Knowing a pressure ulcer has begun demands immediate action. This comprehensive guide details the crucial steps to take when a pressure ulcer is suspected, from initial assessment to reporting protocols. Understanding the stages of pressure ulcer development, risk factors, and prevention strategies are essential for effective management.
This post will cover immediate actions, risk factors, documentation, treatment, long-term care, special considerations, and visual aids. We’ll explore the critical elements of accurate documentation, communication channels, and treatment options to ensure optimal healing and prevent further complications.
Immediate Actions
Pressure ulcers, also known as bedsores, are a serious complication that can arise from prolonged pressure on the skin. Prompt recognition and appropriate intervention are crucial for preventing further damage and promoting healing. This section details the immediate steps to take when a pressure ulcer is suspected or discovered.
Assessing a Suspected Pressure Ulcer
A systematic assessment is vital for accurately determining the extent and severity of a pressure ulcer. This involves a careful visual inspection, paying close attention to the characteristics of the affected area. Begin by evaluating the location, size, depth, and color of the lesion. Observe the surrounding skin for any signs of redness, inflammation, or breakdown. Assess for any signs of drainage or infection, such as pus, foul odor, or warmth.
Palpate the area to detect any tenderness, hardness, or fluctuance. These findings, combined with patient history and other clinical observations, help in determining the appropriate course of action.
Importance of Immediate Reporting and Escalation Protocols
Prompt reporting of a suspected or confirmed pressure ulcer is essential. This allows for immediate intervention and the involvement of healthcare professionals with expertise in wound care. A standardized reporting protocol should be followed to ensure consistent communication and efficient escalation of the issue. The protocol should clearly define the steps involved in reporting, the individuals to be notified, and the required information to be documented.
This facilitates rapid response and collaborative care. Failure to adhere to established protocols can lead to delays in treatment and potentially worsen the condition.
Documenting the Initial Observation of a Pressure Ulcer
Comprehensive documentation of the initial observation is crucial for tracking the progression of the pressure ulcer and evaluating the effectiveness of interventions. The documentation should include a detailed description of the pressure ulcer’s characteristics, including location, size, depth, and color. It should also include the date and time of the observation, the patient’s medical history, and any relevant factors contributing to the development of the pressure ulcer.
The documentation should be consistent with established hospital policies and procedures, ensuring accuracy, completeness, and clarity.
Stages of Pressure Ulcer Development and Immediate Actions
| Stage | Description | Immediate Actions |
|---|---|---|
| Stage 1 | Non-blanchable erythema of intact skin. Skin may appear reddened, but does not break down. A pressure-dependent area of skin reddens when pressure is applied, but the skin returns to normal when the pressure is released. | Reassess pressure points, re-position patient frequently. Document the observation. Report to the appropriate healthcare professional. Monitor for changes in skin color or texture. |
| Stage 2 | Partial-thickness skin loss involving epidermis and/or dermis. The wound bed may appear shallow with a red-pink wound bed, or a shallow open ulcer with a moist surface. The wound may be a blister or an abrasion. | Protect the wound, document the observation. Report to the appropriate healthcare professional. Assess for pain and infection. Consider using a dressing to prevent further damage. |
| Stage 3 | Full-thickness skin loss. Subcutaneous tissue may be visible. The wound may have a deep crater. | Protect the wound, document the observation. Report to the appropriate healthcare professional. Assess for pain and infection. Initiate wound care, as directed by a healthcare professional. |
| Stage 4 | Full-thickness tissue loss with exposed bone, tendon, or muscle. Extensive damage to the underlying tissues. | Protect the wound, document the observation. Report to the appropriate healthcare professional immediately. Assess for pain and infection. Initiate wound care, as directed by a healthcare professional. Surgical intervention may be required. |
Risk Factors and Prevention
Pressure ulcers, often called bedsores, are a serious complication that can develop when skin is subjected to prolonged pressure. Understanding the risk factors and implementing effective preventative measures are crucial in minimizing the risk and improving patient outcomes. Preventing pressure ulcers involves a multifaceted approach focusing on minimizing pressure, maintaining skin integrity, and promoting healthy circulation.Prolonged pressure on bony prominences, such as the heels, hips, and elbows, can lead to tissue damage and ulceration.
