Hyperinsulinemia is associated with type 2 diabetes, a critical link often overlooked. This condition, characterized by persistently high insulin levels, is a key player in the development of type 2 diabetes. We’ll delve into the mechanisms, pathophysiology, diagnosis, and management strategies surrounding this significant health concern.
Understanding the intricate relationship between hyperinsulinemia and insulin resistance is crucial for effective prevention and treatment. The following sections will provide a comprehensive overview of this complex issue, supported by detailed tables, case studies, and explanations.
Introduction to Hyperinsulinemia and Type 2 Diabetes

Hyperinsulinemia, characterized by elevated levels of insulin in the blood, is a key factor in the development and progression of type 2 diabetes. This condition arises from an imbalance in the body’s intricate system of regulating blood glucose. Understanding the mechanisms behind hyperinsulinemia and its connection to insulin resistance is crucial for effective prevention and management of type 2 diabetes.Hyperinsulinemia often develops as a compensatory response to insulin resistance.
The body, struggling to effectively utilize insulin to transport glucose from the bloodstream into cells, prompts the pancreas to secrete more insulin. This initial increase in insulin production helps maintain normal blood glucose levels, but over time, the sustained high insulin levels can lead to further complications, including insulin resistance becoming more pronounced. The body’s cells become less responsive to the insulin signals, and the cycle of hyperinsulinemia and insulin resistance deepens.
The consequence is a gradual decline in glucose uptake and an increased risk of developing type 2 diabetes.
Mechanisms of Hyperinsulinemia
Hyperinsulinemia arises from a complex interplay of factors. A primary contributor is insulin resistance, where cells fail to respond adequately to insulin’s signaling, leading to reduced glucose uptake. This resistance necessitates the pancreas to increase insulin production to compensate. Genetic predisposition, lifestyle factors (diet, physical inactivity), and obesity further contribute to this imbalance. Metabolic disorders like dyslipidemia and inflammation also play a role in the development of hyperinsulinemia.
In some cases, tumors in the pancreas can also lead to excessive insulin secretion.
Relationship Between Hyperinsulinemia and Type 2 Diabetes
Hyperinsulinemia is a significant precursor to type 2 diabetes. Elevated insulin levels, while initially helping to maintain blood glucose, can lead to a chronic state of insulin resistance. This prolonged exposure to high insulin levels can damage beta cells in the pancreas, ultimately reducing their ability to produce sufficient insulin. This combination of insulin resistance and impaired insulin secretion creates a vicious cycle, pushing the individual closer to a diagnosis of type 2 diabetes.
For example, individuals with a family history of type 2 diabetes and a sedentary lifestyle, combined with high-fat diets, may exhibit hyperinsulinemia that progresses to type 2 diabetes.
Role of Insulin Resistance in Progression
Insulin resistance is the core driver behind the progression of hyperinsulinemia and type 2 diabetes. When cells don’t respond effectively to insulin, the body tries to compensate by increasing insulin production. This continuous demand on the pancreas eventually exhausts its capacity to maintain normal insulin levels, leading to a state of hyperinsulinemia. The more insulin resistant the cells become, the greater the compensatory response and the more pronounced the hyperinsulinemia.
Hyperinsulinemia, a condition where your body produces too much insulin, is strongly linked to type 2 diabetes. While managing this can sometimes involve lifestyle changes, exploring options like different types of cosmetic dental procedures might seem unrelated, but maintaining good oral health is crucial for overall well-being. Ultimately, addressing hyperinsulinemia is key to preventing or managing type 2 diabetes.
Over time, this can result in a disruption of metabolic homeostasis and the development of type 2 diabetes.
Clinical Significance of Identifying Hyperinsulinemia
Early identification of hyperinsulinemia in individuals at risk for type 2 diabetes is crucial. This allows for timely interventions to address the underlying causes and potentially prevent the onset of the disease. Regular monitoring of blood glucose and insulin levels, coupled with lifestyle modifications, can help mitigate the progression of hyperinsulinemia. This proactive approach is critical for preventing the long-term complications associated with type 2 diabetes, such as cardiovascular disease and nerve damage.
