Immunotherapy for lung cancer is revolutionizing the fight against this deadly disease. It harnesses the body’s own immune system to target and destroy cancer cells, offering a promising alternative to traditional treatments. This guide explores the mechanisms, different types, clinical trials, combination therapies, patient selection, side effects, and future directions of this innovative approach.
Understanding the diverse types of lung cancer and how immunotherapy impacts them is crucial. This exploration delves into the varying responses based on genetic profiles, highlighting how personalized treatment strategies are emerging. We’ll also examine the efficacy of different immunotherapy types in clinical trials and research.
Introduction to Immunotherapy for Lung Cancer
Immunotherapy represents a revolutionary approach to treating lung cancer, shifting the focus from directly attacking tumor cells to harnessing the body’s own immune system to recognize and destroy them. This innovative strategy has shown remarkable promise in extending survival and improving quality of life for many patients. Unlike traditional chemotherapy, which targets rapidly dividing cells, immunotherapy specifically targets the molecular mechanisms that allow cancer cells to evade detection and destruction by the immune system.This approach has opened up new avenues for treatment, particularly for patients whose lung cancer is resistant to conventional therapies.
Understanding the fundamental mechanisms behind immunotherapy is crucial for comprehending its potential and limitations in the context of lung cancer management. This knowledge also allows for more informed decisions regarding treatment strategies and potential side effects.
Fundamental Mechanisms of Immunotherapy
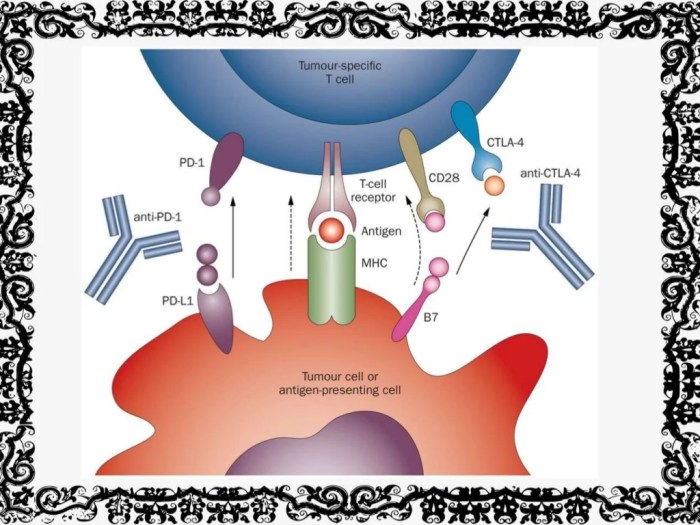
Immunotherapy works by stimulating or restoring the body’s immune response against cancer cells. Cancer cells often develop mechanisms to hide from the immune system. Immunotherapy disrupts these mechanisms, allowing immune cells like T cells to identify and attack the cancerous cells. Key mechanisms include activating immune cells, blocking inhibitory signals that prevent immune responses, and enhancing the ability of immune cells to recognize and kill tumor cells.
Types of Immunotherapy Approaches
Various approaches are employed in lung cancer immunotherapy, each targeting specific aspects of the immune response. These approaches are often combined to enhance their effectiveness.
- Checkpoint Inhibitors: These therapies target proteins on immune cells (like T cells) that normally prevent an immune response. By blocking these “checkpoints,” the immune system is encouraged to attack cancer cells more effectively. For example, blocking the PD-1/PD-L1 pathway is a common approach, as these proteins are often overexpressed in lung cancer cells, allowing them to evade immune detection.
- Immune Cell Therapies: These approaches involve directly modifying or enhancing the activity of immune cells to fight cancer. One example is chimeric antigen receptor (CAR) T-cell therapy, where T cells are genetically modified to recognize and attack specific proteins on cancer cells. This approach is still under development, but early results suggest it could be highly effective for certain types of lung cancer.
- Cancer Vaccines: These vaccines aim to stimulate an immune response against specific proteins expressed on cancer cells. By presenting these proteins to the immune system, the body learns to recognize and destroy cancer cells that carry them. This approach is still in the research and development stage for lung cancer, with some promising results for specific subtypes.
Efficacy Comparison of Immunotherapy Types, Immunotherapy for lung cancer
The following table provides a general overview of the efficacy of different immunotherapy types in lung cancer, acknowledging the complexities and variations in individual responses.