This damage is often exacerbated by factors like impaired mobility, poor nutrition, and decreased sensation. Early identification and intervention are essential to prevent these complications from progressing.
Risk Factors Contributing to Pressure Ulcer Development
Various factors increase the susceptibility to pressure ulcers. These factors can be categorized into modifiable and non-modifiable risk factors. Non-modifiable risk factors are inherent characteristics that cannot be changed, while modifiable factors can be addressed through interventions. Understanding these factors allows healthcare providers to tailor preventative strategies to individual patient needs.
- Non-Modifiable Risk Factors: These factors are inherent to the individual and cannot be altered. Examples include advanced age, decreased mobility, and medical conditions that affect circulation or sensation. Age-related changes in skin elasticity and blood flow are significant contributors to pressure ulcer development.
- Modifiable Risk Factors: These factors can be influenced and addressed to reduce the risk of pressure ulcers. Factors such as poor nutrition, incontinence, immobility, and inadequate hygiene are modifiable and can be addressed through interventions. Nutritional deficiencies, especially protein and calorie intake, significantly affect wound healing, increasing the risk of pressure ulcer formation.
Preventative Measures to Reduce Pressure Ulcer Risk
Effective preventative measures encompass a range of strategies aimed at minimizing pressure, promoting circulation, and maintaining skin integrity. A holistic approach that considers the individual patient’s needs and circumstances is critical.
- Pressure Reduction Strategies: Regular turning and repositioning are crucial for distributing pressure evenly across the body. Using specialized pressure-reducing surfaces, such as air mattresses or cushions, can further reduce the pressure on vulnerable areas. This approach is especially important for patients who are bedridden or have limited mobility.
- Maintaining Skin Integrity: Proper hygiene, including regular cleansing and moisturizing of the skin, is essential. Preventing moisture buildup, particularly in areas prone to friction or shear, is critical. Addressing incontinence promptly and using protective barriers to prevent skin maceration are vital.
- Promoting Circulation: Maintaining good circulation is essential for tissue health. This involves promoting movement, ensuring adequate blood flow, and addressing any underlying circulatory issues. Encouraging regular repositioning and appropriate positioning can improve blood flow.
Comparison of Preventative Strategies Across Patient Populations
The effectiveness of preventative strategies may vary depending on the specific characteristics of the patient population. Tailoring preventative measures to address the unique needs of different patient groups is essential.
| Patient Characteristics | Risk Factors for Pressure Ulcer Development | Preventative Strategies |
|---|---|---|
| Elderly patients with limited mobility | Decreased blood flow, decreased sensation, decreased muscle mass, increased susceptibility to pressure | Frequent repositioning, specialized pressure-reducing surfaces, regular skin assessment, nutritional support |
| Patients with spinal cord injuries | Immobility, decreased sensation, muscle atrophy, impaired circulation | Pressure relief devices, frequent turning, careful positioning, skin care, nutritional support |
| Patients with diabetes | Peripheral neuropathy, impaired circulation, delayed wound healing, decreased sensation | Frequent foot care, regular skin assessment, specialized footwear, meticulous wound care, blood glucose control |
Documentation and Communication
Accurate documentation and swift communication are crucial in managing pressure ulcers. Proper records allow for tracking progress, identifying trends, and evaluating the effectiveness of interventions. Effective communication ensures all relevant healthcare professionals are aware of the situation, facilitating coordinated care and preventing complications. This section will delve into the vital aspects of documentation and communication protocols for pressure ulcers.