Early detection allows for interventions such as dietary changes, exercise, and medications to prevent or delay the development of type 2 diabetes.
Comparison of Normal Insulin Function and Hyperinsulinemia
| Condition | Insulin Action | Symptoms | Risk Factors |
|---|---|---|---|
| Normal Insulin Function | Insulin effectively facilitates glucose uptake into cells, maintaining stable blood glucose levels. | No noticeable symptoms. | Healthy diet, regular exercise, no family history of type 2 diabetes. |
| Hyperinsulinemia | Sustained elevated insulin levels in the blood due to impaired insulin action, often as a compensatory response to insulin resistance. | May include increased hunger, fatigue, excessive thirst, frequent urination, and weight gain. | Family history of type 2 diabetes, obesity, sedentary lifestyle, high-fat diet, and certain medications. |
Pathophysiology of Hyperinsulinemia-Associated Type 2 Diabetes
Hyperinsulinemia, a condition characterized by persistently elevated insulin levels in the blood, is a key factor in the development of type 2 diabetes. This elevated insulin response, initially a compensatory mechanism to overcome insulin resistance, eventually leads to further complications and metabolic dysfunction. Understanding the intricate pathophysiological mechanisms behind this association is crucial for effective prevention and management strategies.The underlying molecular mechanisms linking hyperinsulinemia to insulin resistance involve a complex interplay of factors.
Insulin resistance, a hallmark of type 2 diabetes, occurs when cells fail to respond adequately to insulin signals. This diminished response leads to the body producing more insulin to compensate for the reduced effectiveness. Over time, this compensatory hyperinsulinemia can further impair insulin signaling pathways, creating a vicious cycle that worsens insulin resistance and elevates blood glucose levels.
This feedback loop is crucial in understanding the progression of the disease.
Molecular Mechanisms of Insulin Resistance
Insulin resistance stems from various molecular defects. Impaired insulin receptor signaling, including decreased insulin receptor tyrosine kinase activity, is a primary mechanism. Furthermore, defects in intracellular signaling pathways, such as reduced glucose uptake and utilization within cells, also contribute to insulin resistance. Disruptions in downstream signaling molecules and proteins can also affect insulin action.
Feedback Loops in Glucose Homeostasis
The development of hyperinsulinemia is intricately linked to the feedback loops within glucose homeostasis. Elevated blood glucose levels trigger a cascade of events that stimulate the pancreas to release more insulin. This increase in insulin secretion is meant to lower blood glucose, but the chronic nature of insulin resistance renders this mechanism ineffective. The resulting hyperinsulinemia, in turn, can further impair insulin sensitivity, perpetuating the cycle of hyperglycemia and hyperinsulinemia.
Hyperinsulinemia, a condition where your body produces too much insulin, is strongly linked to type 2 diabetes. Understanding how this excess insulin affects the body is crucial. For instance, it’s important to consider the interplay of various factors, like quadriceps and back health how do they relate, as well. This connection might seem unusual, but maintaining optimal muscle function, as detailed in this article quadriceps and back health how do they relate , ultimately impacts overall metabolic health and contributes to the development of hyperinsulinemia and its association with type 2 diabetes.
Ultimately, recognizing the multifaceted nature of health is key to managing this condition.
This cycle contributes significantly to the progressive nature of type 2 diabetes.
Role of Genetics and Environmental Factors
Genetic predisposition plays a crucial role in the development of hyperinsulinemia and type 2 diabetes. Certain genes can influence insulin secretion, insulin sensitivity, and the metabolic pathways involved in glucose regulation. Environmental factors, such as diet, physical activity, and lifestyle choices, significantly modulate the expression of these genetic predispositions. Individuals with a genetic predisposition to insulin resistance may be more susceptible to developing hyperinsulinemia and type 2 diabetes when exposed to obesogenic environments or sedentary lifestyles.
