transmission. Handwashing, particularly after using the restroom and before handling food, is a cornerstone of infection control. Proper handwashing techniques involve using soap and water, scrubbing hands thoroughly for at least 20 seconds, and ensuring complete rinsing. Consistent adherence to these practices reduces the risk of pathogens transferring from contaminated hands to the mouth.
Sanitation and Safe Water Sources
Sanitation and access to safe water are inextricably linked to the prevention of fecal-oral diseases. Adequate sanitation systems, including proper sewage disposal and waste management, prevent the contamination of water sources and the environment with fecal matter. Safe water sources, such as treated water supplies, are critical in preventing the ingestion of contaminated water. Lack of access to these resources often correlates with higher rates of fecal-oral infections.
Examples include waterborne outbreaks in areas with inadequate water treatment facilities.
Socioeconomic Factors and Transmission Rates
Socioeconomic factors significantly influence the prevalence of fecal-oral diseases. Limited access to clean water, sanitation facilities, and healthcare resources in low-income communities often results in higher transmission rates. Poverty and lack of education contribute to poor hygiene practices, creating a cycle of infection. Inadequate infrastructure and limited access to essential resources often contribute to the spread of diseases.
The fecal-oral route is a common way infections spread, often overlooked. Think about it – contaminated food or water can lead to serious illnesses. Maintaining good hygiene practices is crucial to prevent this. Interestingly, similar to the careful management of sanitation to prevent infections, achieving a euthymic mood in bipolar disorder euthymic mood in bipolar disorder is also about maintaining a stable emotional state, a crucial part of overall well-being.
So, whether it’s preventing infections or managing a mood disorder, careful attention to detail matters in the long run.
For instance, overcrowded living conditions and lack of proper waste disposal in urban slums can lead to widespread contamination.
Environmental Factors Contributing to Contamination
Environmental factors can play a critical role in the contamination of food and water sources. Poorly maintained food handling practices in restaurants or homes, inadequate waste disposal, and the presence of contaminated vectors such as flies and rodents can all contribute to the spread of fecal-oral diseases. Flooding events can contaminate water sources and spread pathogens. Exposure to contaminated soil can lead to ingestion of pathogens through contact with the mouth or food crops.
This underscores the need for comprehensive environmental management to mitigate contamination risks.
Clinical Manifestations and Diagnosis
Understanding the clinical presentations and diagnostic methods for fecal-oral transmitted infections is crucial for timely intervention and effective treatment. These infections, often caused by pathogenic microorganisms, can manifest in a wide array of symptoms, ranging from mild discomfort to severe complications. Accurate diagnosis is paramount to initiating appropriate therapy and preventing further transmission.
The fecal-oral route is a common way infections spread, think about how important handwashing is! It’s crucial to remember proper hygiene to prevent the spread of illness. In fact, using coconut oil for skin care can be beneficial for preventing infections, just like practicing good hygiene can help prevent the fecal-oral route of transmission. Knowing about the fecal-oral route can help us all make better choices about preventing illness.
So, check out how coconut oil for skin can contribute to healthy skin practices, which can help prevent the spread of infections. It’s all interconnected!
Common Clinical Presentations
Fecal-oral infections encompass a broad spectrum of illnesses, with varied clinical presentations depending on the specific pathogen and the individual’s immune status. Some infections may be asymptomatic, while others can cause a wide array of symptoms. Gastrointestinal symptoms are frequently observed, but systemic involvement is also possible. The severity of the infection can range from mild diarrhea to severe dehydration and even life-threatening complications.
Diagnostic Methods
Various diagnostic methods are employed to identify the pathogens responsible for fecal-oral infections. These methods include laboratory tests, imaging techniques, and sometimes even microscopic examinations of stool samples. The selection of diagnostic tools often depends on the suspected pathogen and the clinical presentation.
Symptoms Associated with Fecal-Oral Infections
Fecal-oral infections commonly present with gastrointestinal symptoms. These include:
- Diarrhea: This can range from mild, watery stools to severe, bloody diarrhea. The frequency and consistency of the diarrhea can vary depending on the causative agent.
- Abdominal cramps and pain: These are often associated with inflammation and irritation of the gastrointestinal tract.
- Nausea and vomiting: These symptoms are frequently seen in conjunction with diarrhea and abdominal pain.
- Fever: An elevated body temperature is a common sign of infection, although not always present.
- Dehydration: Severe diarrhea and vomiting can lead to significant fluid loss, potentially causing dehydration, especially in vulnerable populations.
- Headache: Some individuals may experience headaches as a symptom of the infection.
