Herniated disc surgery overview provides a comprehensive look at this often-debated procedure. Understanding the causes, symptoms, and various surgical approaches is crucial for anyone considering this option. We’ll delve into diagnostic procedures, explore different surgical techniques, and examine post-operative care and potential risks. This guide aims to empower you with the knowledge you need to make informed decisions about your health.
From the initial diagnosis to the long-term recovery process, we’ll cover everything in detail. This in-depth look at herniated disc surgery overview aims to provide clarity and understanding for patients and their families.
Introduction to Herniated Disc Surgery: Herniated Disc Surgery Overview
A herniated disc, also known as a slipped disc, is a common spinal condition where the soft, gel-like center of an intervertebral disc bulges or ruptures through a tear in the tough outer layer. This can put pressure on nearby nerves, causing pain and other symptoms. Understanding the causes, symptoms, and types of herniated discs is crucial for patients and healthcare providers alike.The condition often arises from a combination of factors, including age-related wear and tear, repetitive strain, and certain lifestyle choices.
While genetic predisposition can play a role, most herniated discs result from a combination of environmental and individual factors.
Causes of Herniated Discs
Several factors contribute to the development of herniated discs. Age-related degeneration of the spine is a major contributor, as the discs naturally lose water and elasticity over time. Repetitive lifting, heavy exertion, and poor posture can also strain the spine and increase the risk of a herniated disc. Obesity and a sedentary lifestyle can exacerbate these factors.
Certain occupations, such as those involving repetitive twisting or heavy lifting, are also associated with a higher risk of herniated discs.
Symptoms of a Herniated Disc
Symptoms of a herniated disc vary depending on the location and severity of the herniation. Common symptoms include pain, numbness, tingling, and weakness in the affected area. The pain may radiate along the nerve roots, leading to discomfort in the neck, back, arms, or legs. Muscle weakness or spasms can also accompany a herniated disc. The intensity of the symptoms can range from mild discomfort to severe debilitating pain, which can significantly impact a patient’s quality of life.
Patient Population Affected
Individuals of all ages can experience herniated discs, though some demographics are more susceptible. People in their 30s and 40s often experience these conditions, but even younger individuals can develop them due to intense physical activity. Individuals with jobs requiring repetitive lifting or those who engage in strenuous physical activities are also at higher risk. The risk factors vary and can be influenced by factors such as body mechanics, posture, and lifestyle.
So, you’re looking at herniated disc surgery? It’s a pretty common procedure, often involving removing or repairing the damaged disc. While recovering, you might wonder about your diet. Considering foods like sunflower seeds, are they a good choice for your body’s recovery? It’s a good question to explore.
Finding out if sunflower seeds are good or bad for you might be a useful piece of the puzzle. Is sunflower bad for you ? Knowing more about this could help you make informed choices during your recovery process, ensuring you’re getting the best possible nutrition. Ultimately, a healthy diet, in combination with your doctor’s recommendations, is key to a successful recovery from herniated disc surgery.
Types of Herniated Discs
Herniated discs can occur in various locations within the spine. Understanding the location of the herniation is critical for diagnosis and treatment. There are different classifications based on the location and direction of the herniation. Knowing the specific type of herniation can guide the appropriate treatment plan.
Comparison of Herniated Disc Types
| Type of Herniated Disc | Symptoms | Potential Locations |
|---|---|---|
| Cervical Herniated Disc | Neck pain, arm pain, numbness, tingling in the arm or hand, weakness in the arm or hand | Between the cervical vertebrae (neck region) |
| Thoracic Herniated Disc | Pain in the upper back, radiating to the chest, shoulder, or arm, potentially causing difficulty breathing or swallowing | Between the thoracic vertebrae (upper back region) |
| Lumbar Herniated Disc | Lower back pain, radiating pain down the leg (sciatica), numbness, tingling, or weakness in the leg or foot | Between the lumbar vertebrae (lower back region) |
Diagnostic Procedures
Unraveling the mystery of a herniated disc starts with accurate diagnosis. Various tests help pinpoint the location, severity, and impact of the herniation on surrounding nerves. A thorough understanding of these procedures is crucial for developing an effective treatment plan.Understanding the rationale behind each diagnostic test is paramount. Each method contributes unique information, allowing healthcare professionals to piece together the complete picture of the patient’s condition.