Critical Elements of Accurate Documentation
Thorough documentation is essential for pressure ulcer management. It provides a detailed history of the ulcer’s progression, allowing for better treatment planning and evaluation of interventions. Key elements include the date and time of observation, the location and size of the ulcer, its depth and stage, any associated signs and symptoms, and details of the treatment plan. A consistent format for documentation aids in analysis and comparison across observations.
Spotting a pressure ulcer early is crucial. Knowing the signs is key, but sometimes understanding the why behind certain health issues can help too. For instance, chronic obstructive pulmonary disease (COPD) can lead to increased mucus production, impacting overall health and potentially making someone more susceptible to complications like pressure sores. Learning more about why COPD causes increased mucus production can help understand the complex factors at play.
why does copd cause increased mucus production Ultimately, recognizing the early signs of a pressure ulcer remains the best course of action for preventing further issues.
Visual aids like photographs, if possible, should be meticulously labeled with the date, time, and patient identifiers.
Required Communication Channels and Protocols
Prompt communication is critical to ensure the appropriate healthcare professionals are involved in the patient’s care. Communication protocols should be clear and concise, specifying the individuals who need to be informed, the information to be shared, and the method of communication. This ensures timely intervention and reduces the risk of complications.
Examples of Effective Documentation Templates
For consistent and thorough documentation, employing a standardized template is recommended. This helps streamline the process and ensures all relevant information is captured. A template should include patient demographics, date and time of observation, ulcer location, size, depth, stage, wound characteristics (e.g., color, exudate), and any associated pain or discomfort. The template should also document the treatment plan, any changes made, and the response to the treatment.
Furthermore, it should be clear whether the documentation is for initial assessment or follow-up observations.
Communication Pathways and Notification Protocols
Effective communication requires a clear understanding of who needs to be informed and how to reach them. A structured communication protocol streamlines the process, ensuring that relevant information is relayed promptly and accurately.
Recognizing a pressure ulcer is starting to form can be a real wake-up call, especially if you’re already dealing with health challenges. For example, conditions like trigeminal neuralgia and MS trigeminal neuralgia and ms can make everyday tasks difficult, potentially increasing the risk of pressure sores. Knowing the signs early is crucial for preventing further complications and ensuring proper treatment.
| Communication Pathway | Individuals to be Notified | Method of Communication |
|---|---|---|
| Initial Assessment | Nurse, Physician, Wound Care Specialist | Electronic health record (EHR), verbal report |
| Follow-up Observations | Nurse, Wound Care Specialist, Physician | EHR, progress notes, regular team meetings |
| Significant Changes | Nurse, Physician, Case Manager | EHR, phone call, urgent care consultation |
| Interdisciplinary Team Meetings | Nurse, Physician, Physical Therapist, Occupational Therapist, Social Worker | In-person meetings, conference calls, email |
Treatment and Management: Knowing A Pressure Ulcer Has Begun
Pressure ulcers, a serious concern for patients, require a multifaceted approach for effective treatment and management. A personalized plan is crucial, tailored to the individual’s specific needs and the stage of the ulcer. This necessitates a comprehensive understanding of the wound’s characteristics, the patient’s overall health, and their ability to participate in the treatment process.A proactive approach that focuses on preventing further tissue damage and promoting healing is vital.
Recognizing a pressure ulcer is starting to form can be tricky, but early detection is key. A nurse practitioner like julie scott anp bc can offer invaluable guidance on proper assessment and prevention strategies. Understanding the early signs, like skin that’s reddened or feels different, is crucial for timely intervention and avoiding more serious complications.
This involves a coordinated effort among healthcare professionals, caregivers, and the patient. Effective management requires a deep understanding of the factors contributing to the ulcer’s development, along with a commitment to consistent wound care and patient support.
Wound Care Management
Proper wound care is fundamental to the healing process. The goal is to create an environment conducive to the body’s natural healing mechanisms. This involves meticulous cleaning, debridement, and dressing changes, all aimed at removing necrotic tissue, promoting granulation tissue formation, and preventing infection. Careful attention to moisture balance is also essential, as excessive dryness or moisture can hinder healing.