Hyperinsulinemia, a condition where your body produces too much insulin, is often linked to type 2 diabetes. Managing stress is crucial in this context, as chronic stress can impact insulin sensitivity. Finding healthy ways to de-stress, like practicing mindfulness or engaging in regular exercise, can significantly improve insulin function. This is important because, in turn, it can help manage blood sugar levels and potentially reduce the risk of developing type 2 diabetes.
For more tips on how to reduce stress, check out this helpful guide: how to reduce stress. Ultimately, a holistic approach to managing stress and lifestyle factors is key to preventing or controlling hyperinsulinemia and the associated risks of type 2 diabetes.
Impact of Obesity and Other Metabolic Disorders
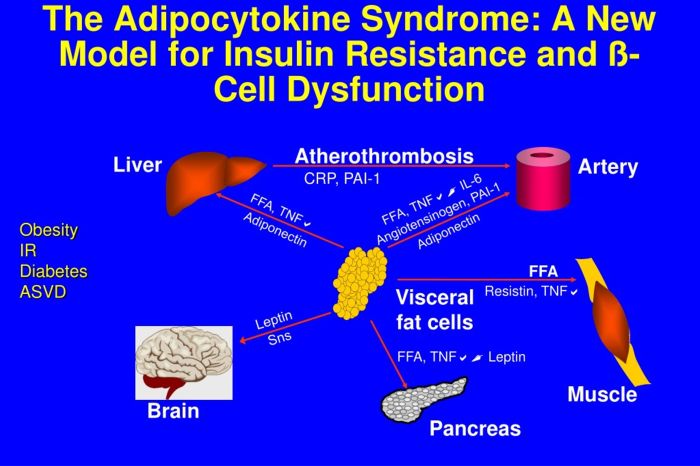
Obesity is a significant risk factor for hyperinsulinemia and type 2 diabetes. Adipose tissue, particularly visceral fat, secretes factors that impair insulin sensitivity and promote insulin resistance. Furthermore, other metabolic disorders, such as dyslipidemia (abnormal blood lipid levels) and hypertension, often co-occur with hyperinsulinemia and type 2 diabetes, exacerbating the disease process. These factors further contribute to the development and progression of the metabolic syndrome.
Comparison of Normal Insulin Levels vs. Hyperinsulinemia
| Body System | Normal Insulin | Hyperinsulinemia | Implications |
|---|---|---|---|
| Glucose Homeostasis | Maintains blood glucose levels within a narrow range | Unable to effectively regulate blood glucose, leading to hyperglycemia | Increased risk of type 2 diabetes, potential complications like cardiovascular disease and neuropathy |
| Lipid Metabolism | Facilitates proper lipid metabolism and storage | Can lead to dyslipidemia (high triglycerides, low HDL), potentially increasing cardiovascular risk | Increased risk of atherosclerosis, heart disease, and stroke |
| Blood Pressure Regulation | Supports healthy blood pressure | May contribute to hypertension through various mechanisms, such as sodium retention | Increased risk of cardiovascular disease, kidney disease |
| Energy Balance | Promotes appropriate energy storage and utilization | Potentially contributes to weight gain and difficulty losing weight | Further exacerbates insulin resistance, increasing the risk of developing type 2 diabetes |
Diagnosis and Assessment of Hyperinsulinemia
Unraveling the intricacies of hyperinsulinemia requires a meticulous diagnostic approach. Simply put, diagnosing hyperinsulinemia involves a combination of clinical evaluation and specific laboratory tests. This process helps differentiate between various causes and guides the development of effective treatment strategies.The diagnostic journey for hyperinsulinemia often begins with a thorough understanding of the patient’s medical history, lifestyle factors, and family history.