Immunotherapy for lung cancer is showing promising results, but alongside treatment, supporting your body’s natural defenses is key. Understanding the different types of magnesium, like whether it’s citrate, glycinate, or oxide, and how to choose the right one for your needs can be really helpful. This knowledge can aid in supporting the body’s response to immunotherapy, and potentially improving overall outcomes.
Learning more about the specifics of types of magnesium what they are and how to choose can offer valuable insights for anyone undergoing this treatment. Ultimately, the right approach to supporting your body throughout immunotherapy for lung cancer can be crucial for positive results.
| Immunotherapy Type | Mechanism of Action | Efficacy in Lung Cancer | Side Effects |
|---|---|---|---|
| Checkpoint Inhibitors (e.g., PD-1/PD-L1 inhibitors) | Block immune checkpoints, allowing immune cells to attack cancer cells. | Generally effective in specific subsets of lung cancer patients, particularly those with high PD-L1 expression. Can improve overall survival and response rates in certain cases. | Fatigue, skin rash, colitis, endocrine dysfunction, and immune-related adverse events (irAEs). |
| Immune Cell Therapies (e.g., CAR T-cell therapy) | Genetically modify immune cells to target cancer cells. | Showed promising results in early clinical trials, but still under development and not widely used in standard practice for lung cancer. | Potentially severe cytokine release syndrome and neurotoxicity. |
| Cancer Vaccines | Stimulate an immune response against specific tumor antigens. | Limited clinical use in lung cancer currently, with ongoing research and development to enhance efficacy and target specific lung cancer subtypes. | Potentially milder side effects compared to other types, but efficacy needs further investigation. |
Types of Lung Cancer and Immunotherapy
Immunotherapy, a revolutionary approach to cancer treatment, is showing promising results in battling lung cancer. However, the effectiveness of these therapies can vary significantly depending on the specific type of lung cancer. Understanding these nuances is crucial for tailoring treatment strategies and maximizing patient outcomes. This exploration delves into the relationship between lung cancer subtypes and immunotherapy responses.The landscape of lung cancer is diverse, encompassing various subtypes with differing biological characteristics.
These differences translate to varying responses to immunotherapy. Immunotherapy protocols are not one-size-fits-all; they must be tailored to the individual patient and their specific cancer type.
Non-Small Cell Lung Cancer (NSCLC) and Immunotherapy
NSCLC accounts for the vast majority of lung cancers. Its diverse genetic makeup leads to varied responses to immunotherapy. Key factors in determining immunotherapy effectiveness include the presence of specific mutations like EGFR or ALK, and the tumor’s expression of PD-L1. Targeted therapies alongside immunotherapy often enhance the response rates in specific genetic subtypes. For example, patients with EGFR-mutated NSCLC may benefit more from immunotherapy combined with EGFR-targeted inhibitors.
Small Cell Lung Cancer (SCLC) and Immunotherapy
SCLC, a more aggressive type of lung cancer, typically responds less favorably to immunotherapy compared to NSCLC. The biological characteristics of SCLC, including its rapid growth and tendency to metastasize early, pose unique challenges for immunotherapy. The role of immunotherapy in SCLC is often limited and primarily explored in combination with other therapies. While immunotherapy is not a primary treatment option for SCLC, it might play a supportive role in certain circumstances.
Genetic Profiles and Immunotherapy Response
Genetic testing plays a critical role in identifying the specific genetic alterations within a patient’s lung cancer. These alterations influence the tumor microenvironment and, consequently, the effectiveness of immunotherapy. Patients with tumors exhibiting high PD-L1 expression are more likely to respond favorably to checkpoint inhibitors, while those with other genetic profiles may require different immunotherapy approaches. For instance, a patient with a tumor harboring a BRAF mutation might not respond well to PD-1/PD-L1 inhibitors but might benefit from other immune-modulating strategies.
Tailoring Immunotherapy Protocols for Specific Subtypes
Immunotherapy protocols are carefully designed to match the unique characteristics of each lung cancer subtype. Clinicians utilize a multi-faceted approach that integrates genetic profiling, tumor biomarkers, and patient factors to determine the optimal treatment strategy. The use of biomarkers like PD-L1 expression levels helps predict which patients might respond well to checkpoint inhibitors, allowing for a more precise and effective treatment plan.
For example, a protocol might involve combining immunotherapy with chemotherapy or targeted therapy for specific genetic subtypes of NSCLC to enhance efficacy. Careful monitoring and adjustments to the immunotherapy regimen are crucial throughout the treatment course.