Nutrition and Hydration
Adequate nutrition and hydration are vital for supporting the body’s healing response. A balanced diet rich in protein, vitamins, and minerals is crucial for tissue repair and overall health. Sufficient hydration ensures proper blood circulation and nutrient delivery to the wound bed. In cases of severe pressure ulcers, nutritional supplements or a modified diet may be necessary to meet the increased nutritional demands of the healing process.
A registered dietitian can help develop a personalized nutrition plan.
Wound Care Dressings
The selection of appropriate wound dressings is critical for effective wound care. Different dressings serve distinct purposes, depending on the characteristics of the wound and the desired outcome. A tailored approach ensures optimal healing and minimizes complications.
| Dressing Type | Description | Application |
|---|---|---|
| Hydrocolloids | These dressings form a gel-like layer that absorbs wound exudate and create a moist environment. | Suitable for wounds with moderate to heavy exudate, promoting autolytic debridement. |
| Hydrogels | These dressings are composed of a water-based gel that provides a moist wound environment. | Useful for wounds with minimal to moderate exudate, promoting healing and comfort. |
| Alginates | These dressings are derived from seaweed and have excellent absorbency, effectively absorbing exudate. | Ideal for wounds with heavy exudate, promoting a moist environment and effectively removing excess fluid. |
| Foam Dressings | These dressings provide cushioning and support for the wound bed, while absorbing exudate. | Suitable for wounds with moderate exudate, offering a protective barrier and comfort. |
| Films | These thin, transparent dressings create an occlusive environment, promoting a moist wound healing environment. | Ideal for wounds with minimal exudate, promoting a moist environment and protection from infection. |
Long-Term Care Considerations
Pressure ulcers, a serious complication affecting vulnerable populations in long-term care, demand proactive and ongoing management strategies. Preventing their recurrence and ensuring optimal healing are crucial for maintaining patient well-being and quality of life. Addressing the unique needs of these patients requires a multi-faceted approach that combines expert medical care with patient empowerment.Effective long-term pressure ulcer prevention hinges on a holistic understanding of the individual patient’s risk factors, combined with meticulous monitoring and responsive intervention.
This approach requires a shift from reactive treatment to proactive prevention and a strong emphasis on ongoing patient and caregiver education. Understanding the roles and responsibilities of the healthcare team is also paramount to coordinating efforts and achieving positive outcomes.
Strategies for Long-Term Pressure Ulcer Prevention
Preventing pressure ulcers in long-term care settings requires a multifaceted approach focusing on both environmental and patient-specific factors. Proactive measures aimed at reducing pressure and friction are essential. This includes utilizing specialized pressure-reducing surfaces, such as alternating pressure mattresses, and optimizing positioning techniques to distribute weight evenly. Regular repositioning, ideally every two hours, is critical.
Best Practices for Ongoing Wound Monitoring and Care, Knowing a pressure ulcer has begun
Maintaining a consistent and thorough monitoring process is essential for timely intervention and successful wound healing. This includes regular assessment of wound characteristics, including size, depth, exudate, and signs of infection. Accurate documentation, shared with the entire care team, is crucial for continuity of care and identifying trends. Visual inspection and palpation of the surrounding skin should also be performed to detect early signs of pressure or inflammation.
Implementing a standardized wound assessment protocol is essential to ensure consistent and reliable data collection.
Role of Patient Education in Promoting Self-Care and Healing
Empowering patients and their families with knowledge about pressure ulcer prevention and care is crucial for long-term success. Patient education should focus on practical strategies such as proper positioning, skin care, and recognizing early warning signs. Educating caregivers on proper techniques for repositioning and wound care is equally important. Demonstrating and practicing techniques will ensure effective implementation.