A careful consideration of symptoms, such as unexplained weight gain, fatigue, or frequent urination, plays a crucial role in suspecting the presence of hyperinsulinemia.
Diagnostic Criteria for Hyperinsulinemia
Precise diagnostic criteria for hyperinsulinemia are not standardized to a single, definitive test. Instead, it’s often a constellation of findings that suggest the condition, usually in conjunction with signs of insulin resistance. These include elevated fasting insulin levels, impaired glucose tolerance, and a family history of type 2 diabetes. Clinicians employ a multi-faceted approach, combining various assessments to arrive at a conclusive diagnosis.
Insulin Level Measurement Tests
Various tests are used to measure insulin levels and assess insulin resistance. These tests provide crucial insights into the body’s response to insulin.
- Fasting Insulin Test: This test measures insulin levels after an overnight fast. Elevated fasting insulin levels often suggest hyperinsulinemia, particularly when coupled with other indicators of insulin resistance.
- Oral Glucose Tolerance Test (OGTT): The OGTT assesses how the body processes glucose after consuming a sugary drink. This test helps identify impaired glucose tolerance, a key characteristic of insulin resistance. The test involves measuring blood glucose levels at various time points after glucose ingestion.
- Insulin Resistance Tests: Direct assessments of insulin resistance often involve measuring the body’s response to an insulin challenge. One common test involves measuring the amount of glucose uptake in response to an administered dose of insulin.
Interpretation of Diagnostic Test Results
Interpreting the results of these tests requires careful consideration of the patient’s overall clinical picture. Elevated insulin levels, in conjunction with impaired glucose tolerance, are often indicative of hyperinsulinemia. A detailed evaluation considering factors such as age, weight, and lifestyle choices is critical.
Clinical Evaluation Process, Hyperinsulinemia is associated with type 2 diabetes
A thorough clinical evaluation is paramount for patients suspected of having hyperinsulinemia. This involves a comprehensive assessment encompassing a detailed patient history, physical examination, and the aforementioned laboratory tests. The goal is to gather comprehensive data to identify underlying causes and formulate an appropriate treatment plan.
Diagnostic Tests for Hyperinsulinemia
| Test | Procedure | Normal Range | Abnormal Findings |
|---|---|---|---|
| Fasting Insulin | Blood sample drawn after an overnight fast. | Typically below 15 mU/L | Levels consistently above 15 mU/L suggest hyperinsulinemia. |
| Oral Glucose Tolerance Test (OGTT) | Patient consumes a glucose solution, and blood glucose levels are measured at specific intervals. | Normal glucose response throughout the test. | Impaired glucose tolerance, with elevated blood glucose levels after glucose ingestion. |
| Insulin Resistance Tests | Measuring the body’s response to an insulin challenge. | Normal insulin sensitivity. | Reduced glucose uptake in response to insulin indicates insulin resistance. |
Management Strategies for Hyperinsulinemia-Associated Type 2 Diabetes
Hyperinsulinemia, a condition characterized by elevated insulin levels in the blood, is a significant factor contributing to the development and progression of type 2 diabetes. Effective management of hyperinsulinemia is crucial for mitigating the associated health risks and improving long-term outcomes. This involves a multifaceted approach encompassing lifestyle modifications, medication interventions, and ongoing monitoring.Managing hyperinsulinemia in type 2 diabetes necessitates a comprehensive strategy tailored to individual needs.
Addressing the underlying factors driving hyperinsulinemia, such as insulin resistance and impaired glucose tolerance, is essential for achieving optimal metabolic control.
Lifestyle Modifications for Improved Insulin Sensitivity
Lifestyle modifications play a pivotal role in improving insulin sensitivity and reducing hyperinsulinemia. These strategies are often the first line of defense and can significantly impact the overall management of the condition. A balanced diet rich in whole grains, fruits, vegetables, and lean protein, combined with regular physical activity, is fundamental.