Diagnostic Tests and Their Applications
Accurate diagnosis is crucial for prompt and effective treatment of fecal-oral infections. Various laboratory tests are utilized to identify the causative pathogens. A summary of common diagnostic tests follows:
| Diagnostic Test | Procedure | Pathogen Detected | Sensitivity |
|---|---|---|---|
| Stool Culture | Culturing stool samples under controlled conditions to isolate and identify the presence of bacteria. | Various bacteria (e.g., Salmonella, Shigella, Campylobacter) | Moderate to high, depending on the pathogen and laboratory techniques. |
| Stool Antigen Detection | Detecting specific antigens produced by pathogens in stool samples using immunoassays. | Specific pathogens like Norovirus, Rotavirus | High for some viruses, moderate for others. |
| Stool Microscopy | Examining stool samples under a microscope to identify characteristic morphological features of pathogens or parasites. | Parasites (e.g., Giardia, Cryptosporidium), certain bacteria | Variable, depending on the pathogen and expertise of the examiner. |
| Molecular Diagnostics (PCR) | Amplifying specific genetic material of pathogens using polymerase chain reaction (PCR) techniques. | Wide range of pathogens, including viruses, bacteria, and parasites. | High, often considered the gold standard for pathogen detection. |
Prevention and Control Strategies: Fecal Oral Route For Transmission Of Infection
Fecal-oral transmission poses a significant public health challenge, but proactive measures can effectively mitigate its impact. Implementing robust sanitation, hygiene practices, and vaccination programs, where applicable, are crucial in preventing the spread of these infections. These strategies target vulnerable populations and aim to break the cycle of transmission, ultimately safeguarding public health.
Public Health Measures
Public health measures play a pivotal role in preventing the transmission of fecal-oral diseases. These strategies encompass a range of interventions, including water and sanitation improvements, food safety regulations, and vector control programs. Targeted education and community engagement are essential components for promoting adherence to preventative measures.
Importance of Sanitation and Hygiene
Proper sanitation and hygiene practices are fundamental in interrupting the fecal-oral route of transmission. Effective sanitation systems, including safe disposal of human waste, are crucial for preventing contamination of water sources and food. Hygiene practices, such as handwashing with soap and water, are equally vital in reducing the risk of infection. Washing hands before preparing food, after using the toilet, and after contact with contaminated surfaces is critical.
Vaccination Strategies
Vaccination strategies play a significant role in preventing specific fecal-oral infections. For example, vaccines are available for certain viral and bacterial pathogens transmitted via the fecal-oral route, offering protection against severe disease. Immunization programs, targeting high-risk groups, can significantly reduce the burden of these infections within communities. Vaccination schedules and their effectiveness vary based on the specific pathogen.
The fecal-oral route is a common way infections spread, often overlooked. It’s fascinating how seemingly unrelated conditions like dissociative and conversion disorder can sometimes manifest in ways that highlight the complex interplay of the mind and body. But, let’s get back to the basics – proper hygiene practices remain crucial in preventing the spread of infections transmitted through the fecal-oral route.
Recommendations for Preventing the Spread of Fecal-Oral Diseases
A comprehensive approach to preventing fecal-oral diseases requires a multifaceted strategy. Here’s a list of key recommendations:
- Improved Water and Sanitation Infrastructure: Investing in reliable and accessible water supplies, coupled with proper sanitation facilities, is paramount in reducing contamination of water sources and preventing the spread of pathogens. This includes constructing latrines and ensuring their proper use and maintenance.
- Promoting Hand Hygiene Practices: Education and promotion of regular handwashing with soap and water, especially after using the toilet and before eating, are essential in preventing the spread of fecal-oral pathogens. This should be emphasized in schools, communities, and public spaces.
- Food Safety Regulations and Monitoring: Stringent regulations regarding food handling, preparation, and storage are crucial. Regular inspections and monitoring of food establishments are vital in preventing contamination of food products. Proper food preparation, storage, and handling by individuals are also important.
- Vector Control: Controlling the population of vectors like flies, which can transmit pathogens from contaminated surfaces to food, is crucial. Environmental sanitation, including proper waste disposal and pest control measures, can significantly reduce vector-borne infections.
- Improved Hygiene Practices in Healthcare Settings: Strict adherence to hand hygiene protocols and sanitation standards in healthcare facilities is essential to prevent nosocomial infections (hospital-acquired infections). This includes proper disposal of medical waste and disinfection of surfaces.
- Public Awareness Campaigns: Effective public awareness campaigns can educate communities about the importance of sanitation and hygiene practices, promoting behavioral changes and fostering a culture of prevention. Community-based education programs, especially in schools, are important for instilling good habits from a young age.
Global Impact and Epidemiology
The fecal-oral route of infection is a significant global health concern, impacting millions worldwide. Understanding the global burden, regional variations, and healthcare system strain is crucial for developing effective prevention and control strategies. This section will delve into the epidemiological aspects of these infections, highlighting their impact on various populations and healthcare systems.