Table of Roles and Responsibilities in Long-Term Pressure Ulcer Management
| Healthcare Professional | Role & Responsibilities |
|---|---|
| Registered Nurse (RN) | Conducts regular wound assessments, develops individualized care plans, educates patients and caregivers, and communicates with the interdisciplinary team. |
| Physical Therapist (PT) | Evaluates patients’ mobility and functional limitations, develops exercise programs, and educates on proper positioning and pressure relief techniques. |
| Occupational Therapist (OT) | Assesses patients’ daily living skills and adapts the environment to promote independence and prevent pressure on bony prominences. |
| Wound Care Specialist/Registered Nurse | Provides specialized wound care, including dressing changes, debridement, and treatment of infections. |
| Physician/Medical Doctor | Diagnoses and prescribes treatment plans, oversees wound care, and consults with other healthcare professionals as needed. |
| Dietitian | Evaluates and addresses nutritional needs to support overall health and wound healing. |
Special Considerations
Pressure ulcer prevention and management require tailored approaches for diverse patient populations. Recognizing individual needs, such as mobility limitations, cognitive impairments, and neurological conditions, is crucial for effective care. Modifying care plans to address these specific needs ensures patient safety and optimal outcomes. Interprofessional collaboration is vital to comprehensively address the multifaceted challenges associated with pressure ulcer management.Individualized care plans are essential for patients with varying needs.
These plans must incorporate the specific challenges and vulnerabilities each patient faces, ultimately promoting healing and preventing further complications. This approach ensures optimal patient outcomes.
Pressure Ulcer Prevention in Patients with Mobility Limitations
Patients with limited mobility are at high risk for pressure ulcers due to prolonged pressure on bony prominences. Implementing strategies to minimize pressure and promote tissue perfusion is critical. These strategies may include frequent repositioning, specialized pressure-reducing surfaces, and the use of assistive devices. For example, a patient in a wheelchair may benefit from frequent repositioning every two hours, coupled with the use of a specialized wheelchair cushion.
Pressure Ulcer Prevention in Patients with Cognitive Impairments
Patients with cognitive impairments may not be able to communicate their discomfort or understand the importance of preventive measures. Consequently, caregivers must actively monitor these patients for signs of pressure and implement preventive strategies. Communication and education must be tailored to the individual’s level of understanding, using clear and simple language. Visual aids and demonstrations can be particularly helpful.
A patient with dementia, for instance, might benefit from visual cues reminding them to change positions regularly.
Pressure Ulcer Prevention in Patients with Neurological Conditions
Neurological conditions, such as stroke or spinal cord injury, can impair sensation and mobility, increasing the risk of pressure ulcers. Regular assessment for pressure areas, diligent repositioning, and the use of specialized pressure-reducing surfaces are vital. Furthermore, close monitoring of skin integrity and prompt intervention for any signs of breakdown are crucial. For instance, patients with spinal cord injuries often require frequent repositioning and the use of specialized mattresses to prevent pressure sores.
Interprofessional Collaboration
Effective pressure ulcer management relies heavily on collaboration among healthcare professionals. Nurses, physicians, physical therapists, occupational therapists, and other healthcare providers must work together to develop and implement comprehensive care plans. Open communication channels and shared decision-making processes are vital for coordinating care.
Unique Considerations for Pressure Ulcer Management in Various Patient Groups
| Patient Group | Unique Considerations |
|---|---|
| Patients with Mobility Limitations | Frequent repositioning, specialized pressure-reducing surfaces, assistive devices, and close monitoring. |
| Patients with Cognitive Impairments | Tailored communication, visual aids, clear instructions, and frequent caregiver education. |
| Patients with Neurological Conditions | Regular assessment for pressure areas, diligent repositioning, specialized pressure-reducing surfaces, and prompt intervention for skin breakdown. |
| Patients with Severe Obesity | Increased risk of pressure ulcer development due to increased weight distribution, requiring specialized pressure-reducing surfaces, and frequent repositioning, along with addressing underlying weight management issues. |
Visual Aids
Understanding pressure ulcers requires more than just knowing the definitions. Visual aids are crucial for recognizing the progression of these wounds, allowing for early detection and intervention. Early diagnosis is key to preventing serious complications.Visual representations of pressure ulcers provide a concrete understanding of the different stages and types. This helps healthcare professionals and caregivers identify the severity of the injury and plan appropriate treatment.