This detailed analysis ultimately guides the most appropriate course of action.
Common Diagnostic Tests
A comprehensive approach to diagnosis often involves a combination of tests. These methods are carefully selected based on the patient’s symptoms and medical history. A key component is the initial physical examination, which assesses range of motion, neurological function, and the presence of any pain or numbness.
Imaging Techniques
Imaging techniques provide crucial visual information about the spine and surrounding tissues. They are essential for identifying herniated discs and ruling out other potential causes of pain.
- Magnetic Resonance Imaging (MRI): MRI uses strong magnetic fields and radio waves to create detailed images of the soft tissues within the body, including the spinal cord and discs. It is particularly effective at visualizing the structure of the disc, identifying herniations, and assessing the overall health of the spinal tissues. MRI is highly sensitive to detecting herniated discs and is often the preferred imaging modality for this purpose.
For example, a patient experiencing severe back pain radiating down the leg might undergo an MRI to pinpoint the location and extent of a herniated disc. The resulting images will show the disc’s structure, revealing any tears, bulges, or protrusions.
- Computed Tomography (CT) Scan: A CT scan uses X-rays to create cross-sectional images of the body. It provides detailed information about the bony structures of the spine, such as vertebrae and joints. CT scans are especially useful in identifying fractures, bone spurs, or other bony abnormalities that might be contributing to the pain. While CT scans are not as good at visualizing soft tissues as MRIs, they can still help pinpoint the exact location of a herniated disc if it’s associated with a bony abnormality.
For instance, a patient with a history of trauma to the back might undergo a CT scan to rule out any fractures or other bony issues that could be contributing to their symptoms.
Comparison of Imaging Techniques
Both MRI and CT scans play crucial roles in diagnosing herniated discs, but they differ in their strengths and weaknesses.
| Diagnostic Procedure | Purpose | Typical Results |
|---|---|---|
| MRI | Detailed visualization of soft tissues, including spinal cord and discs | Images showing the disc’s structure, herniations, and surrounding tissues. |
| CT Scan | Detailed visualization of bony structures | Images showing the vertebrae, joints, and potential bony abnormalities. |
A typical diagnostic process for a suspected herniated disc involves a combination of these methods. Firstly, a thorough patient history and physical examination are conducted. Then, appropriate imaging studies, such as MRI or CT scans, are ordered based on the initial findings. The results of these tests are carefully analyzed, and a definitive diagnosis is reached. This multi-step approach ensures accurate identification of the problem and helps determine the best course of treatment.
Surgical Procedures Overview
Choosing the right surgical approach for a herniated disc is crucial for effective treatment and minimizing complications. This involves careful consideration of the specific location and severity of the herniation, the patient’s overall health, and the surgeon’s expertise. Different surgical techniques offer varying degrees of invasiveness, impacting recovery time and potential risks. Understanding these nuances is essential for informed decision-making.
Surgical Approaches for Herniated Disc Repair
Various surgical approaches are employed to repair herniated discs, each with its own advantages and disadvantages. These procedures aim to alleviate pressure on the spinal nerves, reducing pain and restoring function. Factors influencing the chosen approach include the size and location of the herniation, the patient’s condition, and the surgeon’s preference.
Minimally Invasive Techniques
Minimally invasive techniques are gaining popularity for herniated disc surgery. These procedures typically involve smaller incisions, less tissue disruption, and reduced recovery time compared to traditional open surgery. Minimally invasive approaches often utilize specialized instruments and advanced imaging guidance to precisely target the affected area, thereby minimizing damage to surrounding structures. This approach is beneficial for patients seeking a faster return to normal activities.
Comparison of Surgical Approaches
| Surgical Approach | Benefits | Risks |
|---|---|---|
| Open Discectomy | Direct access to the herniated disc for complete removal; suitable for complex cases. | Larger incision, potentially increased blood loss, longer recovery time, greater risk of scarring and nerve damage. |
| Minimally Invasive Discectomy | Smaller incisions, less tissue trauma, faster recovery, less post-operative pain. | Limited access to the herniated disc; might not be suitable for complex cases; risk of instrument malposition or nerve damage, although lower than open surgery. |
| Endoscopic Discectomy | Very small incisions, minimal tissue disruption, extremely precise removal of the herniated disc. | Requires specialized instruments and skill; less access than minimally invasive, potential for complications with instrument use and nerve damage. |
Role of Spinal Fusion in Treating Herniated Discs, Herniated disc surgery overview
Spinal fusion is a procedure where two or more vertebrae are permanently joined together to stabilize the spine. It is sometimes used in conjunction with herniated disc surgery, particularly when there is significant instability in the spine or when the herniation is associated with degenerative disc disease. The decision to perform spinal fusion is individualized, considering the specific situation and expected outcomes.