Clinical Trials and Research in Immunotherapy
Immunotherapy for lung cancer is an active and evolving field, with ongoing clinical trials playing a crucial role in refining treatment strategies and expanding treatment options. These trials explore novel approaches, assess existing therapies, and identify patient populations most likely to benefit from these innovative treatments. Understanding the current status of these trials provides insight into the future of immunotherapy in lung cancer.Research in immunotherapy for lung cancer is focused on enhancing the body’s natural defenses to combat the disease.
This involves various strategies, including checkpoint inhibitors, adoptive cell therapies, and cancer vaccines, each targeting specific mechanisms of tumor evasion or immune suppression. The goal is to improve treatment efficacy, reduce side effects, and tailor therapies to individual patient characteristics.
Current Status of Clinical Trials
Numerous clinical trials are investigating various immunotherapy approaches for lung cancer, exploring different combinations and targeting specific subtypes. Trials often focus on improving outcomes for patients with advanced or recurrent disease, who may have limited treatment options. The trials are meticulously designed to evaluate safety, efficacy, and tolerability of new therapies and strategies, ensuring data reliability and patient safety.
Latest Advancements and Breakthroughs
Significant advancements in immunotherapy research include the development of novel checkpoint inhibitors targeting specific immune checkpoints, such as LAG-3 and TIM-3, in addition to the well-established PD-1 and CTLA-4. These newer targets aim to further enhance the anti-tumor immune response and overcome resistance mechanisms. Combination therapies, which involve combining immunotherapy with chemotherapy, targeted therapies, or radiation, are also being extensively investigated, with some promising results showing synergistic effects.
Key Clinical Trials Focusing on Immunotherapy in Lung Cancer
Clinical trials are critical to evaluating the efficacy and safety of new immunotherapy approaches. The table below highlights some key clinical trials focused on immunotherapy in lung cancer, demonstrating the diversity of research being conducted.
| Trial Name | Phase | Focus Area | Status |
|---|---|---|---|
| Example Trial 1: Combination of Pembrolizumab and Chemotherapy in Advanced Non-Small Cell Lung Cancer | III | Evaluating the efficacy of combining a checkpoint inhibitor (Pembrolizumab) with chemotherapy in advanced non-small cell lung cancer (NSCLC). | Recruiting |
| Example Trial 2: Adoptive Cell Therapy using CAR T-cells in NSCLC | I/II | Assessing the safety and efficacy of adoptive cell therapy using engineered T-cells targeting specific NSCLC antigens. | Completed |
| Example Trial 3: Cancer Vaccine Targeting Specific Lung Cancer Mutations | I | Evaluating the safety and immunogenicity of a novel cancer vaccine designed to stimulate an immune response against specific mutations found in lung cancer cells. | Ongoing |
| Example Trial 4: Investigating the Role of Immunotherapy in Early-Stage NSCLC | II | Exploring whether immunotherapy can improve outcomes in early-stage NSCLC patients as an adjuvant treatment following surgery. | Recruiting |
Immunotherapy Combination Therapies
Combining immunotherapy with other cancer treatments is a promising approach to enhance the effectiveness of lung cancer treatment. This strategy aims to leverage the unique mechanisms of action of different therapies to create a more potent anti-tumor effect, potentially improving outcomes for patients. The synergistic effects of these combined therapies can significantly impact the body’s ability to fight cancer cells.The rationale behind combining immunotherapy with other cancer treatments is based on the idea that a multi-pronged attack can better target and eliminate cancer cells.
Immunotherapy can enhance the body’s natural defenses against cancer, while chemotherapy, radiation, or targeted therapies can directly damage or eliminate cancer cells. This approach can help improve response rates, prolong survival, and reduce the risk of recurrence.
Combination Therapies with Chemotherapy
Combining immunotherapy with chemotherapy can amplify the anti-tumor effects of both treatments. Chemotherapy drugs often induce cell death, creating a favorable microenvironment for immune cells to recognize and eliminate cancer cells. Immunotherapy can further enhance this process, stimulating a stronger and more sustained anti-tumor response. For example, the combination of immune checkpoint inhibitors with platinum-based chemotherapy has shown promising results in some lung cancer subtypes, leading to improved overall survival rates compared to either treatment alone.
Combination Therapies with Radiation Therapy
Combining immunotherapy with radiation therapy can improve tumor control and reduce the risk of recurrence. Radiation therapy can damage cancer cells, creating antigens that are recognized by the immune system. Immunotherapy can then enhance the immune response to these antigens, leading to improved tumor control and reduced recurrence rates. The combination of immunotherapy with radiation therapy may be particularly effective in treating localized lung cancer, improving outcomes in terms of local tumor control and preventing the spread of cancer.