- Dietary Modifications: A diet low in refined carbohydrates, processed foods, and saturated fats is crucial. Emphasizing whole foods, fiber-rich options, and mindful portion control can help regulate blood sugar levels and promote insulin sensitivity. Examples include incorporating more fruits, vegetables, and lean proteins while limiting sugary drinks, excessive red meat consumption, and foods high in unhealthy fats.
- Regular Physical Activity: Engaging in regular physical activity, including both aerobic and resistance training, enhances insulin sensitivity and promotes overall health. Aim for at least 150 minutes of moderate-intensity aerobic activity per week and incorporate strength training exercises at least two times a week. Regular exercise can significantly improve insulin sensitivity and help control blood sugar levels.
- Weight Management: Maintaining a healthy weight is crucial for improving insulin sensitivity. Weight loss, even modest amounts, can have a substantial impact on insulin resistance and hyperinsulinemia. Strategies like balanced nutrition and regular exercise can help achieve and maintain a healthy weight.
Pharmacological Interventions
Pharmacological interventions are often necessary to effectively address hyperinsulinemia and its associated complications when lifestyle modifications alone are insufficient. Different classes of medications target various aspects of insulin resistance and glucose metabolism.
- Metformin: Metformin is frequently prescribed as a first-line medication for type 2 diabetes. Its mechanism of action primarily involves reducing hepatic glucose production and improving insulin sensitivity in peripheral tissues. This helps lower blood sugar levels and potentially reduce hyperinsulinemia.
- Thiazolidinediones (TZDs): TZDs enhance insulin sensitivity in peripheral tissues by activating peroxisome proliferator-activated receptor gamma (PPAR-γ) receptors. This can lead to improved glucose control and a potential decrease in hyperinsulinemia.
- Sodium-glucose co-transporter 2 (SGLT2) inhibitors: SGLT2 inhibitors work by blocking the reabsorption of glucose in the kidneys, leading to increased glucose excretion in urine. This can help lower blood sugar levels and reduce insulin requirements, potentially contributing to a decrease in hyperinsulinemia.
Monitoring and Follow-up Care
Regular monitoring and follow-up care are essential components of managing hyperinsulinemia-associated type 2 diabetes. This involves ongoing assessment of blood glucose levels, glycosylated hemoglobin (HbA1c), and other relevant biomarkers.
- Regular Blood Glucose Monitoring: Frequent blood glucose monitoring allows for adjustments in medication dosages and lifestyle strategies as needed to maintain optimal blood glucose control.
- Glycosylated Hemoglobin (HbA1c) Testing: HbA1c reflects average blood glucose levels over a period of several months. Monitoring HbA1c provides a comprehensive picture of long-term glucose control and helps in evaluating the effectiveness of management strategies.
- Physician Follow-up: Regular appointments with a healthcare provider are critical for evaluating overall health, addressing any complications, and making necessary adjustments to the management plan.
Comparison of Pharmacological Interventions
| Drug Class | Mechanism of Action | Potential Benefits | Potential Side Effects |
|---|---|---|---|
| Metformin | Reduces hepatic glucose production, improves insulin sensitivity | Effective in lowering blood glucose, often well-tolerated | Gastrointestinal upset (e.g., diarrhea, nausea), vitamin B12 deficiency |
| Thiazolidinediones (TZDs) | Enhances insulin sensitivity in peripheral tissues | Improved glucose control, potential for weight loss | Fluid retention, weight gain, increased risk of heart failure, liver problems |
| SGLT2 Inhibitors | Increases glucose excretion in urine | Lowering blood glucose, blood pressure reduction, potential weight loss | Increased risk of urinary tract infections, genital mycotic infections, dehydration |
Illustrative Case Studies of Hyperinsulinemia and Type 2 Diabetes
Understanding the diverse ways hyperinsulinemia contributes to type 2 diabetes requires examining real-life examples. Case studies offer valuable insights into the development, diagnosis, and management of this condition, highlighting the impact of various interventions and the importance of early detection.These case studies demonstrate how hyperinsulinemia can manifest differently across various patient populations and underscore the significance of personalized approaches to care.