Open vs. Minimally Invasive Surgery
The choice between open and minimally invasive surgery for herniated discs depends on the specific situation. Open surgery offers greater access and visualization but comes with a longer recovery period. Minimally invasive techniques, while often preferred for their reduced invasiveness, may not be suitable for all cases. A discussion with the surgeon will help determine the most appropriate option based on the individual patient’s needs.
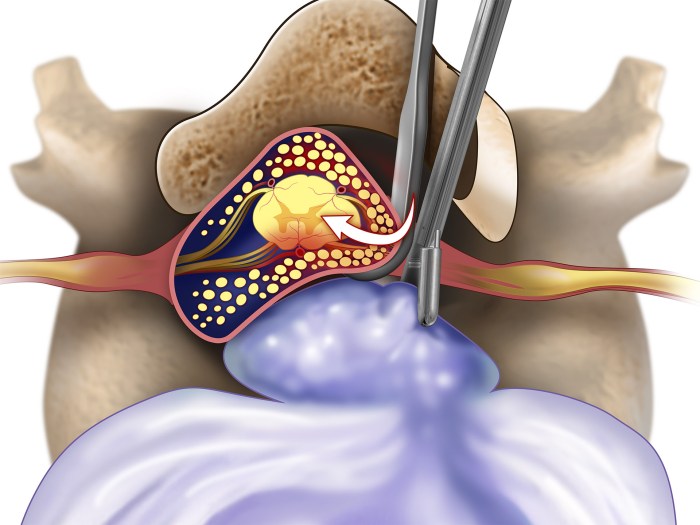
Microdiscectomy: A Common Surgical Procedure
Microdiscectomy is a minimally invasive surgical procedure that aims to relieve pressure on the spinal nerves caused by a herniated disc. During the procedure, the surgeon makes a small incision and uses specialized instruments to remove the herniated portion of the disc. This approach minimizes damage to surrounding tissues and nerves, facilitating a faster recovery for the patient.
The specific steps may vary depending on the surgeon’s preference and the patient’s individual condition.
Key steps often include:
- Imaging guidance: The surgeon uses X-rays, CT scans, or MRI to precisely locate the herniated disc.
- Small incision: A small incision is made in the skin over the affected area.
- Exposure of the disc: The surgeon carefully removes the surrounding tissues to expose the herniated disc.
- Disc removal: The herniated portion of the disc is removed.
- Closure: The incision is closed with sutures.
Post-Operative Care and Recovery
Recovering from herniated disc surgery is a journey, not a sprint. While the surgical procedure addresses the immediate issue, a significant period of post-operative care and rehabilitation is crucial for long-term success. This involves meticulous adherence to instructions, diligent participation in physical therapy, and proactive management of potential complications. A well-structured approach ensures a smoother recovery and minimizes the risk of setbacks.The recovery period after herniated disc surgery is highly variable, depending on the individual’s overall health, the extent of the herniation, and the specific surgical technique employed.
Generally, patients experience a period of healing, initially focused on managing pain and inflammation, then gradually transitioning to strengthening muscles and regaining lost mobility. Patience and consistent effort are key to achieving optimal results.
Typical Recovery Period
The initial recovery period often involves pain management and the gradual resumption of activities. Depending on the procedure and the individual’s condition, this can last anywhere from several weeks to several months. Early mobility, though with limitations, is encouraged to prevent complications like blood clots and stiffness. During this phase, pain medication is often prescribed, and physical therapy plays a critical role in regaining strength and flexibility.
Post-operative pain typically subsides over time as the body heals.
Importance of Physical Therapy and Rehabilitation
Physical therapy is essential for regaining strength, mobility, and flexibility after surgery. A structured physical therapy program helps patients safely and effectively recover their range of motion, rebuild core strength, and improve posture. It teaches exercises to strengthen muscles that support the spine, helping to prevent future issues. A personalized plan tailored to the individual’s progress and limitations is vital.