Combination Therapies with Targeted Therapies
Combining immunotherapy with targeted therapies can be highly effective in certain lung cancer subtypes. Targeted therapies are designed to target specific genetic mutations or pathways involved in cancer cell growth and survival. Immunotherapy can amplify the effects of targeted therapies by increasing the activity of immune cells that recognize and eliminate cancer cells. For example, combining immunotherapy with targeted therapies that inhibit specific growth factors may be beneficial in lung cancers driven by EGFR mutations.
This combination approach could further improve tumor control and reduce the risk of resistance.
Recent advancements in immunotherapy for lung cancer are promising, but a healthy lifestyle plays a crucial role in supporting treatment. While exploring different dietary options, it’s important to consider if almond milk is a beneficial addition to your diet. For a comprehensive understanding of the nutritional value of almond milk, check out this helpful resource: is almond milk good for you.
Ultimately, a balanced diet, combined with the right medical care, can significantly improve outcomes for those undergoing immunotherapy for lung cancer.
Potential Combination Therapies and Their Outcomes (Table)
| Therapy 1 | Therapy 2 | Potential Synergistic Effects | Potential Adverse Effects |
|---|---|---|---|
| Immune checkpoint inhibitors (e.g., nivolumab) | Platinum-based chemotherapy (e.g., cisplatin) | Increased tumor response rate, improved overall survival, potentially reduced side effects compared to single treatments. | Increased risk of immune-related adverse events (e.g., colitis, pneumonitis), and standard chemotherapy-related side effects (e.g., nausea, fatigue). |
| Immune checkpoint inhibitors (e.g., pembrolizumab) | Radiation therapy | Enhanced tumor control, reduced recurrence rates, potentially improved local control in localized cancers. | Increased risk of radiation-related toxicity, and immune-related adverse events. |
| Immune checkpoint inhibitors (e.g., atezolizumab) | EGFR-targeted therapy (e.g., osimertinib) | Potentially improved tumor response rate, reduced resistance, increased survival in EGFR-mutated lung cancers. | Increased risk of both targeted therapy and immunotherapy side effects, potentially overlapping. |
Patient Selection and Response to Immunotherapy
Choosing the right patients for immunotherapy and understanding why some respond while others don’t is crucial for optimizing treatment outcomes. Precise patient selection, based on factors like tumor characteristics and the patient’s own immune system, directly impacts the success rate and minimizes potential side effects. This tailored approach is essential for maximizing the benefits of immunotherapy in lung cancer.The effectiveness of immunotherapy isn’t uniform across all patients with lung cancer.
Various factors influence a patient’s response, ranging from the specific type of lung cancer to their overall health and genetic makeup. Understanding these influencing factors and identifying potential biomarkers allows for more precise patient selection, potentially leading to improved treatment efficacy and reduced side effects.
Criteria for Selecting Patients
Identifying suitable candidates for immunotherapy involves a multifaceted evaluation process. This process considers various factors to ensure that patients most likely to benefit from the treatment are selected. Key factors include the type of lung cancer, the presence of specific genetic mutations, and the patient’s overall health status. Furthermore, factors such as the tumor’s immune microenvironment and the patient’s immune response are also crucial considerations.
- Tumor characteristics, including histological subtype and stage, are essential components in patient selection. For example, patients with non-small cell lung cancer (NSCLC) harboring specific mutations like EGFR or ALK mutations are often prioritized for immunotherapy. Similarly, patients with tumors displaying a higher degree of immune cell infiltration are more likely to respond to immunotherapy.
- Patient’s performance status and comorbidities are vital. Patients with a good performance status (e.g., able to perform daily activities) and fewer significant comorbidities are generally better candidates for immunotherapy.
- Tumor mutational burden (TMB) and microsatellite instability (MSI) are emerging biomarkers that play a role in determining a patient’s suitability for immunotherapy. High TMB and MSI tumors are often more responsive to checkpoint inhibitors. The presence of these markers can significantly influence the likelihood of a positive response to the treatment.
Factors Influencing Patient Response
Numerous factors influence how a patient responds to immunotherapy. These factors can be broadly categorized as tumor-related and patient-related characteristics. Understanding these influencing factors is vital for developing targeted treatment strategies.