They also highlight the effectiveness of lifestyle modifications and pharmacological treatments in improving metabolic profiles and preventing long-term complications.
Case Study 1: Impact of Lifestyle Interventions
A 45-year-old female presented with a family history of type 2 diabetes and reported experiencing increasing fatigue and frequent urination. Initial blood tests revealed elevated fasting insulin levels and impaired glucose tolerance. She was advised to adopt a comprehensive lifestyle intervention plan focusing on dietary modifications and increased physical activity. This included a reduction in processed foods, refined sugars, and saturated fats, along with an increase in whole grains, fruits, vegetables, and lean protein sources.
A structured exercise program was also incorporated, aiming for at least 150 minutes of moderate-intensity aerobic activity per week. After six months, her fasting insulin levels decreased significantly, and her HbA1c levels fell within the normal range, demonstrating the positive impact of lifestyle changes in managing hyperinsulinemia-associated type 2 diabetes.
Case Study 2: Effectiveness of Pharmacological Therapies
A 62-year-old male with a history of hypertension and dyslipidemia presented with poorly controlled type 2 diabetes and persistently elevated insulin levels. Despite lifestyle interventions, his blood glucose and insulin levels remained uncontrolled. He was then prescribed metformin, a widely used oral antidiabetic medication, along with a statin to manage his dyslipidemia. The addition of metformin significantly reduced his insulin resistance, leading to improved glucose control and normalization of his insulin levels.
The combination of lifestyle modifications and pharmacological interventions resulted in a considerable improvement in his metabolic profile, demonstrating the effectiveness of a multi-pronged approach.
Case Study 3: Importance of Early Diagnosis
A 30-year-old male, experiencing symptoms such as increased thirst and frequent urination, initially attributed them to stress. However, he was encouraged to seek medical attention after his blood pressure readings and urine tests indicated elevated glucose and insulin levels. Early diagnosis and intervention allowed for prompt implementation of lifestyle interventions and medication adjustments. This case underscores the importance of recognizing early signs and symptoms of hyperinsulinemia and type 2 diabetes, enabling timely interventions to prevent the progression of the disease and associated complications.
Potential Complications of Hyperinsulinemia and Their Prevention
Hyperinsulinemia, if left unmanaged, can lead to a range of serious complications. The table below Artikels some of the potential complications, their descriptions, risk factors, and prevention strategies.
| Complication | Description | Risk Factors | Prevention Strategies |
|---|---|---|---|
| Cardiovascular Disease | Increased risk of heart disease, stroke, and high blood pressure. | High insulin levels, obesity, hypertension, dyslipidemia. | Maintain a healthy weight, regular exercise, a balanced diet low in saturated and trans fats, and control blood pressure and cholesterol levels. |
| Non-alcoholic Fatty Liver Disease (NAFLD) | Accumulation of fat in the liver, potentially leading to liver damage. | High insulin levels, obesity, metabolic syndrome. | Weight management, regular exercise, a healthy diet, and blood glucose control. |
| Polycystic Ovary Syndrome (PCOS) | Hormonal imbalance affecting reproductive health. | Insulin resistance, obesity. | Weight loss, regular exercise, and management of insulin resistance. |
| Sleep Apnea | Interruptions in breathing during sleep. | Obesity, high insulin levels. | Weight loss, regular exercise, and treatment of underlying conditions. |
Concluding Remarks: Hyperinsulinemia Is Associated With Type 2 Diabetes
In conclusion, hyperinsulinemia’s association with type 2 diabetes highlights the multifaceted nature of metabolic disorders. Early diagnosis, lifestyle interventions, and appropriate pharmacological approaches are crucial for managing this condition effectively. By understanding the underlying mechanisms and potential complications, we can empower individuals to make informed choices and improve their health outcomes.