The goal is to enable patients to return to their normal activities as soon as possible.
Potential Complications
While herniated disc surgery is generally safe, potential complications can arise. These include infection, bleeding, nerve damage, persistent pain, and delayed healing. However, these complications are less frequent with improved surgical techniques and meticulous post-operative care. Prompt medical attention is crucial if any unusual symptoms arise. Proper communication with the surgical team and adherence to post-operative instructions significantly reduce the risk of complications.
Role of Pain Management
Effective pain management is vital during the recovery period. A multi-modal approach, including medication, physical therapy, and potentially other non-pharmacological techniques, helps to control pain and promote healing. The goal is to manage pain effectively without compromising mobility or recovery. Open communication with the medical team is key to adjusting pain management strategies as needed.
Common Activities and Exercises
As part of the recovery process, patients are encouraged to engage in activities and exercises that promote healing and gradual return to function. This could include gentle stretching, walking, and progressively more challenging exercises as tolerated. Swimming, yoga, and other low-impact activities can also be beneficial. It’s crucial to follow the guidance of physical therapists and medical professionals to avoid exacerbating the injury or causing further complications.
Post-Operative Care and Recommendations
- Follow all prescribed medications and instructions: Strict adherence to the prescribed medications, including pain relievers and antibiotics, is crucial for effective pain management and infection prevention.
- Maintain good posture: Maintaining proper posture throughout the day is important to prevent further strain on the spine and promote healing.
- Engage in prescribed physical therapy exercises: Regular participation in physical therapy exercises is vital for regaining strength and flexibility.
- Report any unusual symptoms: Prompt reporting of any unusual symptoms, such as increased pain, swelling, or fever, is essential for timely intervention.
- Avoid heavy lifting and strenuous activities: Heavy lifting and strenuous activities should be avoided during the recovery period to prevent further injury to the spine.
- Gradual return to normal activities: Returning to normal activities should be gradual and progressive, as advised by the medical team.
Potential Risks and Complications
While herniated disc surgery is generally safe and effective, like any surgical procedure, it carries potential risks and complications. Understanding these risks is crucial for informed decision-making alongside your healthcare provider. Thorough pre-operative discussions and careful surgical technique can significantly minimize these risks.Careful consideration of the specific anatomy and the patient’s overall health is paramount. The choice of surgical approach plays a vital role in mitigating complications.
The potential benefits must be weighed against the potential drawbacks, ensuring that the procedure aligns with the individual patient’s needs and goals.
Potential Surgical Complications
Surgical procedures, even minimally invasive ones, involve inherent risks. These include bleeding, infection, nerve damage, and the possibility of the disc herniation recurring. The likelihood of each complication varies based on several factors, including the patient’s overall health, the severity of the herniation, and the surgical technique employed.
Likelihood and Management of Complications
| Potential Risk/Complication | Likelihood | Management Strategies |
|---|---|---|
| Bleeding | Moderate | Careful surgical technique, blood transfusions if needed, monitoring for signs of excessive bleeding. |
| Infection | Low, but possible | Antibiotics, meticulous surgical technique, wound care, monitoring for signs of infection. |
| Nerve Damage | Low, but potential for lasting effects | Careful surgical technique, meticulous dissection of nerves, postoperative neurological evaluation. |
| Recurrence of Herniation | Low, but possible | Careful surgical technique, addressing the underlying cause of the herniation, follow-up care. |
| Blood clots | Low | Compression stockings, leg exercises, blood thinners if indicated. |
| Dural tears | Low | Careful surgical technique, dural repair if necessary, monitoring for cerebrospinal fluid leaks. |
Long-Term Effects
Long-term effects of herniated disc surgery can vary significantly. Some patients experience complete pain relief and return to normal activities. Others may experience lingering pain, weakness, or numbness. Factors such as the severity of the initial herniation, the extent of the surgical intervention, and individual patient response play a critical role in determining long-term outcomes.
Comparison of Surgical Approaches
Different surgical approaches for herniated disc surgery, such as microdiscectomy, endoscopic discectomy, and open discectomy, have varying levels of invasiveness and associated risks. Microdiscectomy, for instance, is often considered less invasive but may not be suitable for all cases. Endoscopic discectomy uses small incisions and specialized instruments, potentially reducing recovery time. Open discectomy, while more invasive, provides greater access and is suitable for complex cases.