- Tumor mutational burden (TMB): The higher the number of mutations in a tumor, the more likely it is to be recognized by the immune system, leading to a stronger anti-tumor response. This characteristic is directly associated with response to immune checkpoint inhibitors.
- Expression of immune checkpoint molecules: Tumors expressing high levels of immune checkpoint molecules, such as PD-L1, can be a sign of a stronger immune response. Patients with tumors displaying high PD-L1 expression are often considered strong candidates for immunotherapy with checkpoint inhibitors.
- Patient’s immune system: A patient’s immune system plays a pivotal role in determining the efficacy of immunotherapy. Patients with a robust and functional immune system are generally more likely to respond favorably to the treatment. Factors such as prior exposure to infections or vaccinations can also influence the immune response.
Predictive Biomarkers
Certain biomarkers can predict a patient’s likelihood of responding to immunotherapy. These biomarkers help oncologists tailor treatment strategies, increasing the chances of successful outcomes. A biomarker is a measurable indicator that can predict a patient’s response.
- PD-L1 expression: The presence and level of programmed death-ligand 1 (PD-L1) on tumor cells is a significant biomarker for predicting response to anti-PD-1 or anti-PD-L1 therapies. High PD-L1 expression is frequently associated with improved responses.
- Tumor mutational burden (TMB): A higher TMB suggests a greater likelihood of the immune system recognizing and attacking the tumor. This is particularly important in predicting response to checkpoint inhibitors.
- Expression of other immune checkpoint molecules: The presence and level of other immune checkpoint molecules, such as CTLA-4, can provide further insights into a patient’s response potential.
Monitoring Patient Response
Monitoring patient response to immunotherapy is crucial for adjusting treatment strategies and assessing the effectiveness of the therapy.
- Regular imaging studies (CT scans or PET scans) are used to track tumor shrinkage or growth. These scans allow clinicians to observe the impact of immunotherapy on tumor size and assess response rate. This data is used to evaluate the effectiveness of the treatment.
- Blood tests are employed to measure tumor markers and immune cell counts. These blood tests provide further insights into the tumor’s response to immunotherapy. Monitoring these biomarkers assists in determining the effectiveness of the treatment.
- Assessment of patient symptoms and quality of life is vital. Clinicians regularly assess the patient’s overall well-being and the impact of the therapy on their daily lives. This holistic approach ensures that the treatment is tailored to the individual needs of each patient.
Side Effects and Management of Immunotherapy: Immunotherapy For Lung Cancer

Immunotherapy for lung cancer, while offering hope for improved outcomes, can also bring about a range of side effects. Understanding these potential complications and the strategies for managing them is crucial for patients undergoing this treatment. Careful monitoring and proactive management are vital to maximizing treatment benefits while minimizing discomfort.
Common Side Effects
A variety of side effects can arise from immunotherapy, reflecting the body’s response to the treatment. These side effects can vary in severity and duration, and some may be manageable with appropriate medical intervention. It’s important to note that not all patients experience all side effects, and the severity of each effect can differ greatly between individuals.
Recent breakthroughs in immunotherapy for lung cancer are truly inspiring. While the focus is on innovative treatments, it’s also important to consider complementary approaches to overall well-being. For example, finding ways to naturally manage discomfort like bunions can significantly improve quality of life. Learning how to shrink bunions naturally could be a valuable step in that direction.
how to shrink bunions naturally This holistic approach, while not a cure, can contribute to a more comfortable experience for those undergoing lung cancer immunotherapy.
Immune-Related Adverse Events (irAEs)
Immunotherapy works by stimulating the immune system to fight cancer cells. However, this stimulation can sometimes trigger an overactive immune response, leading to immune-related adverse events (irAEs). These events can manifest in various organs and tissues, including the skin, lungs, and gastrointestinal tract. Examples of irAEs include skin rashes, colitis, and pneumonitis. The specific irAE and its severity will depend on the type of immunotherapy used and the patient’s individual characteristics.
Strategies for Managing Side Effects
Managing side effects is a critical component of immunotherapy treatment. Early detection and prompt intervention are key to minimizing discomfort and complications. A multidisciplinary approach, involving oncologists, immunologists, and other healthcare professionals, is often necessary. This approach allows for tailored strategies based on the specific side effect and its severity.