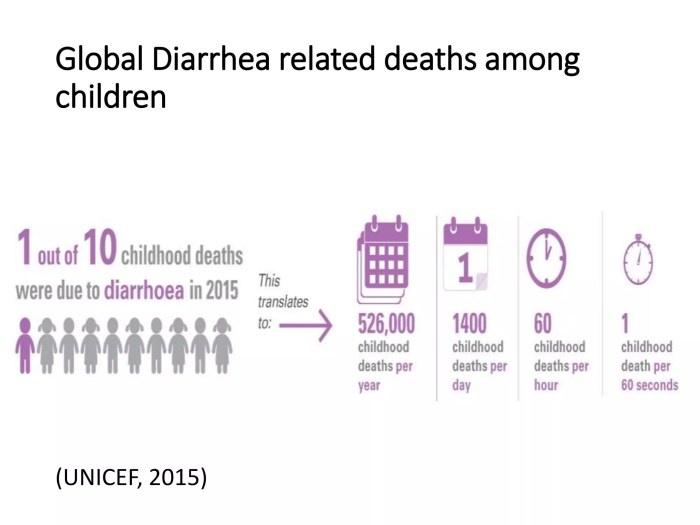
Global Burden of Fecal-Oral Diseases
Fecal-oral infections pose a substantial public health challenge globally. Estimates indicate a considerable burden of disease, primarily affecting developing countries but also presenting a risk in developed nations with inadequate sanitation and hygiene practices. The sheer number of infections translates into substantial healthcare costs and lost productivity, especially in regions with limited access to quality medical care.
Regional Variations in Transmission Rates
Transmission rates of fecal-oral infections vary significantly across different geographical regions. Factors such as sanitation infrastructure, hygiene practices, access to clean water, and socioeconomic conditions play a crucial role in determining the prevalence of these infections. For example, areas with poor sanitation and inadequate access to clean water sources often experience higher rates of diarrheal diseases. This disparity highlights the importance of targeted interventions in specific regions to address the unique challenges and vulnerabilities.
Impact on Healthcare Systems
Fecal-oral infections strain healthcare systems worldwide, particularly in resource-limited settings. The high volume of patients requiring treatment, including intensive care and hospitalization, can overwhelm healthcare facilities, leading to shortages of beds, staff, and essential medical supplies. Additionally, the potential for outbreaks can further exacerbate the strain on resources, requiring rapid response mechanisms and robust surveillance systems.
Socio-economic Consequences
The socio-economic impact of fecal-oral infections is profound. Infections often lead to lost productivity due to illness and treatment, affecting both individual livelihoods and national economies. Children are particularly vulnerable, experiencing developmental delays and reduced educational opportunities due to repeated episodes of illness. Furthermore, these infections can lead to long-term health complications, adding to the overall economic burden.
Emerging Pathogens and Future Challenges
The fecal-oral route continues to be a significant pathway for the transmission of infectious diseases, and the landscape is constantly evolving. Emerging pathogens, often with novel genetic characteristics and transmission patterns, pose a substantial threat to public health. Understanding these new challenges and developing effective strategies for prevention and control is crucial to mitigate future outbreaks.
Emerging Pathogens
The constant evolution of pathogens necessitates ongoing surveillance and adaptation of public health measures. New strains and species, often originating from zoonotic reservoirs, can emerge and exhibit unique transmission properties, increasing the complexity of controlling outbreaks. Examples include certain antibiotic-resistant strains of
- Salmonella* and
- Campylobacter*, as well as novel enteroviruses that can cause severe gastrointestinal illness. These pathogens can display altered virulence factors or enhanced transmissibility, making them more challenging to contain.
Antimicrobial Resistance
Antimicrobial resistance is a critical concern for the treatment of infections transmitted via the fecal-oral route. The overuse and misuse of antibiotics, both in human and veterinary medicine, contribute to the selection and spread of resistant bacteria. This can severely limit treatment options for individuals infected with resistant pathogens. For instance, the rise of carbapenem-resistant Enterobacteriaceae (CRE) poses a significant challenge, making infections like urinary tract infections, bloodstream infections, and pneumonia considerably more difficult to manage.
Treatment options are limited, increasing the risk of mortality and morbidity.
Challenges in Controlling Spread
Controlling the spread of emerging pathogens transmitted via the fecal-oral route presents multifaceted challenges. These pathogens may have novel transmission mechanisms, making traditional control measures less effective. Factors like poor sanitation, inadequate hygiene practices, and the presence of animal reservoirs can exacerbate the spread. Furthermore, globalization and increased human mobility contribute to the rapid dissemination of these pathogens across geographical boundaries.
The need for global collaboration and coordinated efforts to address these challenges is paramount.
Future Research Directions
Further research is crucial to effectively combat the emerging threats posed by fecal-oral pathogens. This includes investigating novel diagnostics, developing new therapeutic agents, and identifying effective preventive strategies. Understanding the genetic basis of pathogen evolution, including the emergence of antibiotic resistance, is vital for developing targeted interventions. Additionally, more research is needed to determine the role of environmental factors and animal reservoirs in pathogen transmission and to evaluate the effectiveness of novel control strategies in real-world settings.
The development of rapid diagnostic tests and the exploration of alternative therapeutic options, such as phage therapy, are promising avenues for future research. Strengthening surveillance systems and improving global collaborations are also essential.
Summary
In conclusion, fecal-oral transmission of infection poses a significant global health challenge. Understanding the mechanisms, pathogens, and factors influencing transmission is critical for developing effective prevention and control strategies. Public health measures, including improved sanitation, hygiene practices, and access to safe water sources, are crucial in minimizing the impact of these infections. Future research should focus on emerging pathogens, antimicrobial resistance, and innovative strategies to combat this ongoing threat.