Herniated disc surgery, while often successful, can sometimes lead to post-operative nausea and vomiting. Understanding the potential causes of these common side effects is key to effective recovery. For a deeper dive into the various triggers behind nausea and vomiting, check out this helpful resource on causes of nausea and vomiting. Ultimately, proper management of these symptoms is crucial for a smooth and comfortable recovery from herniated disc surgery.
The best approach depends on the specific characteristics of the herniation and the patient’s individual needs.
Steps to Take if Complications Arise
If complications arise after herniated disc surgery, immediate communication with your surgeon is crucial. Detailed documentation of the symptoms and the timing of their onset is essential. Prompt medical attention is critical for effective management of any complications. Follow your surgeon’s instructions carefully and attend all scheduled follow-up appointments. Open communication and a collaborative approach between the patient and the healthcare team are essential for optimal outcomes.
Alternatives to Surgery
A herniated disc can be a painful and debilitating condition, but surgery isn’t always the first or best option. Many individuals find relief through non-surgical treatments, which often offer a less invasive approach to managing symptoms and potentially preventing the need for more drastic measures. Understanding these alternatives is crucial for making informed decisions about your health journey.Conservative therapies are frequently the first line of treatment for herniated discs.
These methods focus on relieving pain, improving function, and promoting healing without resorting to surgery. The effectiveness of these therapies can vary greatly depending on the individual and the severity of the herniated disc.
Non-Surgical Treatment Options
Conservative therapies aim to reduce pain and inflammation, improve spinal mobility, and promote healing without surgery. These methods typically involve a combination of approaches tailored to the specific needs of the patient. Successful outcomes often depend on consistent adherence to the prescribed treatment plan.
So, I’ve been researching herniated disc surgery lately, and it’s a pretty big deal. Recovery can be a long haul, and honestly, some of the post-op symptoms can be surprisingly varied. For example, you might experience some unexpected things like heart palpitations at night, which can be concerning. Thankfully, resources like this heart palpitations at night page can help you understand these potential side effects better.
Overall, understanding the entire spectrum of potential issues is key to making informed decisions about your treatment plan for herniated disc surgery.
- Physical Therapy: Physical therapists develop personalized exercise programs to strengthen core muscles, improve posture, and increase flexibility. These exercises are crucial for stabilizing the spine and reducing stress on the affected area. Examples include targeted stretches, strengthening exercises for the abdominal and back muscles, and specific exercises for improving posture. Proper guidance from a qualified physical therapist is essential for achieving optimal results.
- Medications: Over-the-counter pain relievers, such as ibuprofen or naproxen, can help reduce inflammation and pain. Prescription medications, like muscle relaxants or stronger pain medications, might be necessary in more severe cases. These are typically used in conjunction with other treatments and under the supervision of a medical professional.
- Epidural Steroid Injections: These injections deliver corticosteroids directly into the epidural space around the affected nerve roots. This can reduce inflammation and pain, providing temporary relief. These injections are often considered for short-term pain management, but their effectiveness varies from person to person and may not be suitable for all cases.
- Spinal Decompression Therapy: This therapy aims to reduce pressure on the nerve roots by gently stretching the spine. Different techniques, such as traction or intermittent decompression, can be employed. The effectiveness of spinal decompression varies, and its suitability depends on the specific condition and the patient’s response.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. Acupuncture is believed to stimulate the flow of energy, reduce pain, and promote healing. While some individuals experience relief from acupuncture, its effectiveness for herniated discs is not universally recognized by the medical community.
Effectiveness of Conservative Therapies
The effectiveness of non-surgical treatments for herniated discs depends on several factors, including the severity of the herniation, the location of the herniation, and the individual’s overall health. In many cases, conservative therapies provide significant pain relief and improved function, allowing patients to avoid the risks and potential complications of surgery. For example, a patient with a mild herniation and a history of successful physical therapy for back pain might benefit from continued conservative management.
Conversely, a patient with severe nerve compression requiring immediate intervention may not be a good candidate for non-surgical treatments alone.
Circumstances Favoring Non-Surgical Treatments
Non-surgical treatments are often preferred over surgery when the herniated disc is relatively small, the symptoms are manageable, and the patient is a good candidate for conservative therapies. Factors such as age, overall health, and the presence of other medical conditions are also considered. For instance, if a younger patient with a manageable herniation demonstrates a positive response to physical therapy, conservative management might be a preferred approach.