Table Summarizing Common Side Effects and Management Strategies
| Side Effect | Description | Management Strategies |
|---|---|---|
| Fatigue | A feeling of tiredness, weakness, and lack of energy. This can range from mild to debilitating and may significantly impact daily activities. | Rest periods, regular exercise (with physician approval), adjusting treatment schedules, nutritional counseling, and medications to address underlying causes. |
| Skin Rash | A localized or widespread skin reaction, ranging from mild redness to severe blistering and inflammation. | Topical creams or ointments, cool compresses, avoidance of harsh soaps and detergents, and potentially adjusting immunotherapy dosages or schedules. |
| Diarrhea | Frequent and loose bowel movements, often accompanied by abdominal cramps and discomfort. | Dietary modifications (low-fiber diet initially), antidiarrheal medications, and monitoring for dehydration. |
| Cough and Shortness of Breath | Symptoms that may indicate pneumonitis, an inflammation of the lungs. Can range from mild discomfort to severe respiratory distress. | Monitoring lung function, supplemental oxygen, corticosteroids to reduce inflammation, and possibly adjusting immunotherapy. |
| Nausea and Vomiting | Feeling of unease in the stomach, often accompanied by the urge to vomit. | Anti-emetic medications, dietary changes (small, frequent meals), and potential adjustment of treatment schedules. |
Future Directions and Challenges
Immunotherapy has revolutionized lung cancer treatment, but significant challenges remain. Further advancements hinge on understanding the complexities of the immune system’s response to tumors, and tailoring therapies to specific patient populations. This necessitates ongoing research and the development of innovative approaches to enhance efficacy and mitigate side effects.The journey towards personalized and more effective immunotherapy for lung cancer is marked by a need for precise targeting, overcoming resistance mechanisms, and addressing safety concerns.
Exploring novel combination therapies and improving patient selection criteria are key aspects in optimizing treatment outcomes.
Expanding the Scope of Immunotherapy Targets
The immune system’s intricate interplay with lung cancer cells is not fully understood. Identifying novel targets beyond the currently used checkpoints, such as PD-1 and CTLA-4, is crucial. This includes investigating alternative pathways involved in tumor evasion and immune suppression. Researchers are exploring the role of other immune cells, such as T regulatory cells (Tregs), and their interactions with tumor cells.
Improving Patient Selection and Response Prediction
Predicting patient response to immunotherapy remains a significant challenge. Developing robust biomarkers and diagnostic tools that can accurately identify patients most likely to benefit from immunotherapy is essential. These biomarkers could include genetic profiles, tumor mutational burden, and immune cell infiltration. Furthermore, understanding the mechanisms of resistance development will help tailor treatment strategies.
Overcoming Resistance Mechanisms
Tumor cells often develop resistance to immunotherapy, rendering therapies ineffective. Understanding the molecular mechanisms behind this resistance is crucial. This includes identifying the genetic and epigenetic changes that drive resistance and exploring strategies to overcome them. For instance, studies are investigating the role of specific mutations in the tumor genome and how they impact the immune response.
Exploring Novel Combination Therapies
Combining immunotherapy with other therapies, such as chemotherapy, targeted therapy, or radiation therapy, could significantly enhance treatment efficacy. Synergistic effects between these modalities could lead to improved tumor control and reduced side effects. This approach aims to maximize the benefits of immunotherapy while minimizing its potential drawbacks. Examples of synergistic combinations include combining checkpoint inhibitors with chemotherapy to enhance tumor cell killing and limit resistance.
Addressing and Mitigating Side Effects
Immunotherapy can induce a range of side effects, from mild fatigue to severe autoimmune reactions. Developing strategies to mitigate these side effects is crucial for patient well-being. This includes implementing supportive care protocols and exploring ways to minimize the intensity and duration of adverse events. Early detection and intervention for adverse events are critical to ensure patient safety and comfort.
Future Prospects of Immunotherapy in Lung Cancer
Despite the current challenges, the future of immunotherapy in lung cancer treatment is promising. Continued research and development efforts hold the potential to improve the efficacy and safety of existing therapies and to identify entirely new approaches. Personalized medicine approaches, incorporating patient-specific factors, will be crucial in tailoring treatments for optimal outcomes. This approach allows for targeted therapies that specifically address the unique characteristics of individual tumors, enhancing the likelihood of successful outcomes.
Final Review
In conclusion, immunotherapy for lung cancer represents a significant advancement in oncology. While challenges remain, ongoing research and clinical trials are paving the way for more effective and personalized treatment strategies. The future of immunotherapy holds immense promise, offering hope for improved outcomes and a better quality of life for patients facing this formidable disease. This guide has provided a comprehensive overview, but it’s crucial to consult with medical professionals for personalized advice.