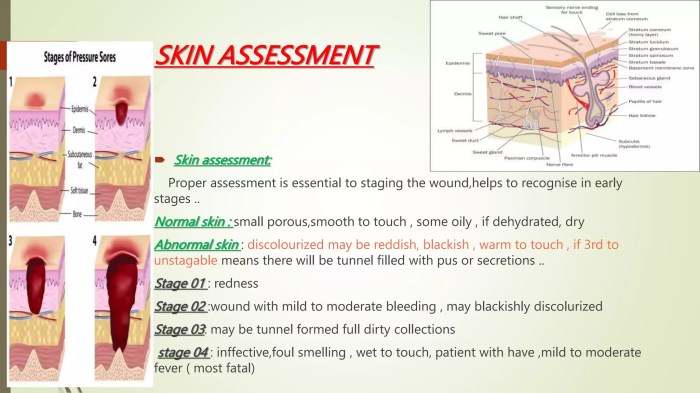
Early Stage Characteristics
Early-stage pressure ulcers are often characterized by subtle changes in skin color and texture. A reddened area that doesn’t blanch (turn pale when pressed) might be a first sign. The skin might feel warm to the touch in this area. In some cases, there might be a slight indentation or a feeling of hardness beneath the skin, though this isn’t always present.
These subtle changes are often missed, making early detection vital.
Progression of Pressure Ulcers
Pressure ulcers progress through several stages, each marked by escalating tissue damage. The initial reddening can deepen to a dark red, maroon, or purple hue. As the ulcer progresses, the skin may break down, forming an open sore. Blisters, drainage, and surrounding tissue damage become more apparent. The progression can vary depending on factors like the individual’s health, the location of the pressure, and the type of pressure applied.
Types of Pressure Ulcers
Pressure ulcers manifest in various forms, each with its own visual cues. A Stage I pressure ulcer is characterized by non-blanchable redness. A Stage II pressure ulcer shows partial-thickness skin loss. A Stage III pressure ulcer involves full-thickness tissue loss, with visible subcutaneous fat. Stage IV ulcers have exposed bone, tendon, or muscle.
Deep tissue injury is a different type of pressure ulcer, presenting as a localized area of discolored or intact skin with a persistent pain response.
Visual Representation Table
| Stage | Description/Appearance | Example |
|---|---|---|
| Stage I | Non-blanchable redness of intact skin. The area may appear warm or painful. | A localized area of redness over a bony prominence, such as the heel or sacrum, that doesn’t turn pale when pressed. |
| Stage II | Partial-thickness skin loss. The wound may appear as an abrasion, blister, or shallow crater. | A shallow open sore or blister on the heel, possibly with some drainage. |
| Stage III | Full-thickness skin loss. Subcutaneous fat may be visible. | A deeper wound extending into the subcutaneous tissue, potentially exposing some fat. |
| Stage IV | Full-thickness tissue loss with exposed bone, tendon, or muscle. | A deep wound that extends down to the underlying bone, tendon, or muscle. |
| Deep Tissue Injury | Localized area of discolored or intact skin with a persistent pain response. | A bluish or purplish area of skin that is painful, even when the skin is not broken. |
Final Wrap-Up
In conclusion, recognizing and responding to the early signs of a pressure ulcer is vital for successful treatment and prevention. By understanding the stages, risk factors, and appropriate actions, healthcare professionals and caregivers can significantly improve patient outcomes. The key to effective pressure ulcer management lies in swift, informed action and ongoing vigilance.