Comparison of Non-Surgical Treatments
| Treatment | Effectiveness | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Physical Therapy | High | Improves core strength, posture, flexibility | Requires commitment and consistency |
| Medications | Moderate | Provides pain relief | Potential for side effects, may not address underlying cause |
| Epidural Steroid Injections | Variable | Temporary pain relief | Potential for complications, limited long-term effectiveness |
| Spinal Decompression Therapy | Limited evidence | Potential for reduced pressure | Potential for side effects, not universally accepted |
| Acupuncture | Limited evidence | Potential for pain relief | Not a mainstream medical treatment, limited scientific backing |
Patient Experiences and Outcomes

Herniated disc surgery aims to alleviate pain and restore function, but the patient experience is multifaceted. Outcomes vary greatly, depending on individual factors, the severity of the herniation, the surgical approach, and post-operative care. Understanding these factors is crucial for patients considering this procedure and their expectations for recovery.
General Overview of Patient Outcomes
Success rates for herniated disc surgery are generally high, with many patients experiencing significant pain relief and improved quality of life. However, complete recovery isn’t guaranteed for every individual, and factors such as pre-existing conditions and individual responses to treatment can influence the outcome.
Patient Satisfaction Rates with Different Surgical Approaches
Patient satisfaction with minimally invasive surgical techniques, such as endoscopic discectomy, often shows higher rates of early recovery and reduced post-operative pain compared to traditional open procedures. These differences are often attributed to less tissue trauma and a smaller incision size. However, long-term outcomes may vary between techniques, emphasizing the importance of individual consultation with a surgeon.
Factors Influencing Patient Recovery
Several factors play a role in a patient’s recovery journey after herniated disc surgery. These include pre-operative health conditions, adherence to post-operative instructions, and the patient’s overall lifestyle and willingness to engage in rehabilitation.
- Pre-existing health conditions: Conditions like diabetes or cardiovascular issues can potentially complicate recovery. Patients with pre-existing conditions may require specialized care and management during the recovery period.
- Adherence to post-operative instructions: Following prescribed medication schedules, physical therapy regimens, and activity restrictions are critical for successful recovery. Failure to adhere to these guidelines can hinder progress and potentially lead to complications.
- Patient’s overall lifestyle and willingness to engage in rehabilitation: Maintaining a healthy lifestyle that includes regular exercise, a balanced diet, and sufficient rest, coupled with a commitment to rehabilitation exercises, significantly impacts the healing process.
Illustrative Examples of Successful Recovery Stories
Numerous patients report successful recovery following herniated disc surgery. These experiences often involve a combination of factors, such as diligent adherence to post-operative care, proactive participation in physical therapy, and a positive mindset.
“After my surgery, I followed the doctor’s instructions meticulously. The pain subsided quickly, and with consistent physical therapy, I regained my mobility and strength within several months.”
John Smith, 45.
Importance of Patient Education and Preparation
Thorough education about the surgical procedure, potential risks, and the recovery process is vital for patient preparedness and realistic expectations. This education should cover not only the physical aspects but also the emotional and psychological aspects of the journey.
Factors Impacting Patient Outcomes
| Factor | Description | Potential Impact on Outcome |
|---|---|---|
| Pre-operative health | Presence of pre-existing conditions like diabetes or cardiovascular disease. | May increase the risk of complications and slow recovery. |
| Surgical approach | Minimally invasive versus traditional open procedures. | May affect recovery time, pain management, and potential complications. |
| Patient adherence to post-op instructions | Following prescribed medication, therapy, and activity restrictions. | Directly correlates with recovery speed and success. |
| Post-operative rehabilitation | Engagement in physical therapy and exercises. | Essential for regaining strength, mobility, and pain relief. |
| Lifestyle factors | Diet, exercise, stress levels. | Influence overall healing and recovery time. |
Conclusive Thoughts
In conclusion, herniated disc surgery overview highlights the complexity of this procedure. While it can offer significant relief for debilitating pain, it’s essential to weigh the potential benefits against the risks and explore all available options. Understanding the diagnostic process, surgical procedures, and recovery is key to making the right decision. We encourage further research and open communication with healthcare professionals to achieve the best possible outcomes.










